Alexandru Ioan Deaconu1,3, Silvia Iancovici1, Alexandrina Nastasa1, Alexandra Acostachioae4, Diana Zamfir1, Tudor Constantinescu2,3, Claudia Toma2,3, Dragos Zaharia2,3, Miron Bogdan2,3, Maria Dorobantu1,3
1 Department of Cardiology, Clinical Emergency Hospital, Bucharest, Romania
2 ”Marius Nasta” Institute of Pneumology, Bucharest, Romania
3 4th Clinical Department – Cardio-Thoracic Pathology, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania
4 “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania
Abstract: Objectives – We set to evaluate the potential utility of right ventricle (RV) Tei-index as a prognostic parameter in patients with pulmonary arterial hypertension (PAH). We investigated its correlation with the clinical status, current treatment, a series of paraclinical parameters, as well as established determinants of prognosis in patients with PAH. Methods – We enrolled in our study 24 patients with PAH confirmed by right heart catheterization (RHC) over a period of 4 years (2012-2016). We performed complete transthoracic echocardiography and six minute walk distance in all subjects. Results – The RV TEI index correlated with the World Health Organization functional class (WHO FC) (p=0.05) and right atrial pressure determined by RHC (p=0.01). Patients undergoing diuretic treatment had a statistically significant lower TEI Index (p=0.017). There was also a trend of association between treatment with bosentan and a lower TEI index (p=0.0727). Conclusions – In PAH patients, the RV TEI Index correlates with clinical parameters (WHO FC, 6MWD) and hemodynamic variables (right atrial pressure). RV TEI Index could improve under treatment with diuretics and possibly bosentan in these patients.
Keywords: pulmonary arterial hypertension, TEI index
Rezumat: Obiective – Ne-am propus să evaluăm utilitatea indexului TEI al ventricului drept (VD) ca parametru prognostic la pacienţi cu hipertensiune arterială pulmonară (HTAP). Am investigat posibile corelaţii cu statusul clinic, tratamentul urmat, o serie de parametri paraclinici şi elemente de prognostic utilizate curent în evaluarea pacienţilor cu HTAP. Metode – Am inrolat în studiu 24 de pacienţi cu HTAP confirmată prin cateterism cardiac drept, într-un interval de timp de 4 ani (2012-2016). Pacienţilor li s-a efectuat ecocardiografie transtoracică completă, cateterism cardiac drept şi test de mers de 6 minute. Rezultate – Indexul TEI al VD s-a corelat cu clasa funcţională OMS (p=0.05) şi cu presiunea în atriul drept (PAD) determinată la cateterism cardiac (p=0.01). Pacienţii aflaţi în tratament cu diuretic au avut valori ale indexului TEI al VD semnificativ statistic mai reduse (p=0.017). De asemenea, există o trendinţă de asociere între tratamentul cu bosentan şi reducerea indexului Tei al VD (p=0.072). Concluzii – La pacienţii cu HTAP, indexul TEI al VD se corelează cu parametrii clinici (clasa funcţională OMS, testul de mers de 6 minute) şi variabile hemodinamice (PAD). La aceşti pacienţi indexul TEI al VD se poate ameliora sub tratament cu diuretice şi posibil bosentan.
Cuvinte cheie: hipertensiune arterială pulmonară, indicele TEI
INTRODUCTION
Pulmonary arterial hypertension (PAH) is a rare but life-threatening disease. PAH is defined as an increase in pulmonary arterial pressure ≥25 mmHg as assesed by right heart catheterization (RHC) associated with a pulmonary artery wedge pressure (PAWP) ≤15 mmHg and a pulmonary vascular resistance (PVR) >3 Wood units in the absence of other causes of precapillary PH1.
Echocardiography is currently the most useful method of screening and monitorization for patients diagnosed with PAH, regardless of whether they are undergoing treatment or not. In this category of patients, right ventricular function is a major determinant of effort capacity and clinical evolution. Echocardiography is also a non-invazive method for establishing the causes and consequences of elevated pulmonary artery pressures2. The measured parameters include estimation of pulmonary artery sistolic pressure (sPAP), right ventricle (RV) to right atrium (RA) gradient, RV areas and fractional area change (FAC), tricuspid annular plane systolic excursion (TAPSE), and RV Tei-index. Current guidelines acknowledge measurement of RA aria and the presence of pericardial effusion as echocardiographic prognostic markers in PAH1. The TEI index also known as the RIMP is a global estimate of both systolic and diastolic function of the RV and it is based on the relationship between ejection and nonejection work of the RV3.
OBJECTIVE
We sought to evaluate the potential utility of RV TEIindex as a prognostic parameter in patients with PAH. We investigated its correlation with the clinical status, current treatment, a series of paraclinical parameters, as well as established determinants of prognosis in patients with PAH.
MATERIAL AND METHOD
We enrolled in our study 24 patients with PAH confirmed by right heart catheterization (RHC) over a period of 4 years (2012-2016). Patients were referred to our cardiology ward from the “Marius Nasta” Institute of Pneumology, and were all included in the National Program for Arterial Pulmonary Hypertension Management. Mean age of the study group was 53.5 +/14.7 years, range 26-82 years, with 29 % women.
All subjects underwent complete transthoracic echocardiography using a Vivid 7 system within maxi-mum 6 months before or after the RHC (medium interval 2 months). We measured TAPSE, R A, R V, S wave, acceleration time (AT), mean pulmonary artery pressure (mPAP), right ventricle to right atrium pressure gradient, right ventricle ejection fraction, pulmonary artery systolic pressure (sPAP), E wave, A wave, E/E’, inferior vena cava dimension and TEI index, all according to the current guidelines for RV echocardiographic evaluation3.
Thus, the TEI index was defined as the ratio of isovolumic time (IVT) divided by ejection time (ET), or [(isovolumic contraction time (IVCT) + isovolumic relaxation time (IVRT))/ET].
Spectral Doppler recordings of CW of the tricuspid regurgitation jet in order to measure the interval “a” between the start and end of trans tricuspid flow (Figure 1), and PW of right ventricular outflow in order to measure interval “b”, the right ventricular ejection time (Figure 2).
Intervals a and b are used to calculate myocardial performance index (MPI) for the right and left ventricle as per the formula: MPI = (a – b)/b.
bpm = beats/min; CW = continuous-wave Doppler; HR = heart rate; PW = pulsed-wave Doppler.
In order to measure the isovolumic time and ejection time, the formula is using 2 time intervals a and b as shown in the figures 1 and 2, isovolumic time = a-b and ejection time = b. The interval a includes the IVCT, the ejection time (ET) and the IVRT, and the TEI index may also be expressed by the formula a-b/b. For the evaluation of the right ventricular (RV) TEI index the a interval, from the end to the start of trans-tricuspid flow (the interval from the end of the A wave to the start of the E wave), is obtained from the apical 4-chamber view with the Doppler sample volume located betwe-en the tips of the tricuspid valve leaflets.
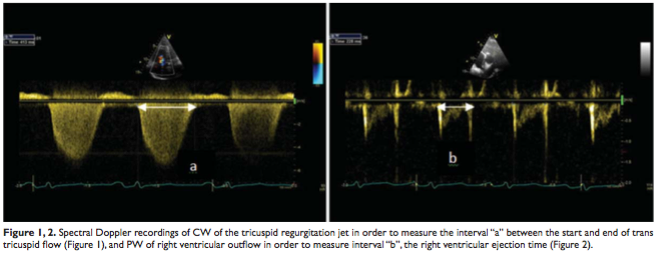
The b interval (right ventricular ejection time) is measured from the parasternal long-axis view, with the sample volume located just below the pulmonary valve.
The upper reference limit used for the right-sided MPI is 0.40 using the pulsed Doppler method, according to current recommendations1.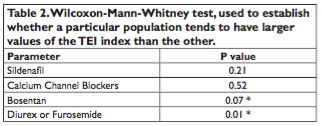
Tricuspid regurgitation (TR) was functional in all patients in terms of mechanism and was evaluated by means of quantitative (PISA measurements), qualitative (tricuspid valve morphology, color flow TR jet) and semi-quantitative parameters (vena contracta width, hepatic vein flow).
All patients underwent a six-minute walk distance (6MWD) test within 6 months before or after the RHC. The 6MWD test was performed by a trained pneumologist on a 20 m corridor with no prior practice walks in accordance with the American Thoracic Society guidelines4. The World Health Organization (WHO) functional class (FC) was determined in accordance with current PAH guidelines1.
RESULTS
Mean TEI index was 0.652 +/-0.356. TR was moderate in 22 patients and severe in 2 patients. Mean distance in the 6MWD was 440 m (range 200 m – 700 m). Mean RA volume was 90.8 mL (range 39 – 205 mL). Clinically, 1 patient presented in WHO FC I, 6 patients inWHO FC II,16 inWHO FC III and 1 inWHO FC IV. Mean right atrial pressure (RAP) was 7 mmHg (range 1-14 mmHg).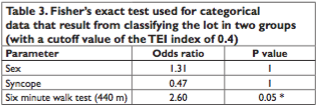
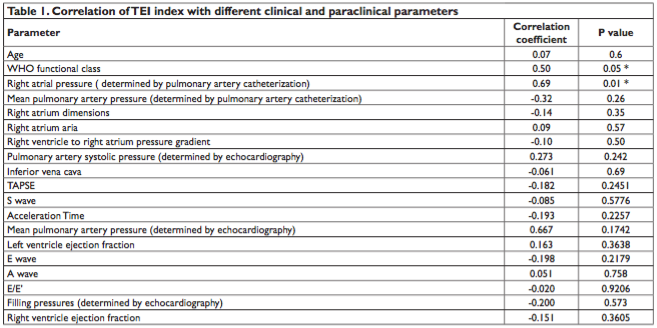
The TEI index correlated with WHO FC and RAP determined by RHC, but not with other echocardiographic markers of RV function, such as TAPSE, RV ejection fraction or right cavities dimensions (Table 1).
Possible implications of the different treatments for PAH on the value of TEI index were also investigated (Table 2). Patients undergoing diuretic treatment had a statistically significant lower TEI Index (p=0.017). There was also a trend of association between treatment with Bosentan and a lower TEI index (p=0.0727).
When considering TEI index as normal when <0.4 and high when >0.4, a correlation was documented between normal TEI index and longer than 440 m dis-tances at the six minute walk test (odds ratio = 2.6, p=0.059).
DISCUSSION
The most relevant findings of our study were: (1) the TEI index correlated with clinical parameters used in the assessment of PAH severity such as WHO FC and 6MWD; (2) the TEI Index was associated strongly with diuretic treatment and had a trend towards association with Bosentan treatment; (3) the TEI Index correlated strongly with RA pressure determined invasively.
Several studies tested the utility of RV TEI index in the evaluation of RV function and as a marker of adverse outcome in patients with pulmonary hypertension5-7. The advantages of using the TEI Index are that it avoids the geometric assumptions and limitations of complex RV geometry3.
The WHO FC class, despite its interobserver variability, remains one of the most powerful predictors of survival, as a worsening FC class is one of the most alarming markers of disease progression1. The correlation between the TEI index and the WHO class (p=0.052) supports the potential of the TEI index as an indicator of RV function and overall prognosis.
The TEI index also correlated with the 6MWD. This strengthens the association between the TEI index and clinical parameters assessing the severity of the disease. In our study group the correlation was present at a threshold of the 6MWD of 440 m. Consequently, patients with a TEI index >0.4 had a odds ratio of 2.602 (borderline statistical significance, p=0.059) for a shorter than 440 m walking distance and conversely, patients with a TEI index < 0.4 were associated with longer than 440 m 6MWD. For the lower threshold used in the PAH guidelines, 165 m, there was no statistical correlation with the TEI index due to the very small number of patients in our group that were in this category of the 6MWD.
A surprising finding is the lack of correlation among the TEI index and other echocardiographic parameters used in the global assessment of RV function, such as: RV EF, TAPSE or S wave. This comes in contradiction with previous studies, such as the one conducted by For fi a et al. which reported that TAPSE strongly reflects RV function and prognosis in PAH.
Regarding the association between TEI Index and hemodynamic variables, Dyer et al. and Ogihara et al demonstrated that RV Tei-index correlated with mean PAP6 as well as pulmonary vascular resistance (PVR)7. In our study, the TEI index correlated with the right atrial pressure (p=0.0178), but no other associations with hemodynamic measurements were possible. This correlation contradicts the assumption formulated by other studies3, namely that TEI index measurement is unreliable when RA pressure is elevated.
Another finding of our study was that TEI Index was strongly associated with diuretic treatment, being lower in patients on furosemide or furosemide/spironolactone (p=0.017) compared to patients without diuretic treatment. These findings are similar to previous results3, leading to the conclusion that the RV TEI index is in part preload-dependent. Since our study was observational, no evaluation was performed before versus after diuretic therapy in the same patient.
STUDY LIMITATIONS
The relatively long timespan (6 months) from the right heart catheterization to the moment of the echocardiography and clinical assessment (WHO FC, 6MWD) in some patients is one of the main limitations of our study. Patients in atrial fibrillation were excluded from the study as differing R-R intervals make TEI Index measurement unreliable. Absence of long-term followup and the relatively small patients group represent other limitations.
CONCLUSION
In PAH patients, the RV TEI Index correlates with clinical parameters (WHO FC, 6MWD) and hemodynamic variables (right atrial pressure). RV TEI Index could improve under treatment with diuretics and possibly Bosentan in these patients. The strong association with the clinical status of the patient warrants further studies to confirm the potential of the RV TEI Index as a prognostic parameter in patients with PAH.
Conflict of interest: none declared.
References:
1. Galiè N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, Simonneau G, Peacock A, Vonk Noordegraaf A, Beghetti M, Ghofrani A, Gomez Sanchez MA, Hansmann G, Klepetko W, Lancellotti P, Matucci M, McDonagh T, Pierard LA, Trindade PT, Zompatori M, Hoeper M, Aboyans V, Vaz Carneiro A, Achenbach S, Agewall S, Allanore Y, Asteggiano R, Paolo Badano L, Albert Barberà J, Bouvaist H, Bueno H, Byrne RA, Carerj S, Castro G, Erol Ç, Falk V, Funck-Brentano C, Gorenflo M, Granton J, Iung B, Kiely DG, Kirchhof P, Kjellstrom B, Landmesser U, Lekakis J, Lionis C, Lip GY, Orfanos SE, Park MH, Piepoli MF, Ponikowski P, Revel MP, Rigau D, Rosenkranz S, Völler H, Luis Zamorano J. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J. 2015;46(4):903-975.
2. Popescu BA, Ginghina C. Ecocardiografia Doppler. In: Bogdan Alexandru Popescu, Carmen Ginghină, eds. Ecocardiografia Doppler. Vol 1. 1st ed. Bucharest: Editura Medicală; 2011:273-298. doi:616.12-008.3073:534.321.9.
3. Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB. Guidelines for the Echocardiographic Assessment of the Right Heart in Adults: A Report from the American Society of Echocardiography Endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 2010;23:685-713.
4. ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002;166:111–7.
5. Forfia PR, Fisher MR, Mathai SC, Housten-Harris T, Hemnes AR, Borlaug BA, Chamera E, Corretti MC, Champion HC, Abraham TP, Girgis RE, Hassoun PM. Tricuspid annular displacement predicts survival in pulmonary hypertension. Am J Respir Crit Care Med 2006; 174:1034–41.
6. Dyer KL, Pauliks LB, Das B, Shandas R, Ivy D, Shaffer EM, Valdes-Cruz LM. Use of myocardial performance index in pediatric patients with idiopathic pulmonary arterial hypertension. J Am Soc Echocardiogr 2006;19:21–7.
7. Ogihara Y, Yamada N, Dohi K, Matsuda A, Tsuji A, Ota S, Ishikura K, Nakamura M, Ito M. Utility of right ventricular Tei-index for assessing disease severity and determining response to treatment in patients with pulmonary arterial hypertension. J Cardiol. 2014 Feb;63(2):14953.
 This work is licensed under a
This work is licensed under a