Daniel Gherasim1, Bianca Moise2, Eduard Apetrei1,3
1 “Prof.Dr.C.C.Iliescu” Emergency Institute for Cardiovascular Disease, Bucharest
2 Sanador Hospital, Bucharest
3 “Carol Davila” University of Medicine and Pharmacy, Cardiology Department, Bucharest
Contact address:
Dr. Daniel Gherasim, Clinical Cardiology, “Prof. Dr. C.C. Iliescu” Emergency Institute for Cardiovascular Disease, Bucharest, Sos. Fundeni 258, Sector 2, Bucharest, Zip code 022328
E-mail: gherasimdanro@yahoo.com
Abstract: Exercise testing (ET) is a well-established, safe an cost-effectiveness procedure which is widely used in clinical practice for many decades for detection of coronary artery disease (CAD). The mean test sensitivity and specificity are not very high and are lower than the values for the most expensive imaging procedures mentioned in the current guidelines for stable CAD. Modern ET is not limited to the observation of ST segments abnormalities, important information can be obtained from exercise capacity, which is the most important predictor of mortality, heart rate and blood pressure response and/or development of arrhythmias , during the exercise, but also in the recovery period. Some prognostic scores including ET variables were developed for increase the predictive value of ET. Worldwide, the decrease in cardiovascular mortality was possible through a better management of risk factors, but also through development of new revascularization therapies, devices and antiischaemic agents. Restenosis continue to be the major limitation of coronary revascularization and patients after coronary revascularization could be identified as being at high risk for future cardiac events. New generations of stents with lower rate of restenosis are developed and the trend of research in this field is a dynamic one. There are only few studies examining the utility of exercise testing after percutaneous coronary intervention (PCI) or coronary artery bypass graft surgery (CABG). There is no consensus regarding the use of exercise testing after PCI or (CABG). There are divergent opinions regarding the use of ET post PCI as a routine strategies or functional (symptom-driven) strategies. Angina post-PCI is an insensitive marker of restenosis, as between 25% to 50% of patients have cardiac ischemia that is clinically silent. Recurence of symptoms may occur in 10 to 20 percent of patients after stent implantation; the rate for stent restenosis is 30-40% following balloon angioplasty and 20-30% after stenting with bare metal stents, and <10% with drug-eluting stents. For better evaluation of the risk of restenosis and/or progression of native CAD, less commonly used ECG criteria could be useful in the exercise electrocardiography (ECG) changes analysis. To summarize, exercise testing is very useful in the detection of ischemia in postrevascularization patients, despite some inherent limitations which alter also the accuracy of the test for the initial evaluation of suspected CAD. The post-revascularization patients are high risk patients who need to be carefully evaluated early, but also late after the revascularization procedure and the ET, especially in centers with a good expertise, is the first option in noninvasive evaluation of this growing group of patients.
Keywords: exercise stress testing, predictive value, percutaneous coronary interventions (PCI), coronary artery bypass graft surgery (CABG).
Rezumat: Testul de efort reprezintă o metodă utilă, sigură şi cu un bun raport cost/eficienţă, fiind utilizat de mult timp şi pe scară largă în practica clinică pentru diagnosticul bolii ischemice coronariene. Sensibilitatea şi specificitatea testului de efort nu sunt foarte înalte, dacă ar fi să le comparăm cu sensibilitatea şi specificitatea raportate pentru tehnicile imagistice, mai scumpe, aşa cum sunt trecute în ghidurile curente. În prezent, interpretarea testului de efort nu se limitează doar la modificările segmentului ST, ci şi la alte date cum ar fi capacitatea de efort, cel mai important predictor de mortalitate, răspunsul frecvenţei cardiace şi a tensiunii arteriale, ca şi prezenţa aritmiilor, atât în faza de exerciţiu propriu-zis, cât şi în faza de recuperare sau revenire. De asemenea, au fost dezvoltate scoruri de risc pe baza datelor obţinute la testarea de efort, tocmai pentru creşterea valorii predictive a testului. Scăderea, la nivel global, a mortalităţii prin boli cardiovasculare a fost posibilă printr-un mai bun control şi tratament al factorilor de risc, dar şi prin dezvoltarea unor noi tehnici de revascularizare şi a medicaţiei antiischemice. Restenoza rămâne principala limitare pentru orice modalitate de revascularizare, pacienţii coronarieni, postrevascularizaţie, putând fi încadraţi ca având un risc crescut pentru evenimente cardiace. Au apărut noi generaţii de stenturi cu rate scăzute pentru restenoză şi cercetările în acest domeniu continuă. Au fost publicate puţine studii care evaluează utilitatea testului de efort după revascularizaţie, fie ea intervenţională sau chirurgicală şi nici nu există un consens privind testul de efort la pacienţi după revascularizare. Opiniile sunt împărţite privind efectuarea testului de efort, de rutină sau doar în cazul apariţiei simptomelor. Trebuie spus că angina nu poate reprezenta un marker sensibil pentru restenoză, din moment ce în 25 până la 50 % din cazuri, ischemia este silenţioasă. Recurenţa simptomelor poate apare în 10-20% din cazuri după stentare, iar rata restenozei este apreciată la 30-40% după angioplastie cu balon, la 20-30% după stent metalic şi la <10% din cazuri după stent activ. Pentru o mai bună evaluare a riscului de restenoză sau/şi progresia bolii ischemice, au fost analizate criterii electrocardiografice (ECG) mai puţin utilizate şi care ar putea fi utile în interpretarea modificărilor ECG. În concluzie, testul de efort este deosebit de util în depistarea ischemiei, în ciuda limitărilor cunoscute şi care influenţează acurateţea testului şi atunci când îl folosim ca evaluare iniţială, în scop diagnostic. Pacienţii după revascularizare sunt pacienţi la risc înalt şi trebuie atent monitorizaţi, atât precoce, dar şi la distanţă după efectuarea procedurii, testul de efort fiind prima opţiune în evaluarea noninvazivă a acestor pacienţi, mai ales în centrele cu o bună experienţă în domeniul testării de efort.
Cuvinte cheie: test de efort, valoare predictivă, angioplastie, revascularizaţie chirurgicală.
Introduction
Cardiovascular diseases (CVD) remains the main cause of death, accounting for 4 million deaths per year in Europe or 40% of all deaths in EU countries1,2. Coronary heart disease only, accounts for almost 1.8 milion deaths, or 20% of all deaths in Europe annually, with Baltic countries and central and eastern European countries having the highest mortality rates. Mortality rates for ischemic heart disease are higher for men then for women in all countries, with 70% on average higher in men in EU member states. In our country the IHD mortality rates per 100 000 population were 287 for women and 425 for men (Source: 2011.Eurostat Statistics Database)2.The economic implications are huge for the health care budget and for that, identification of patients at high risk of adverse events is crucial.
The exercise stress test is used in the evaluation of symptomatic patients to predict the presence and extent of coronary artery disease (CAD) and remains, despite a not very high sensitivity reported in old studies, the most widely accessible and relatively inexpensive method for initial evaluation of suspected coronary artery disease. From a meta-analysis of 147 studies, the standard exercise electrocardiographic cut-point of 0,1 mV of horizontal or down sloping ST segment depression selected as discriminating cut-point for ischemia, has a mean sensitivity of 68% and a mean specificity of 77% for the detection of CAD. In a retrospective case series of 404 patients from our center, we found a higher predictive value for exercise testing; the sensitivity of the test was 85.3% and the specificity 46.8%, the positive predictive value was 65.3% and the negative predictive value was 73.1% (paper under press).
Dynamic changes in the prevalence and treatment of cardiovascular risk factors in the modern era or in the treatment of stable coronary artery disease or acute coronary syndromes have produced changes in the prevalence of CAD and CVD mortality and also changes in the inducible ischemia during stress tests3.
The ECG exercise test (ET) has a class I indication for the diagnosis of obstructive CAD, but the predictive value of ET post coronary revascularization is still a issue for debating4.
In the last decades, some controversial ECG criteria have been analyzed in the attempt to increase the sensitivity of the test: heart adjustment of ST depression, P wave prolongation, U wave changes, transient axis shifts or duration or amplitudes of QRS complex, QT interval and T-wave subintervals. An important issue, beside the identification of obstructive disease, is the prediction of future coronary events and mortality by the ET. Methods demonstrated the prognostic value include evaluation of exercise capacity, which is considered the most important prognostic marker obtained by exercise test, chronotopic competence and incompetence, peak exercise blood pressure response, heart rate recovery and frequent ventricular ectopy during recovery, and also exercise test scores, which incorporate clinical and demographic risk factors4-6.
A. Exercise testing after PCI
The use of percutaneous coronary interventions (PCI) for treatment of CAD has dramatically increase in the last three decades. The first coronary artery bypass grafting (CABG) was performed 50 years ago, in 1964, in the same period when the first report of one of the most used test in clinical cardiology, the Bruce protocol exercise treadmill test, was published7,8. Thirteen years later the first PCI was performed, becoming during the last decades, one of the most frequently performed therapeutic interventions in medicine. In 1993 the first bare-metal coronary stent was developed and approved for the USA market, and in 2002 the drug-eluting stents (DES) were approved for the European market. Nowadays the stents are currently used in >80% of PCI procedures and the trend of researches for better quality devices is a very dynamic one.
There are three major questions to be solved regarding the ET post PCI: 1) the optimal period to perform the ET (the timing of ET); 2) the value of ECG and hemodynamic responses; 3) the predictive value for different strategies of revascularization.
1. When we will perform an exercise test after revascularisation?
Restenosis remain a major and probable single limitation of PCI and reflect complex pathophysiology processes. Clinical events after balloon percutaneous transluminal coronary angioplasty (PTCA) are attributable to arterial renarrowing at the PTCA site, intimal hyperplasia in the area of coronary stenting, progression of atherosclerotic disease at remote sites, or a combination of these events. Angiographic and clinical restenosis are generally developing within 6 to 9 months after PTCA and major cardiac events, including death or myocardial infarction, and progression of atherosclerosis occurring as a low, but constant risk (1-2% risk per year) indefinitely after the procedure. The risk of restenosis after PTCA depends on clinical factors, such as diabetes mellitus or prior restenosis, anatomical factors such as total oclusions or smaller vessel size, and procedural factors, such as the final minimal lumen diameter.
The accuracy of ET for detection of restenosis, as for the diagnosis of CAD, depends of the moment when the test will be applied in the continuum of cardiovascular disease, as shown in Figure 1.
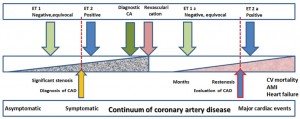
Figure 1. The accuracy value of exercise testing is correlated with the severity of CAD and the moment when we apply the test in continuum of coronary artery disease. The cut-point used for abnormal ST-depresion could coincide with the apearence of significant stenosis. Earlier we performe the test, better will be the prognosis, either for suspected CAD or for already knew CAD. ET=exercise testing; CA=coronary angiography. ET1 and ET 1a=tests performed in a moment when the lesions are minimal; ET 2 and ET 2a=tests performed when the lesions are clinical and/or hemodynamic significants.
Recurrence of symptoms may occur in 10 to 20 percent of patients after stent implantation; the rate for stent restenosis is 30-40% following balloon angioplasty and 20-30% after stenting with bare metal stents, and <10% with drug-eluting stents, but recurrent rates were reported in some studies being even higher, up to 80%. depending on vessel size or type of restenosis. (intrastent, marginal, remote disease9.
2. The ET is still using in the modern era of cardiology ?
Despite a modest reduction in stress testing rates after PCI from 59.3 per 100 person-year in 2006 to 47.1 per 100 person-year in 2008, the rate of ECG ET post PTCA compared with exercise test with imaging increased slighty over time, an increase which is significant after adjustement10.
3. Sensitivity of ET for the prediction of restenosis
A meta-analysis showed that ET has a poor sensitivity (46%) and a moderate specificity (77%), for the identification of post-PCI restenosis. Comparing with ET, stress echocardiography and nuclear imaging had a better sensitivity (63% and 87%, respectively) and specificity (87%, and 78%, respectively), but the studies which were analysed were published between 1975 and 200011. A lot of changes in the paterns of risk factors, and therapies occurred since than. There are only few data about the predictive value of ET nowdays.
The ET for the detection of restenosis or new lesion has a sensitivity of 61%, specificity of 63%, a PPV of 67%, and a NPV of 57%, in a study on 66 males who had performed an ET before and 6 months after procedure12.
4. Routine versus functional strategies
It is unclear if a routine early ET strategy is predictive of clinical events or not. There are few studies in which the conclusions favor the early post PCI strategy, but the majority of observational studies does not support the role of ET early after PCI.
Angina post-PCI is an insensitive marker of restenosis, as between 25% to 50% of patients have cardiac ischemia that is clinically silent13,14. The exercise test performed in our laboratory of a female patient which had developed asymptomatic restenosis is presented in Figure 2.
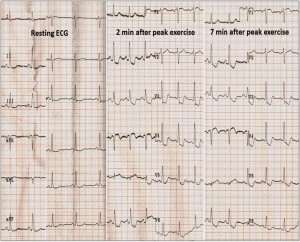
Figure 2. Routine exercise testing in a 62 year old female with diabetes and dyslipidemia, 3 months after balloon percutaneous transluminal coronary angioplasty (PTCA) and bare metal stent (BMS) implantation on proximal LAD, revealed silent ischemia (important downsloping ST depression in leads II, III, aVF, V3-V6 and ST elevation in aVR, ST abnormalities which had persisted 10 minutes in recovery period) due to restenosis, angiographicaly confirmed.
In a post-hoc analysis of the subgroup of patients that underwent ET 6 weeks following the PCI (the routine arm) in the ADORE trial (Aggressive Diagnosis of Restenosis), the authors found that early ET was poorly predictive of clinical events, with a positive predictive value of 21.9%. The sensitivity was 41.2%, the specificity was 73,3%, and the negative predictive value was 87.5 %.The ADORE trial compared a strategy of routine functional testing with a selective, symptom –driven strategy, clinical follow-up being at 9 months. The poor sensitivity could be related to the low probability to find a significant restenosis prior to 6 weeks following PCI, and also to the low sensitivity of ET for the detection of one-vessel disease compared with multi-vessel CAD. A subgroup of patients with diabetes randomized to routine FT had a higher composite clinical event rate than those randomized to the selective strategy, but the procedural rates did not differ significantly15.
In the second ADORE trial (ADORE II), the same ET strategies were compared, but this time in high risk patients: diabetes, multivessel disease, left ventricular ejection fraction <35%, and/or PCI of the proximal left anterior descending artery. The quality of live (QOL) and functional status were assessed also. More positive tests were observed at 6 months compared with 1.5 months evaluation (almost double).The incidences of cardiac procedures and clinical events were not significantly different at nine-up follow up, but routine exercise endurance was improved in the routine arm, without significant improvement of the QOL16.
In the Routine versus Selective Exercise Treadmill Test after Angioplasty (ROSETTA) Registry, the investigators found that was five-fold difference in the intensity of functional testing between patients who underwent the routine and selective testing strategies, in 791 patients from 13 centers in 5 countries. The routine functional testing was not associated with an increase in the use of cardiac procedures, but was associated with a reduction in cardiac events, including unstable angina (6.1% versus 14.4%; p = 0.001), myocardial infarction (0.4% versus 1.6%; p = NS), death (0% versus 2.2%; p = 0.02) and composite clinical events (6.3% versus 16.3%) during 6 month follow-up, as shown in Figure 3. The patients enrolled in the routine arm were more likely to receive two or more anti-anginal medications (57% versus 43%, respectively; p = 0.0002). The difference clinical events could be attributable to the early identification and treatment of patients at risk for follow-up events, the major benefit of routine strategy being reassurance for patients and physicians. One of the conclusion was, therefore, that despite a previous founded low sensitivity and specificity in the post PCI setting, the routine use of exercise electrocardiography alone, could improve outcomes17.
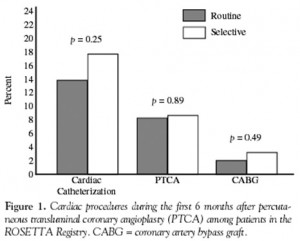
Figure 3A. Cardiac procedures during the first 6 months after percutaneous transluminal coronary angioplasty (PTCA) among patients in the ROSETTA Registry. CABG=coronary artery bypass graft.
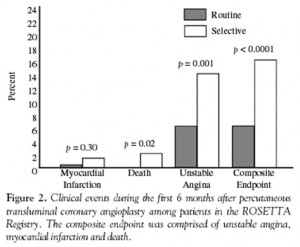
Figure 3B. Clinical events during the first 6 months after percutaneous coronary angioplasty among patients in the ROSETTA Registry. The composite endpoint was comprised of unstable angina, myocardial infarction and death. From ref. 17,with permission from HMP Communications.
5. ECG changes
The exercise test ussualy is performed for the detection of CAD, using an discriminatory cut-point of 0,1 mV of horizontal or downsloping depression, and without antiischemic therapy, the result being positive, negative, inconclusive or equivocal. Post PCI, when we already know the CAD is present, the test must be performed with medication, including, for example, beta-adrenergic blockade agents, and for this reason the criteria of submaximal heart rate can’t be used for the definition of test as maximal or submaximal. Revised formulas for determination of age-predicted maximal heart have been proposed, eg. maximal heart rate = 164-0/72 x age18. The main criteria will be exercise capacity, estimated from exercise time or measured during a cardiopulmonary exercise testing. There are no divergent opinions concerning the cut-off point for ischemia, which will be the same (0,1 mV), but the ST depression don’t have the same prognostic value in patients with different therapeutic strategies for revascularization. In the DANAMI-2 (the second DANish trial in AMI) study, the ST depression was more frequent and was an independent risk predictor in patients treated with fibrilolysis, but not in the PCI group. Exercise capacity was the most powerful prognostic predictor for death and re-infarction for every treatment strategy, an increasing with one metabolic equivalent of the task (MET) being correlated with a 20% decrease of death and reinfarction19.
For purpose of early detection of restenosis, we have looking for another criteria to increase sensitivity of ET, ST segment changes <0,1 mV being not very uncommon. A number of facts must be taken into account: resting ECG showing Q waves or intraventricular conduction abnormality, incomplete revascularization, the relative common ST depression observed predominantly within 2 weeks or even later, without remaining significant stenosis, especially in patients with diabetes or hypertension. The ET can’t differentiate between restenosis and a new lesion, but the general agreement is that the main purpose for ET in patients post PCI is the detection of restenosis.
6. Compare the results of ET before and after PCI
One of the strategy which can help us is to perform an ET before the PCI and another ET after PCI, and to compare the ECG territories where ST changes have occurred. ST-segment changes observed in other leads after angioplasty compared with the preangioplasty exercise test may show a false-positive result, during an ET performed 3 months after angioplasty20. Also, an increase in exercise capacity after PCI was correlated with coronary luminal enlargement achieved with angioplasty, and decrease of exercise capacity was correlated with luminal reduction and restenosis, when the ET and angiograms obtained 2 weeks before and 20 weeks after PCI were compared21.
One interesting observation is that the rate of false positive tests in the first month after PCI is higher in patients with DES implantation, probably due to a more proeminent endothelial dysfunction, even DES are associated with a reduced rate of restenosis, compared with bare metal stents22. Concernings were formulated about the plaque instability and the safety of ET in the first 24-48 hours, beside his utility short after PCI. A Swiss study showed us that early ET first day after coronary bare-metal stenting is safe (the number of patients with stent thrombosis was the same in active and control group) and offer important prognostic information about mortality, trend toward repeat revascularization and risk for major adverse cardiac events, all of them being at higher level in patients with positive ET, especially in combination with incomplete revascularization, which was defined as stenosis >50%23.
In a small study (29 patients), Milo M et al.24 have demonstrated a lower coronary blood flow response to adenosine assessed by transthoracic Doppler echocardiography in patients with ST segment response ≥1 mm to exercise in serial ET during a follow-up of 6 months, ST segment changes being related to the presence of coronary microvascular dysfunction (CMVD) in the above mentioned period. The utility of ET early (within 2 weeks) only for detection of ischemia is debatable25.
7. Unconventionaly ECG criteria
Not validated criteria for detection of ischemia, some ECG findings marked as controversial or less commonly used, seems to have a better sensitivity in the prediction of restenosis.
The sum of ST depression (ΣΔST index) of leads II, III, aVF, V4-V6 reported to heart rate index (ΔHR) was 13.7 in the restenosis group and 9.3 in the patent group (p=0.017) in a study with patients receiving PCI to treat acute coronary syndrome (ACS). The sensitivity, specificity, positive predictive value, and negative predictive value of this index were 85%, 63%, 44%, and 92%26. Also, the increase of ST/HR index from one test to another, performed in a period from 3 months to 12 months after PCI, showed o very high sensitivity, of 91% and a specificity of 77%, with a positive predictive value of 70% and negative predictive value of 94%27.
The ST changes in recovery phase in relation to heart rate, represented as rate-recovery loop, has been found to be more specific for the identification of restenosis then ST depression alone. In patients with ischemia, the loop has an counterclockwise aspect, different from what we find in normal patients where a clockwise rate-recovery loop is recorded6.
Using ST depression, heart rate and rate-recovery loop, Lehtinin et al.28 developed ST /HR hysteresis which exceed the simplest ST/HR index or ST segment depression for the detection of ischemia, but the method need to be incorporated in computer-based algorithms.
The addition of right precordial leads V3R through V5R or the calculation of QRS score were reported to improve the diagnostic ability of standard exercise testing in detecting silent ischemia due to restenosis, especialy, for right precordial leads, in patients undergoing PCI in right coronary artery or left circumflex artery29. The QRS score (or ATHENS Score) combine the amplitude changes in R, S, and Q waves obtained in two leads and use a cut-off of less than 5 mm.for the detection of ischemia30: QRS score (mm) = (ΔR- ΔQ-ΔS) avF + (ΔR- ΔQ-ΔS) V5.
The P wave prolongation or abnormal exercise induced QT dispersion (ie, the difference between the shortest and the longest QT intervals when multiple leads are compared) have been proved to increase the sensitivity of the ET for detecting ischemia.
B. Exercise testing after CABG
There is no consensus regarding the use of exercise testing after coronary artery bypass graft surgery (CABG). In this group of patients, often with rest ECG abnormalities, there is a concern about accuracy of ET. In asymptomatic patients, the rate for silent graft disease could be higher with venous conduits. The disappearance of ST depression was associated with a high probability of complete revascularization, but up to 30% of the patients with complete revascularization continue to have ST depression. Also, the ST response can be normal in the presence of occluded graft, if the other grafts are still opened. The ST–segment depression seems to be not as reliable as preoperative ST-segment depression and must be correlated with the other data obtained from ET, ie exercise capacity31.
The test provide more useful information some years later after surgery (5 to 10 years), when the likelihood of coronary disease is raising.
In a meta-analysis the ET has a sensitivity of 45% (95% CI 36% to 54%) and a specificity of 82% (95% CI 68% to 95%) for prediction of graft restenosis or progression of native disease. The imaging techniques had a better sensitivity; a sensitivity of 68% and a specificity of 84% for stress myocardial perfusion imaging, sensitivity of 86% and specificity of 90% for stress echocardiography were proven32.
In Bypass Angioplasty Revascularization Investigation (BARI) trial, which had compared an initial strategy of surgical to percutaneous revascularization on mortality and recurrent infarction in patients with multivessel disease, the patients performed an ET at one year, two years and five years after procedure. There is no important role for routine ET at least three years after revascularization, but a good exercise capacity (achieving the third stage of the Bruce protocol) and having a Duke risk score > -6 at the test performed five-years after CABG, is indicative for a two-years survival after the test33.
The ACC/AHA Practice Guidelines for Exercise Testing recommend the periodic ET monitoring only for selected, asymptomatic high risk patients for graft reoclusion as class II b indication, the same as for detection of restenosis, incomplete revascularization, or disease progression.
Another registry which had compared the two strategies, routine vs functional in 408 patients with coronary artery bypass graft surgery (CABG) was The Routine versus Selective Exercise Treadmill Testing after Coronary Artery Bypass Graft Surgery (ROSETTA-CABG) Registry. During the 12-month follow up, clinical events and cardiac catheterizations were less common among patients who underwent routine functional testing, but the numbers of revascularization procedures (cardiac catheterizations, PCI, repeat CABG) were the same. Also, the ET results had not a strong impact on prescription of anti-anginal dugs. The event rates was very low and the authors don’t warrant the routine functional strategy after CABG34. In practice the patterns vary widely and the expertise of the center rather than the clinical characteristics of the patient determines the use of ET.
In a study performed in our center on 108 patients postrevascularization, the exercise test had found to have an important role in the decision for repeated angiography (Figure 4).
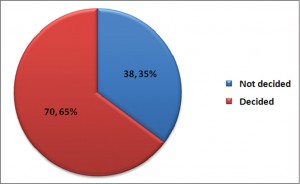
Figure 4. The role of ET in the decision for repeated coronary angiography in postrevascularization patients.
The ET was positive in more than 70% of cases for progression pf the disease, graft occlusion, or intrastent restenosis35 (Figure 5).
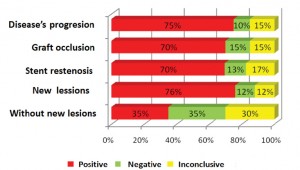
Figure 5. The exercise tests in a case series of 108 patients post revascularization and the follow-up coronary angiography. Ref.35.
To summarize, exercise testing is also a useful tool in the detection of ischemia in postrevascularization patients, as in initial evaluation of suspected CAD. A carefully analysis of the ECG changes and of the other parameters derived from ET could identify those patients with an increasing risk for restenosis. The test is safe and with a good cost/quality ratio. The postrevascularization patients are high risk patients who need to be evaluated early, but also late after the revascularization procedure. The exercise testing, especially in centers with a good expertise, is the first option in noninvasive evaluation of this growing group of patients.
Competing interests: The authors declare that they don’t have competing interests.
References
1. Nichols M, Townsend N, Scarborough P, Rayner M. Cardiovascular disease in Europe 2014:epidemiological update. Eur Heart J. 2014;35: 2950-2959
2. OECD (2014),Health at a glance: Europe 2014,OECD Publishing. http://dx.doi.org/10.1787/health_glance_eur-2014-en, pp.15-46
3. Rozanski A, Gransar H, Hayes S, Min J, Friedman JD, Thomson LEJ, Berman DS. Temporal trends in the frequency of inducible myocardial ischemia during cardiac stress testing.1991 to 2009. J Am Coll Cardiol. 2013;61:1054-65
4. Gibbons RJ, Balady G, Bricker JT, Chaitman BR, Fletcher GF, Froelicher VF, Mark DB, McCallister BD, Mooss AN, O’Reilly MG, Winters WL. ACC/AHA 2002 Guideline Update for Exercise Testing.A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Exercise Testing). 2002. American College of Cardiology Web site. Available at :www.acc.org/clinical/guidelines/exercise/dirIndex.htm
5. Fletcher G, Ades P, Kligfield P, Arena R, Balady GJ, Bittner VA, Coke LA, Jerome FL, Forman DE, Gerber TC, Gulati M, Madan K, Rhodes J, Thompson PD, Williams MA. Exercise standards for testing and training:a scientific statement from the American Heart Association. Circulation. 2013;128:873-934
6. Kligfield P, Lauer M. Exercise electrocardiogram testing.Beyond the ST segment. Circulation 2006; 114:2070-2082.
7. Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, Falk V, Filippatos G, Hamm C, Head SJ, Jüni P, Kappetein AP, Kastrati A, Knuuti J, Landmesser U, Laufer G, Neuman FJ, Richter DJ, Schauerte P, Sousa Uva M, Stefanini GG, Taggart DP, Torracca L, Valgimigli M, Wijns W, Witkowski A.2014 ESC/EACTS Guidelines on myocardial revascularization. The Task Force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Hear J 2014;35 (37):2541-2619
8. Shah BN. On the 50th anniversary of the first description of a multistage exercise treadmill test: re-visiting the birth of the ’Bruce protocol’.Heart.2013; 99 (24):1793-1794
9. Popma J, Kuntz R, Baim D. Percutaneous coronary and valvular intervention. In Baunwald’s Heart Disease. A textbook of cardiovascular medicine 7th edition. Eds: Zipes D, Libby P, Bonow R, Braunwald E. Elsevier Saunders, 2005, 1367-1402.
10. Federspiel J, Mudrick DW, Shah BR, Stearns SC, Masoudi FA, Cowper PA, Green CL, Douglas P.Patterns and predictors of stress testing modality after percutaneous coronary stenting. Data from the NCDR. J Am Coll Cardiol Img. 2012:5:969-980.
11. Garzon PP, Eisenberg MJ. Functional testing for the detection of restenosis after percutaneous transluminal coronary angioplasty: a meta-analysis. Can J Cardiol. 2001;17(1):41-8.
12. Chalela WA, Kreling JC, Falcão AM, Hueb W, Moffa PJ, Pereyra PLA, Ramires JAF. Exercise stress testing before and after successful multivessel percutaneous transluminal coronary angioplasty. Braz J Med Biol Res.2006; 39: 475-482.
13. Bengston JR, Mark DB, Honan MB. Detection of restenosis after elective percutaneous transluminal coronary angioplasty using the exercise treadmill test. Am J Cardiol.1990; 65:28-34.
14. Ruygrok PN, Webster MWI, de Valk V, van Es GA, Ormiston JA, Morel MM, Serruys PW. Clinical and angiographic factors associated with asymptomatic restenosis after percutaneous coronary intervention.Circulation 2001;104:2289-2294
15. Saririan M, Cugno S, Blankenship J, Huynh T, Sedlis S, Starling M, Pilote L, Wilson B, Eisenberg MJ. Routine versus selective functional testing after percutaneous coronary intervention in patients with diabetes mellitus. J Invasive Cardiol. 2005;17(1):25-9
16. Eisenberg MJ, Wilson B, Lauzon C, Huynh T, Eisenhauer M, Mak KH, Blankenship JC, Doucet M, Pilote L. Routine functional testing after percutaneous coronary intervention: results of the aggressive diagnosis of restenosis in high-risk patients (ADORE II) trial. Acta Cardiol. 2007;62(2):143-150
17. Eisenberg M, Schechter D, Lefkovits J, Goudreau E, Deligonul U, Mak KH, MD, Duerr D, Del Core M, Garzon P, Huynh T, MD, Smilovitch M, Sedlis S, MD, Brown DL, Brieger D, Pilote L,for the ROSETTA Investigators. Utility of Routine Functional Testing After Percutaneous Transluminal Coronary Angioplasty: Results From the ROSETTA Registry. J Invas Cardiol 2004; 16:318-322
18. Brawner CA, Ehrman JK, Schairer JR, Cao JJ, Keteyian SJ. Predicting maximum heart rate among patients with coronary heart disease receiving beta-adrenergic blockade therapy.Am Heart J.2004;184:910-914
19. Valeur N, Clemmensen P, Saunamäki K, Grande for the DANAMI-2 investigators. The prognostic value of pre-discharge exercise testing after myocardial infarction treated with either primary PCI or fibrinolysis: a DANAMI-2 sub-study. Eur Heart J. 2005;26:119-127
20. Michaelides AP, Dilaveris PE, Psomadaki ZD, Aggelakas S, Stefanadis C, Cokkinos D, Gialafos J, Toutouzas PK. Reliability of the exercise-induced ST-segment changes to detect restenosis three months after coronary angioplsty: significance of the appearance in other leads. Am Heart J.1998;135(3):449-456
21. Jørgensen B, Simonsen S, Endresen K, Forfang K, Egeland T, Thaulow E. Physiologic response to gain and loss in coronary minimal luminal diameter in patients treated with coronary angioplasty: prediction of restenosis on the basis of exercise capacity. Am Heart J. 2000; 139 (3):482-490
22. Nerla R, Di Monaco A, Sgueglia GA, Battipaglia I, Careri G, Pinnacchio G, TAzia P, Lanza GA, Crea F. Exercise stress test results in patients with bare metal stents or drug-eluting stents: pathophysiological and clinical implications. Circ J. 2010; 74(11): 2372-2378
23. Wenaweser P, Surlemy JF, Windecker S, Roffi M, Togni M, Billinger M, Cook S, Vogel R, Seiler C, Hess O, Meier B.Prognostic value of early exercise testing after coronary stent implantation. Am J Cardiol 2008; 101:807-811
24. Milo M, Nerla R, Tarzia P, Infusino F, Battipaglia I, Sestito A, Lanza GA, Crea F. Coronary microvascular dysfunction after elective percutaneous coronary intervention: correlation with exercise stress test results. Int J Cardiol. 2013;168(1):121-125
25. Gertsch M.Exercice ECG.InThe ECG a Two-Step Approach to Diagnosis.Eds Gertsch M.Springer,2004,pp 479-504
26. Kim C, Choi HE. The Predictive Value of ΣΔST/ΔHR Index for Restenosis after Percutaneous Coronary Intervention. Ann Rehabil Med. 2012;36(4):544-50
27. Hamasaki S, Arima S, TAhara M, Kihara K, Shono H, Nakao S, Tanaka H. Increase in the delta ST/delta heart rate (HR)index: a new predictor of restenosis after successful percutaneous transluminal coronary angioplasty. Am J Cardiol.1996; 78(9):990-5
28. Lehtinen R, Sievanen H, Viik J, Turjanmaa V, Niemela K, Malmivuo J. Accurate detection of coronary artery disease by integrated analysis of the ST-segment depression/heart rate patterns during the exercise and recobery phases of the exercise electrocardiography test.Am J Cardiol. 1996;78:1002-1006
29. Michaelides AP, Liakos CI, Antoniades C, Dilaveris PE, Tsiamis EG, Tsioufis KP, Aggeli KD, Toutouzas KP, Raftopoulos LG, Stefanadis CI. Right-sided chest leads in exercise testing for detection of coronary restenosis. Clin Cardiol. 2010; 33(4):236-40
30. Michaelides AP, Psomadaki ZD, Andrikopoulos GK, Aigyptiadou MN, Dilaveris PE, Richter DJ, Kartalis A, Stefanadis CI, Toutouzas PK. A QRS score versus ST-segment changes during exercise testing: which is the most reliable ischaemic marker after myocardial revascularisation? Coron Artery Dis. 2003;14(8):527-32
31. Ellestad M.Stess testing after surgical intervention and coronary angioplasty. In Stress Testing. Principles and Practice. Fifth edition.Eds. Ellestad M.Oxford University Press 2003, pp179-187
32. Chin AS, Goldman LE, Eisenberg MJ. Functional testing after coronary artery bypass graft surgery: a meta-analysis. Can J Cardiol. 2003;19(7):802-8
33. Krone R, Hardison R, Chaitman B, Gibbons R, Sopko G, Bach R, Detre K. Risk Stratification After Successful Coronary Revascularization: The Lack of a Role for Routine Exercise Testing. J Am Coll Cardiol 2001;38:136-142
34. Eisenberg MJ, Wou K, Nguyen H, Duerr R, Del Core M, Fourchy D, Huynh T, Lader E, Rogers FJ, Chaudhry R, Okrainec K, Pilote L. Lack of benefit for routine functional testing early after coronary artery bypass graft surgery: results from the ROSETTA-CABG Registry. J Invasive Cardiol. 2006;18(4):147-52
35. Moise BE, Gherasim D, Ginghină C. The predictive role of exercise testing in patients postmyocardial revascularization. Rom J Cardiol. 2012; 22, Supplement A, A227-A228.
 This work is licensed under a
This work is licensed under a