Roxana Siliște1, Mara Jidveian2, Raluca Ianula1, Dan Spătaru1
1 Cardiology and Internal Medicine Department, Coltea Clinical Hospital, Bucharest; U.M.F ”Carol Davila”
2 Oncology Department, Coltea Clinical Hospital, Bucharest
Contact address:
Roxana Siliște, MD
Cardiology and Internal Medicine Department, Coltea Clinical Hospital, Bucharest; U.M.F ”Carol Davila”
We present a case of a 54 years old male, referred to our clinic for exertional dyspnea, from the Oncology Department. He was diagnosed one year before with right upper lobe lung cancer. He underwent right upper lobectomy, lymph node dissection and right pulmonary artery resection. The histopathologic exam showed poorly differentiated squamous cell carcinoma (SCC). He received four cycles of chemotherapy (Paclitaxel/CBDCA). After six month of chemotherapy, an upper polar left renal tumor was found on abdominal CT scan. He underwent a left nephrectomy. The histopathologic exam confirmed a SCC metastasis from the lung cancer. He started a new chemotherapy scheme with Docetaxel 75 mg/mp.
Six months later he was addressed to our clinic for evaluation. He complains of progressively installed exertional dyspnea, atypical chest pain and weight loss. On physical examination we found normal vital signs, no cardiomegaly, no heart murmur, no pulmonary crackles, no edema. Laboratory tests showed mild leukocytosis, inflammatory syndrome, and high values of NTproBNP (5300 ng/dl). CK, CKMB and troponin were in normal range. The resting ECG revealed sinus tachycardia and minor RBBB. The chest X-ray showed normal cardiothoracic index, a small nodular lesion in the right lower lobe, ascended right hemidiaphragm and right pleural adhesion (Figure 1). The echocardiography showed normal valves, no dilation of cavities, normal left ventricular (LV) systolic function with an estimated EF of 60%, mild pulmonary hypertension (sPAP= 40 mmHg) and a small pericardial effusion. In the parasternal view we noticed in the basal segment of the LV posterior wall a large intramyocardial mass (2,7/4,63 m). The mass had a different echogenicity compared to normal myocardium (Figure 2A, 2B, 2C). Another mass, with the same echogenicity, could be seen between left atrium (LA) and aorta (AO) (Figure 3A, B). We have also seen a small mobile mass attached to the LA roof (corresponding to above mentioned mass, as well as spontaneous contrast into the LA (Figure 3A, B). The thoracic CT scan showed a large intrapericardial mass (5,4/3,8 cm) with intimate contact with right pulmonary artery, aorta, left atrium, right atrium and superior right pulmonary veins (Figure 4A). Another hypodense lesion (4,4/3,2 cm) was seen into the myocardium of the postero-inferior LV wall (Figure 4B). The patient received anticoagulants, betablockers and a new chemotherapy scheme (Gemcitabine/Carboplatine). He survived only six month after the diagnosis of intramyocardial and intrapericardial metastasis.
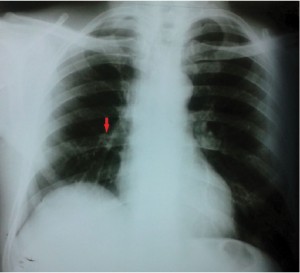
Figure 1. Chest X ray shows a small nodular lesions in the right lower lobe (red arrow), ascended right hemidiaphragm and right pleural adhesion.

Figure 2. Echocardiography: parasternal long axis view (2A, 2B) and parasternal short axis view (2C) shows a large intramyocardial mass (red arrow).
(LV= left ventricle, Ao = aorta, RV = right ventricle, LA = left atrium).
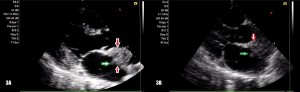
Figure 3. Echocardiography: a left atrium optimized parasternal long axis view shows a mass between aorta (AO) and left atrium (LA) (between red arrows) and a small mobile mass in the LA. (green arrow).
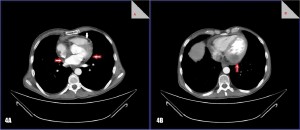
Figure 4. CT scan.
4A – A pericardial mass (between red arrows), pericardial effusion (white arrow)
4B – An intramyocardical hypodense mass.
Conflict of interest: none declared.
 This work is licensed under a
This work is licensed under a