Liviu Macovei1,2, Larisa Anghel1, Mircea Balasanian1,2, Dan Mihai Alexandrescu1, Catalina Arsenescu Georgescu1,2
1 “Prof. Dr. George I. M. Georgescu” Cardiovascular Diseases Institute, Iasi, Romania
2 “Grigore T. Popa” University of Medicine and Pharmacy, Iasi, Romania
Abstract: We present the case of a 49 years old woman with Takayasu arteritis, and rapid evolution of the coronary lesions, involving the left main coronary artery. The endovascular or surgical treatment of coronary vascular disease and aortic regurgitation involved a very high risk, determined by the important and diffuse fibrotic or calcification lesions from aortic or coronary arteries. So, “in extremis”, we performed the percutaneous transluminal coronary angioplasty of the left main coronary artery (LM) and right coronary artery (RCA), despite all the major risks induced by this procedure.
Keywords: Takayasu arteritis, prognostic, coronary lesions, case report.
INTRODUCTION
Takayasu arteritis is a rare chronic infl ammatory arteritis of large and medium-sized arteries, a panarteritis with intimal proliferation. This granulomatous panarteritis predominates in women, typically before the age of 40s, with an up to 10:1 ratio for female-to-male1. The aorta may be involved throughout its entire length and, even though any of its branches can be diseased,
the most commonly affected are the subclavian and the common carotid arteries. The pulmonary arteries are involved for up to 50% of patients, much less being described the critical coronary lesions and the major aortic regurgitation2,3. Coronary disease is often asymptomatic, as illustrated by the identification of silent myocardial injury for 27% of patients. Myocardial perfusion defects were present in 53% of the cases, while intra-arterial angiography has shown that the coronary artery lesions typically affected the ostia and proximal segments for up to 30% of the cases4,5. There are important limitations in Takayasu arteritis, sometimes the endovascular or surgery treatment involving a higher risk, due to diffuse calcifi cations. The care of patients with TA requires a team approach that includes clinicians familiar with the proper use of immunosuppressive therapies, vascular imaging and intervention specialists and, in the setting of critical
stenosis or aneurysms, cardiovascular surgeons. For most patients, medical and surgical therapies provide important palliation6,7.
CASE REPORT
We present the case of a 49 years old women diagnosed with Takayasu arteritis (type VC) who was referred to our service for the fi rst time fi ve years ago, for stable angina and effort dyspnea. At that time, the echocardiography showed normal left ventricular function and minimal aortic regurgitation, with no critical coronary lesions detected at invasive coronary angiography examination, but with multiple and diffuse arterial calcifications specific for Takayasu arteritis. According to the American College of Rheumatology classification criteria, at 34 years old the patient was diagnosed with Takayasu arteritis based on: the age younger than 40 years at disease onset, claudication of the extremities, decreased pulsation of both brachial arteries, difference more than 10 mmHg in systolic blood pressure between arms and arteriographic narrowing of the primary branches of the aorta and large arteries in the upper extremities that is not due to arteriosclerosis,
fi bromuscular dysplasia, or other causes. The presence of these criteria yields a sensitivity of 90.5% and a specificity of 97.8%8. At this visit, the patient had 15 years since she was diagnosed with Takayasu arteritis. When she was initially diagnosed with this large-vessel vasculitis, she complained of other constitutional symptoms such as fatigue, malaise and giddiness without other clinical
complications. Because she had only a mild form of Takayasu arteritis, she didn’t require a long term corticosteroid treatment. She had a good response to initial corticosteroid therapy, without relapses and prednisone was administered only for 2 months, until the constitutional symptoms disappeared. Under medical treatment (rilmenidinum 1 mg/day, amlodipinum 20 mg/day, atorvastatinum 40 mg/day, clopidogrel 75 mg/day), the patient’s evolution was uneventful for 4 years and 9 months, then she presented unstable angina and heart failure symptoms. At this time, the electrocardiogram showed normal sinus rhythm and her blood results showed no signifi cant changes. A transthoracic echocardiogram demonstrated a normal left ventricular ejection fraction of 50%, mild aortic insufficiency, without dissection of the ascending aorta and aortic arch. This time, the coronary artery CT examination revealed an important evolution of coronary lesions (diffuse non-obstructive coronary lesions), especially on the right coronary artery and on the left anterior descending coronary artery. The endovascular or surgery treatment for coronary
disease and aortic regurgitation were discussed, with the consensus for medical treatment, considering the presence of a very high operatory risk. After only 3 months, the patient has presented for
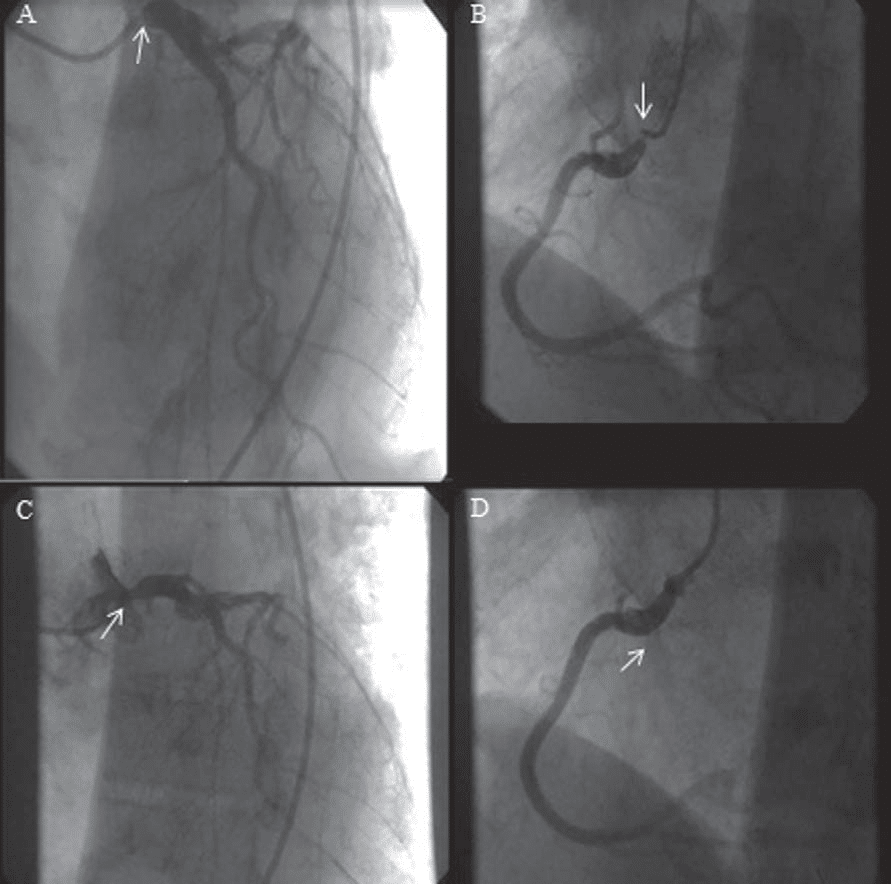
acute coronary syndrome with increased level of troponin. The coronarographic control revealed a subocclusion of the left main coronary artery (LM) and right coronary artery (RCA) (Figure 1).
Figure 1. Left main (LM) and right coronary artery (RCA) pre and post PTCA with stent. A – subocclusion of LM. B – ostial subocclusion of RCA. C – PTCA with stent on LM. D – PTCA with stent on RCA.
Even though, for other cases the solution has been the CABG, the surgery was not indicated in this case, considering the impossibility of the aorto-coronary anastomoses due to the calcified arterial lesions. Thus, in this situation, we limited to an interventional treatment, considering the fact that the patient was also in an inactive stage of Takayasu arteritis. After selective intubation of the left main trunk ostium with a JL 4 SH guide catheter, we cross the stenosis area and successively predilatation with a 3.0/15 mm balloon at 20-22 atm, with diffi cult dilatation of the ostia due to severe calcifi cations. We implant a pharmacologically active 4.0/13 mm stent at 18 atm, post dilated with the same balloon at 22 atm, yielding the regression of the lesion from 95% to 0%.
In the same procedure, we implant a pharmacologically active 40/22 mm stent in the right coronary artery, reducing the degree of stenosis from 95% to 0% (Figure 1). After the myocardial revascularization, the patient was hemodynamically stable, without angina or arrhythmic events and was discharged home after five days. We began the chronic treatment with high dose
of atorvastatin 80 mg/day, beta blocker, angiotensin converting enzyme inhibitor and double antiaplatelet agents. The one year follow-up of the patient showed a good evolution, without angina or dyspnoea.
DISCUSSION
This case report represents an important diagnosis and treatment challenge for clinical practitioners, because of the severity and complex coronary lesions and important treatment limitations. The endovascular or surgical treatment for coronary disease and aortic regurgitation involved a very high risk, determined by important and diffuse fibrotic or calcification lesions of the aortic or coronary arteries. Another particularity of this case is the rapid evolution of the coronary artery lesions, involving the left coronary main. Afterwards, it is important to underline the limits of
surgical treatment in this situation, the “in extremis” choice being the percutaneous transluminal coronary angioplasty of the left main coronary artery and right coronary artery, with all the major risk induced by this procedure. Conflict of interests: none declared.
References:
1. Arend WP, Michel BA, Bloch DA, Hunder GG, Calabrese LH, Edworthy SM, Fauci AS, Leavitt RY, Lie JT, Lightfoot RW Jr. The American College of Rheumatology 1990 criteria for the classifi cation of Takayasu arteritis. Arthritis Rheum 1990; 33(8):1129-1134.
2. Bonow RO, Mann DL, Zipes DP, Libby P. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine 10th ed. Philadelphia, PA. Elsevier Health Sciences 2014; 1847-1849.
3. PereraA H, Youngstein T, Gibbs RGJ,Jackson J E, Wolfe JH, Mason JC.Optimizing the outcome of vascular intervention for Takayasu arteritis. Br J Surg 2014; 101 (2):43-50.
4. Soto ME, Melendez-Ramirez G, Kimura-Hayama E, Meave-Gonzalez A, Achenbach S, Herrera MC, Guering EL, Alexánderson-Rosas E, Reyes PA. Coronary CT angiography in Takayasu arteritis. JACC Cardiovasc Imaging 2011; 4(9): 958-966.
5. Zhang H, Liu D, Li X, Tan H, Jin Q, Liu X. Intractable angina pectoris after coronary artery bypass surgery in Takayasu arteritis involving the aorta ventralis and main coronary artery in a young girl. Int J Clin Exp Med 2014; 7(1):320-322.
6. Chatterjee S, Flamm SD, Tan CD, Rodriguez ER. Clinical Diagnosis and Management of Large Vessel Vasculitis: Takayasu Arteritis. Current Cardiology Reports 2014; 16(7): 499.
7. Mason JC. Takayasu arteritis: surgical interventions. Current Opinion in Rheumatology 2015; 27(1):45-52.
8. Arend WP, Michel BA, Bloch DA, Hunder GG, Calabrese LH, Edworthy SM, et al. The American College of Rheumatology 1990 criteria for the classifi cation of Takayasu arteritis. Arthritis and Rheumatology 1990; 33(8):1129-1134.
 This work is licensed under a
This work is licensed under a