Alin Ionescu1, Monica Dobrovie1, Monica Chivulescu1, Raluca Ionescu2, Adriana Raica3, Dan Deleanu1, Carmen Ginghina1,4, Bogdan Alexandru Popescu1,4, Ruxandra Jurcut1,4
1 „Prof. Dr. C.C. Iliescu” Emergency Institute of Cardiovascular Diseases, Bucharest
2 Fundeni Clinical Institute, Bucharest, Romania
3 Asclepios Medical Centre, Constanta, Romania
4 „Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania
Abstract: Partial anomalous pulmonary venous connection (PAPVC) is a rare abnormality which consists of a failure of connection between the initial draining system of the lungs and the common pulmonary vein. Its occurrence in the left lung represents just 10% of cases and most of the time it is diagnosed as an incidental finding either by means of imaging tech-niques either during thoracic surgery that is undergone for various reasons.
Although most patients are asymptomatic, some of them develop during adulthood pulmonary arterial hypertension (PAH) which ultimately leads to overt right heart failure, raising the issue of whether or not to undergo surgical correction.
We present the case of a 66-year-old female patient for whom the defi nitive etiological diagnosis of her dyspnea required a multi-modality imaging approach, highlighting the need for complex interactions between different specialties and subspe-cialties.
Keywords: multi-modality imaging, partial anomalous pulmonary venous connection, patent foramen ovale, right heart failure.
INTRODUCTION
PAPVC is considered to be a rare congenital abnor-mality, occurring 10 times less frequently on the left side than on the right1,2. It represents the abnormal drainage of one or, less frequently, several veins from the lungs into to right atrium, most commonly by way of the brachiocephalic vein (BCV) into the superior vena cava (SVC), although there are reports descri-bing other trajectories3,4. Most of these anomalies are asymptomatic and go unnoticed, being found inciden-tally in autopsy reports5. Coexistence between PA-PVC and atrial septal defects (ASD) of various types is discovered in about 44-85% of cases6,7, thus implying the need to carefully inspect the interatrial septum. In some cases, the left-to-right shunt is significant enou-gh to cause right-sided volume overload with sub-sequent PAH, tricuspid regurgitation (TR) and right heart failure (RHF). In order to accurately diagnose this pathology and the precise anomalous connecti-ons, several imaging and interventional techniques can be employed, ranging from transthoracic or transeso-phageal echocardiography, cardiac catheterization and angiography to high resolution thoracic CT angiogra-phy or thoracic MRI with 3D reconstructions8. In a recent publication6 it was shown that surgical correc-tion, both on and off cardio-pulmonary by-pass, can be performed with reliable safety and efficacy for those patients who are symptomatic or show signs such as RV dilation, moderate-severe TR or PAH.
CASE REPORT
We report the case of a 66-year-old woman who sought medical attention on account of dyspnea and fatigability and short episodes of irregular palpitations. She was diagnosed with PHT and persistent episodes of atrial fibrillation (AF) 2 years earlier but was not investigated further. Her ECG showed AF with signs of right ventricular overload with complete RBBB with secondary repolarization abnormalities. Her laborato-ry findings revealed only hypercholesterolemia, slight hypothyroidism and a BNP of 80 pg/ml. The evaluati-on of her functional capacity test was stopped prema-turely at 5 minutes on account of dyspnea, reaching only 378 m with a slight decrease in oxygen saturation (92%). TTE raised the suspicion of left-to-right shunt, with a PFO (Figure 1) with a Qp/Qs ratio above 1.5, mo-derate-severe tricuspid insufficiency (Figure 2) with an estimated systolic pulmonary artery pressure (PAP) of 50 mmHg, dilated right heart chambers (Figure 3) with flattening of the IVS during diastole (Figure 4), with normal systolic function of both ventricles, diastolic dysfunction of the left ventricle and severe biatrial en-largement. All of these findings where confirmed by TEE: a 3D view of the interatrial septum identifi ed the PFO (Figure 5) and the saline contrast bubbles confirmed that the shunt was exclusively left-to-right (Figure 6).
In the absence of a clear etiology to explain the PAH and its accompanying symptoms, right heart ca-theterization (RHC) was performed – this confirmed the PHT, with a mean PAP of 28 mmHg, and with a Qp/Qs higher than 1. A venous abnormality was ob-served, with the left upper pulmonary lobe draining into the left brachiocephalic vein (Figure 7). A thoracic CT confirmed and detailed the venous anomaly (Figu-re 8 and 9 – the yellow arrows indicate the trajectory of the venous anomaly).
This case illustrates the difficulties encountered in establishing the precise etiology of PHT and its accom-panying symptoms and the need for multimodality ima-ging in such complex clinical scenarios. The differential diagnosis for PHT covers an extremely wide spectrum of diseases. Also, it should be noted that while a PA-PVC is infrequently encountered, especially pertaining to the left side, they are almost routinely associated with an ASD (most of them of sinus venous type).
These anomalies, usually incidentally discovered, may lead to varying degrees of left-to-right shunt which goes unnoticed until adulthood, but predispo-ses the patient to right-sided volume overload with PHT and right ventricular dysfunction. Taking into account the degree of the PHT and its implications on the cardiovascular symptoms, surgical correction can be employed with a good measure of safety and efficacy, both through minimally-invasive techniques and by median sternotomy and cardiopulmonary by-pass6. Nevertheless, surgical correction is reserved in case of symptoms and/or signs or right-sided volume overload. For the moment, a conservative strategy has been employed in the case of our patient in order to observe her response in clinical status to heart failure therapy and she’s due to follow up every 3-6 months.
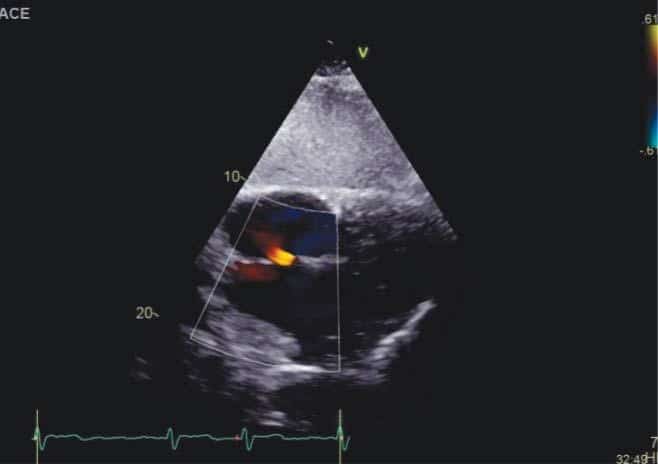
Figure 1. TTE, color-Doppler, subcostal view. PFO evidenced by diastolic flow from the left to the right atrium.
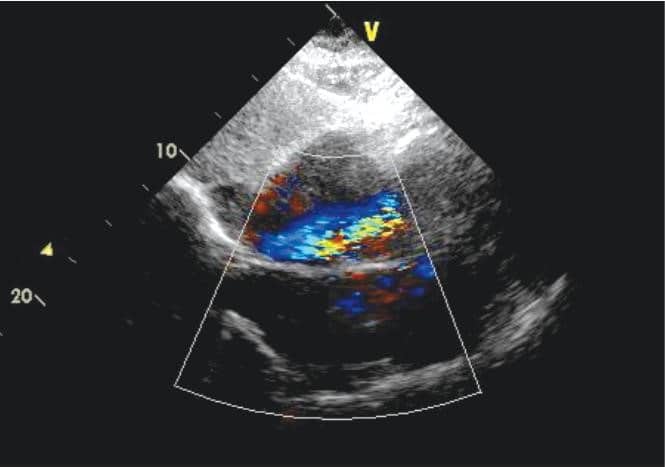
Figure 2. TTE, color-Doppler, subcostal view. Moderate-severe tricuspid insufficiency.
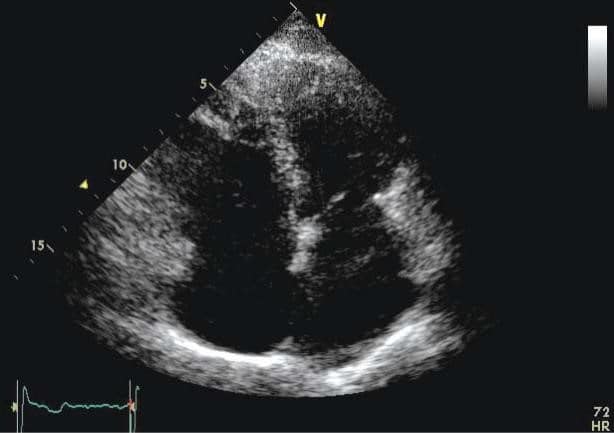
Figure 3. TTE, 2D mode, apical 4 chamber view. Dilated right heart cavities.

Figure 4. TTE, 2D mode, parasternal short axis view at the level of the papillary muscles. Paradoxical interventricular septum, with systolic flatten-ing towards the left ventricle.
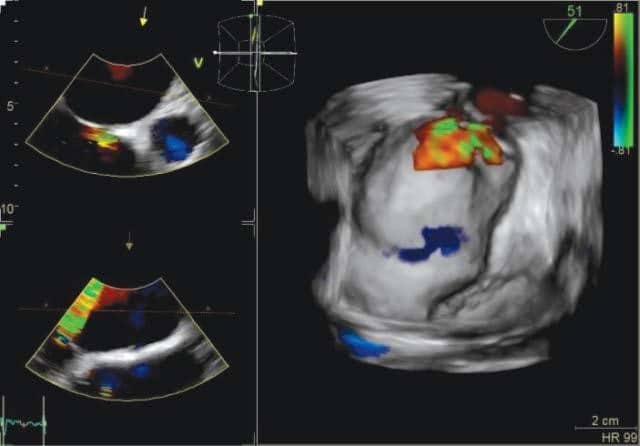
Figure 5. TOE, color-Doppler, 3 chamber view. PFO is revealed.
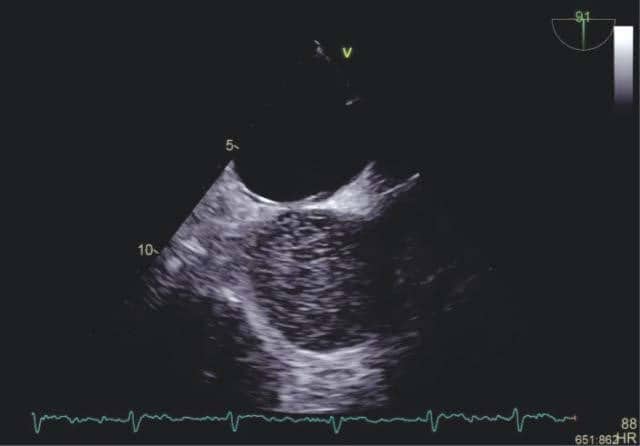
Figure 6. TOE, 2D mode, 90 degrees. Saline (bubble) study revealed the shunt is strictly left-to-right (by injecting agitated saline into a peripheral vein which reaches the right atrium but do not reach the left atrium).
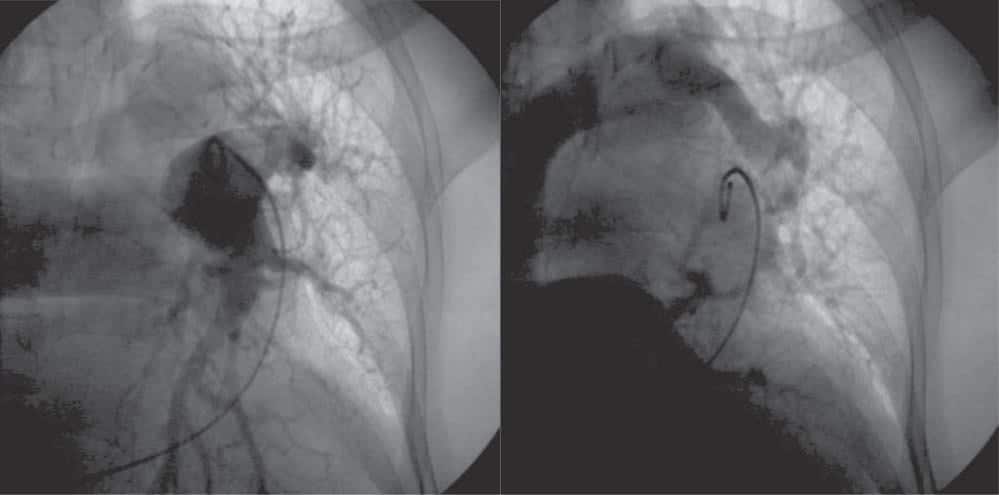
Figure 7. Pulmonary angiography. Left: injection of contrast into the left pulmonary artery. Right: the venous network of the superior part of the left lung drains in the left brachiocephalic vein and not in one of the pulmonary veins.
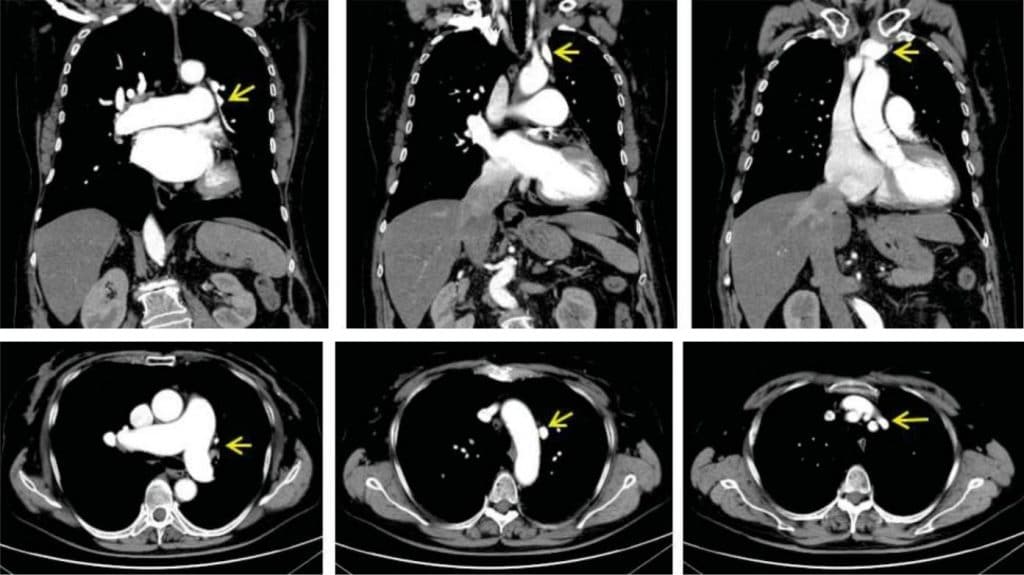
Figure 8. CT pulmonary angiography, venous phase, coronal sections. Tracking of abnormal left pulmonary upper lobe drainage into the left brachiocephalic vein (yellow arrows).
CONCLUSIONS
Multimodality imaging techniques are an essential approach to correctly diagnose the etiology behind PHT and to reach the most suitable therapeutic stra-tegy, either surgical or conservative.
Conflict of interest: none declared.
References
1. Snellen HA, van Ingen HC, Hoefsmit EC. Patterns of anomalous pul-monary venous drainage. Circulation 1968;38:45–63.
2. Javangula K, Cole J, Cross M, Kay PH. An unusual manifestation of left partial anomalous pulmonary venous connection. Interactive Cardiovascular and Thoracic Surgery JO Interact CardioVascTho-racSurg 2010;11:846-848. PMID: 20805252.
3. Hiji T, Fukushige J, Hara T. Diagnosis and management of partiala-nomalous pulmonary venous connection. Cardiology 1998;8:148– 151.
4. Zylak CJ, Eyler WR, Spizarny DL, Stone CH. Developmental lung anomalies in the adult: radiologic-pathologic correlation. Radio-graphics. 2002;22:S25-43. PMID: 12376599.
5. Van Meter C Jr, LeBlanc JG, Culpepper WS III, Ochsner JL. Partiala-nomalous pulmonary venous return. Circulation 1990;82:207–213.
6. Elbardissi AW, Dearani J, Suri R, Danielson G. Left-sided partial anomalous pulmonary venous connections. Ann Thorac Surg 2008; 85:1007-1014. PMID: 18291189.
7. Gupta, Monesha. Partial Anomalous Pulmonary Venous Connection. Emedicine [Online]. 2010. Available at http://emedicine.medscape. com/article/897686-overview. Accessed 7th October 2017
8. Dillon EH, Camputaro C. Partial anomalous pulmonary venous drainage of the left upper lobe vs duplication of the superior vena cava: distinction based on CT findings. AJR Am J Roentgenol. 1993 Feb;160(2):375-9.
 This work is licensed under a
This work is licensed under a