Priscilla Pasc1,2, Ioana Alexandra Cote1, Mircea Ioachim Popescu1,2
1 Clinical County Emergency Hospital of Oradea, Romania
2 Faculty of Medicine and Farmacy of Oradea, University of Oradea, Romania
Abstract: Kounis syndrome (also known as acute allergic coronary syndrome) is defined as an acute coronary syndrome caused by an allergic reaction or a strong immune reaction to a drug or other substance. It is a rare syndrome with authentic cases reported to 130 men and 45 women until 2017. Anaphylaxis is rarely seen as an acute vasospastic coronary syndrome, the main pathophysiological mechanism being the release of cytokines and other infl ammatory mediators during a hypersen-sitivity reaction triggered by food, insect bites or drugs. In this article, we will present the case of an acute coronary syndro-me occurring in the context of the anaphylactic reaction triggered by the sting of several hornets- Vespa crabro from the family of the Hymenoptera. The diagnosis of Kounis syndrome was supported by electrocardiographic appearance and bio-chemical markers associated with clinical manifestations of acute coronary syndrome in the context of anaphylactic shock. Keywords: Kounis syndrome, acute allergic coronary syndrome, hornet stings
INTRODUCTION
Hymenoptera stings and subsequent allergic reacti-ons, including fatal anaphylaxis, are common causes of medical emergencies. Data from the literature suggest that systemic venom reactions occur in less than 5% of the cases, with severe allergic reactions being more frequent in Hymenoptera insect bites than from any other arthropod and may be the number one cause of worldwide deaths caused by insect venom. The most important Hymenoptera groups are: Apoidea (bees), Vespoidea (wasps) and Formicidae (ants). Reactions downgraded by the bites of these insects range from small or large local reactions to anaphylaxis and even death. Also, studies suggest that they can lead to mul-tisystemic damage, including intravascular haemolysis, rhabdomyolysis, thrombocytopenia, acute renal failu-re (ARF), liver failure, neuropsychiatric disorders and even cardiac arrest. Manifestations as myocardial in-farction and myocarditis are uncommon.
Acute coronary syndrome that accompanies activa-tion of mast cells from hypersensitivity or anaphylac-toid allergic reactions was fi rst described by Kounis and Zavras in 1991 and was referred to as „allergic angina” or „allergic myocardial infarction”. The Kounis syndrome mechanism (KS) involves the release of in-flammatory cytokines by activating mast cells, leading to vasospasm of the coronary artery and / or erosion or rupture of the atheromatous plaque. KS has been described in several situations, including exposures to a variety of natural or artificial allergens.
Vespa crabro is part of the Vespidae family, the Hy-menoptera order, and is the largest wasp in Europe and North America. Popular is called hornets or goo-seberries. It can cause multiple stings, because, unlike bees, it does not lose its needle after stinging. Its ve-nom contains a mixture of both toxic and allergenic substances responsible for triggering the hypersen-sitivity reaction. Reaction to the sting of this insect may be prolonged or severe in people with atopic predisposition, with manifestations such as urticaria, bronchospasm or circulatory collapse. Also, stings can precipitate an acute coronary syndrome by different pathophysiological mechanisms including direct action of venom constituents on coronary endothelium or allergic reaction with the release of mediators that act on coronary vascular muscles.It is requered to be ta-ken into consideration a possible allergic acute coro-nary sindrom every time a patient has an anaphylactic reaction triggered by hymenoptera bites, especially if the pacient has chest pain and haemodynamic di-sorders, even if these conditions occur rarely beca-use they require additional diagnosis and appropriate treatment.
CASE PRESENTATION
A 39-year-old patient, without a history of cardiovas-cular disease, shows up in the emergency department for systemic anaphylactic manifestations: respiratory (dyspnoea, polypnea, wheezing), subcutaneous and cutaneous (generalized erythema, pruritus, angioede-ma) and central nervous system reactions (the feeling of imminent death, irritability, restlessness). The pati-ent reports that the symptoms appeared shortly after being stung simultaneously by several hornets from the Hymenoptera family, objectively, showing small erythematous papula at the bitten skin area. Also, the patient complains of precordial pain with epigastric ir-radiation, which have been occurred shortly after the occurrence of anaphylactic manifestations.
The general objective examination reveals an altered general condition, signs of cutaneous ede-ma (face, extremities), three erythematous papules secondary to the sting, localized on the left laterally thorax, forearm and left arm. The targeted examina-tion of the cardiovascular system detects rhythmic heartbeats, without any heart murmurs detected and a blood pressure of 80/60 mmHg.
Electrocardiogram performed on arrival in the emergency room does not reveal any signifi cant chan-ges, but the one performed one hour after arrival in the emergency service records normal sinus rhythm, 64 heartbeats/minute, QRS axis at -45 degrees and a 2
mm ST segment elevation in DII, DIII, AVF (Figure 1). Repeated ECGs at 3, 6 and 10 hours show progressive ST segment resolution and the appearance after seve-ral days of negative T-waves in DIII, AVF (Figure 2).
Laboratory tests. In terms of biochemical deter-minations, the enzymes of myocardial necrosis, namely troponin I, are fastly determined. Initially unreacted, its values progressively increase to subsequent serial determinations (at 2 hours, 6 hours and 10 hours) (Table 1), with maximum value determined at 1.7 pg / ml ten hours after presentation.
Additional laboratory tests shows neutrophilic leukocytosis, slightly increased level of C-reactive protein (CRP), renal and hepatic samples within normal range (Table 2). The number of white blood cells de-creases progressively over the next days.
The Echocardiography reveals left ventricular aneurysm, a LVEF of 56% and mild mitral regurgitation (Figure 3,4). In evolution, the echographic aspect is stationary.
Coronary angiography. Based on the highly suggestive clinical picture of an acute coronary syndro-me, coronary angiography is performed urgently, re-vealing normal coronary angiography, without arterial plaques or other detectable anomalies (Figure 5,6). The medical treatment consisted in adrenaline 0.1 mg intramuscular injection (1: 1000 dilution), corti-costeroids (methylprednisolone), intravenous fluids (Ringer lactate) and bronchodilators (ventolin). Also, platelet antiaggregants are administered in the context of suspicion of acute cardiac ischaemia.
Symptomatology resolved within a few hours witho-ut repeating the cardiovascular symptoms during the admission period. Repeated paraclinical examinations (laboratory tests, ECG, echocardiography) followed the course mentioned above, revealing a signifi cant improvement over the course of a few days. The pati-ent was discharged from the hospital on the 5th day of the disease fully recovered, with the review plan after two weeks when the repeated investigations were in the normal range.
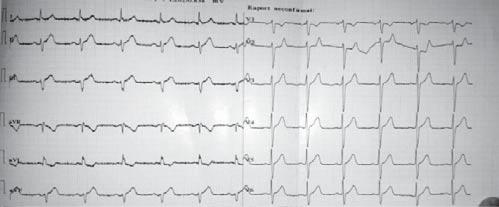
Figure 1. Electrocardiogram performed one hour after arrival in the emergency service.
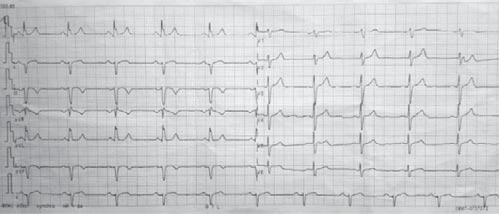
Figure 2. Electrocardiogram performed at discharge from hospital.
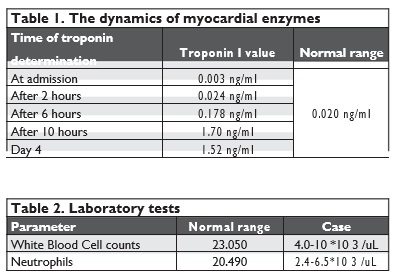

Figure 3. Echocardiography performed at the admission-parasternal long axis section.

Figure 4. Echocardiography performed at the admission- apical section.
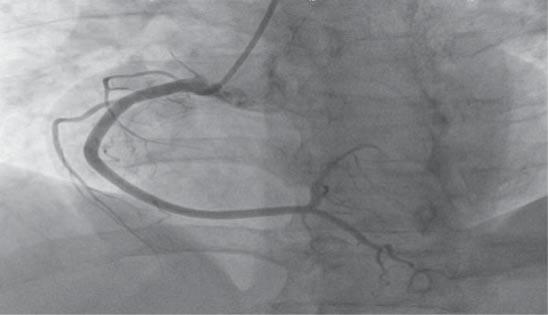
Figure 5. Right coronary artery.
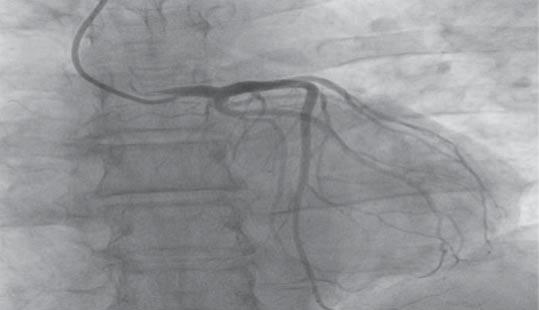
Figure 6. Left and circumflex coronary artery.
DISCUSSIONS
Corroborating the clinical and paraclinical manifesta-tions, the diagnosis of an acute coronary syndrome emerged in the context of an anaphylactic reaction caused by the sting of several hornets (Vespa crabro), from the Hymenoptera family. Precordial pain, electrocardiographic and enzymatic changes support the diagnosis. Rare cases have been described in the litera-ture, which is why the mechanism of myocardial invol-vement is unknown. Both the type I hypersensitivity pathway and the toxic direct effects of inoculated ve-nom during the sting can be incriminated. The compo-nents of the hymenoptera venom are various, mostly allergenic, such as phospholipase A2, hyaluronidase and melitin. Of these, phospholipase is the most po-tent allergen, triggering an IgE mediated immune res-ponse, and melitin, responsible for pain and inflamma-tion at the site of the sting, is an important component due to its ability to activate other poisonous proteins and its toxic potential. In addition, pharmacologically active constituents such as histamine, serotonin, do-pamine, noradrenaline and a bradykinin-like substan-ce that can induce histamine release have been isola-ted from the venom. The sequence of events in the triggered hypersensitivity reaction culminates with the release of serotonin and histamine with vasodilatory effect and formation of leukotrienes with a strong va-soconstrictor effect. At the cardiovascular level, these mediators can precipitate coronary artery spasm and accelerate the breakdown of coronary artery arterial plaques. In addition, all these substances can aggravate myocardial ischaemia either by the hypotension se-condary to vasodilation or by increasing myocardial oxygen demand by direct ionotropic or chronotropic effect, in the presence of a compromised blood supply of the myocardium.
There are three variants of Kounis syndrome. The Type I variant includes patients with normal coronary arteries without predisposing factors for coronary ar-tery disease, which evolves with coronary spasm but with normal myocardial necrosis enzymes, or with prolonged spasm that evolves to myocardial infarcti-on. This variant could be a manifestation of endothelial dysfunction or microvascular angina. Type II includes patients with preexisting atheromatous disease, whe-re the acute allergic episode may induce erosion or rupture of the plaque that manifests as an acute myo-cardial infarction. A type III variant was described as a coincidence of hypersensitivity reactions after implan-tation of drug-eluting stents, causing stent thrombosis. The case of the 39-year-old patien,t with no cardio-vascular risk factors and no history of angina episodes, belongs to type I Kounis syndrome with electrocar-diographic changes and elevated myocardial necrosis enzymes. The electrocardiographic aspect of ST seg-ment elevation in inferior derivation with its progressive reduction to the isoelectric line and the subsequent development of negative T-waves are highly suggestive for myocardial ischemia. Also, the rise in troponin I dynamics to significant values for myocardial necrosis, supports the diagnosis. Emergency coronary angiogra-phy does not reveal significant lesions, but this does not rule out the possibility of transient myocardial is-chaemia, most likely due to coronary spasm. Other in-vestigations, such as perfusion myocardial scintigraphy or cardiac magnetic resonance imaging, would have been of great use to the case.
The case presented further supports for Kounis syndrome as a distinct phenomenon. Some authors have argued that the vasospastic process is the domi-nant pathophysiological explanation of Kounis syndro-me, advocating systemic vasodilation and coronary hypoperfusion as the main mechanism in myocardial ischemia in the context of anaphylaxis. However, diffe-rentiation of primary myocardial injury from mast cell activation by global myocardial hypoperfusion may be challenging and remains a potential alternative expla-nation for acute coronary artery syndrome.
Another hypothesis of myocardial infarction in the anaphylactic reaction suggests that treatment with epi-nephrine frequently used in the emergency room for anaphylactic reactions may be responsible for myocar-dial injury. Epinephrine is considered the cornerstone in managing anaphylaxis. Intramuscular administration of adrenaline 1: 1000 at a maximum dose of 0.5 mg is recommended for the treatment of anaphylaxis. The mechanism of myocardial lesion would be coronary vasospasm secondary to administering epinephrine. The case described was also treated with adrenali-ne intramuscularly, but at a small and single dose of 0.1 mg. Knowing the pharmacokinetics and its very short half-life (5-10 minutes), coronary vasospasm is less likely to occur as a secondary to adrenaline ad-ministration, since angina symptoms occurred before adrenaline administration and electrocardiographic and enzymatic anomalies occurred two hours after administration. However, the possibility of worsening of coronary spasm after administration of epinephrine is not excluded.
CONCLUSIONS
Diagnosis and treatment of Kounis syndrome can be really challenging, requiring concomitant attenti-on to both cardiac and anaphylactic pathophysiology. Although allergic episodes are common in everyday practice, early recognition of Kounis syndrome caused by the stings of the hymenoptera hornets is important for the therapeutic conduct and choice of the optimal treatment. Further studies are needed in the future to understand the allergic mechanisms involved in acu-te coronary syndromes pathogenesis and to pave the way for effective therapeutic interventions.
Conflict of interest: none declared.
References
1. Fassio F1, Almerigogna F. Kounis syndrome (allergic acute coronary syndrome): different views in allergologic and cardiologic literature. Intern Emerg Med. 2012 Dec;7(6):489-95
2. M Triggiani, V Patella. Allergy and the cardiovascular system.Clin Exp Immunol. 2008 Sep; 153(Suppl 1): 7-11.
3. Capurro N, Levi R.The heart as a target organ in systemic allergic re-actions: comparison of cardiac analphylaxis in vivo and in vitro. Circ Res. 1975 Apr;36(4):520-8.
4. Sarfaraz Memon, MD, Lovely Chhabra, Allergic acute coronary syn-drome (Kounis syndrome). Proc (Bayl Univ Med Cent). 2015 Jul; 28(3): 358-362.
5. Dissanayake Mudiyanselage Priyantha Udaya Kumara Ralapanawa, A case of Kounis syndrome after a hornet sting and literature review,. BMC Research Notes December 2014, 7:867
6. W. D. Jayamali,H. M. M. T. B. Herath. Myocardial infarction during anaphylaxis in a young healthy male with normal coronary arteries- is epinephrine the culprit?. BMC Cardiovasc Disord. 2017; 17: 237
 This work is licensed under a
This work is licensed under a