R. M. Chreih1,3, D. Deleanu2, Carmen Ginghină2,3
Article received on the 15th of March 2013. Article accepted on the 31st of May 2013.
1 Clinique Chirurgicale du Libournais, Libourne, France
2 Emergency Institute for Cardiovascular Disease „Prof. Dr. C.C. Iliescu”, Bucharest, Romania
3 “Carol Davila” Medicine and Pharmacy University, Bucharest, Romania
Rami Mihail Chreih, MD
Clinique Chirurgicale du Libournais, Libourne, France
Abstract: Premises – Coronary flow on non-culprit coronary arteries in Acute Coronary Syndrome patients that underwent coronary angioplasty offers important information on global myocardial integrity. Material and methods – For this study the coronary flow on non-culprit coronary arteries in Acute Coronary Syndrome patients (110 patients – Case Group) was analyzed and was compared to the coronary flow in non-coronary patients that underwent coronary angiography (230 patients – Control Group). In order to analyze the coronary flow, the Corrected TIMI Frame Count / Minimal Luminal Diameter (CTFC/MLD) method was employed. Results – The comparative analysis of the coronary flow on non-culprit arteries and of the coronary flow on normal coronary arteries the following results were obtained: 8.182 ± 2.112 vs. 5.441 ± 0.9950 (p < 0.005) for all coronary arteries; 8.121 ± 2.2121 vs. 5.247 ± 1.0327 (p < 0.005) for the Left Anterior Descending artery; 7.972 ± 1.9510 vs. 5.584 ± 0.9214 (p < 0.005) for the Circumflex Artery; 8.244 ± 2.1248 vs. 5.341 ± 0.9752 (p < 0.005) for the Right Coronary Artery. Conclusions – The study proved that coronary flow is significantly slower on non-culprit coronary arteries in Acute Coronary Syndrome than on normal coronary arteries in non-coronary patients, when analyzing all three coronary arteries together as well as when separately analyzing each of the three coronary arteries. The slower coronary flow on non-culprit coronary arteries in Acute Coronary Syndrome patients is a proof of global myocardial suffering.
Keywords: Acute Coronary Syndrome, angioplasty, coronary angiography, CTFC/MLD
Rezumat: Premize – Fluxul sanguin la nivelul arterelor coronare neresponsabile în Sindromul Coronarian Acut (SCA) la pacienții unicoronarieni tratați prin angioplastie coronariană cu stent oferă informații importante privind integritatea miocardică globală. Material și metode – În cadrul acestui studiu am analizat fluxul sanguin la nivelul arterelor coronare neresponsabile de Sindromul Coronarian Acut la pacienți unicoronarieni (110 pacienți – grupul Caz) și am comparat acest flux cu fluxul coronar al pacienților non-coronarieni care au fost supuși coronarografiei în cadrul protocolului preoperator (230 pacienți – grupul Control). Pentru analiza fluxului coronarian, s-a folosit metoda TIMI cu numărătoarea fotogramelor corectată / diametrul luminal minim (CTFC/MLD). Rezultate – La analiza comparativă a fluxului coronarian pentru arterele neimplicate în Sindromul Coronarian Acut și pentru arterele coronare normale angiografic se obțin rezultatele: 8,182 ± 2,112 vs. 5,441 ± 0,9950 (p <0,005) pentru analiza tuturor arterelor coronare; 8,121 ± 2,2121 vs. 5,247 ± 1,0327 (p <0,005) pentru Artera Descendentă Anterioară; 7,972 ± 1,9510 vs. 5,584 ± 0,9214 (p <0,005) pentru Artera Circumflexă; 8,244 ± 2,1248 vs. 5,341 ± 0,9752 (p <0,005) pentru Artera Coronară Dreaptă. Concluzii – Studiul a demonstrat că fluxul coronarian este semnificativ mai lent la nivelul coronarelor neresponsabile pentru pacienții cu Sindrom Coronarian Acut în comparație cu fluxul coronarian la nivelul arterelor coronare normale pentru pacienții non-coronarieni, atât la analiza comună a tuturor celor trei artere coronare cât și în cazul fiecărei artere coronare analizate separat. Această încetinire a fluxului coronarian la nivelul coronarelor neimplicate în Sindromul Coronarian Acut este o dovadă a suferinței miocardice globale.
Cuvinte cheie: sindrom coronarian acut, angioplastie, coronarografie, CTFC/MLD
INTRODUCTION
Nowadays, the importance of cardiovascular pathology reaches the highest levels because of the increase of the population mean age, and because the increase of the cardiovascular risk factors exposure. Acute Coronary Syndrome (ACS) is the most important factor regarding cardiovascular morbidity and mortality1. The medical and economical implications that ACS has make ACS the main target for scientific research and development. Today, the main therapy in ACS is coronary angioplasty and stenting2,3.
The current study was triggered by the noticing of the existence of patients in which the myocardial impairment in ACS is proportional with the area irrigated by the culprit artery, patients that show a mismatch between the successful coronary angioplasty and the less than favorable post-procedural evolution.
MATERIAL AND METHODS
The current study is a prospective case-control study that carried on for 3 years (April 2006 – April 2009). Patients admitted at Emergency Institute for Cardiovascular Disease „Prof. Dr. C.C. Iliescu” – Bucharest were recruited for this study. Coronary angiography and angioplasty procedures took place in the interventional cardiology department.
Thus, 110 patients admitted with ACS and treated with coronary angioplasty and stenting were recruited. These patients formed the Case group.
Inclusion criteria for these patients were:
- Acute Coronary Syndrome diagnosis
- This implies the fact that the patient must fulfill the diagnostic criteria for Coronary Syndrome and that the patient must also be addressed so as for the intervention to take place in the acute phase of the pathology, the moment in which the benefit is maximal.
- The patient must undergo coronary angioplasty and stenting
- This second criterion implies that the patient must have the indication coronary angioplasty and stenting, thus implying that patient anatomy is compatible with coronary angioplasty and that lesion location is accessible for angioplasty.
- The patient must have single-vessel coronary disease
- This criterion involves non-culprit coronary arteries, arteries that must be lesion free so as not to lead to any bias; coronary plaque, even if not important from a stenosis point of view, might influence the investigated coronary flow, flow transformed in continuous variable.
- Recording quality
- This criterion involves technical target-points:
- Thus, first the contrast filling visualization of the whole coronary vessel is necessary in order to correctly evaluate the time the substance needs to flow from one marker to another. There are cases, for instance left coronary main stem lesions or proximal lesions, in which the operator might use diaphragms that may care improve lesion image, but that interfere with distal segment visualization.
- Second, the recording must be made at 30 frames /second. Although this objective might seem easy obtainable, there are cases in which the operator must use lower recording frequencies: patients that for different reasons must receive the minimal irradiating dose or technical limitations that impose lower recording frequencies.
- Third, the analyzed coronary arteries must be filled in an even way and with an antegrade direction. Thus, the intracoronary contrast column must not contain discontinuities or “gaps” so as not to become a bias in coronary flow speed calculus. Also, antegrade flow certifies that he analyzed flow is the flow originated directly from contrast injection, any retrograde flow phenomenon being the consequence of collateral circulation influence on the flow in the analyzed artery, and, by consequence a bias in flow calculation.
- Recording for the flow on non-culprit coronary arteries must be made before the culprit vessel angioplasty. Otherwise, coronary flow analysis for non-culprit vessel might be compromised by hemodynamic phenomena that occur after angioplasty (hyperemia, etc.)
- This criterion involves technical target-points:
Exclusion criteria for these were:
- Coronary impairment or pectoral angina history
- Multi-vessel Acute Coronary Syndrome
- Valvular aortic stenosis
- Left ventricle impairment
230 patients with normal coronary arteries were also recruited. In order to a respect both the ethical criteria of this study and the favorable risk/benefit ratio of coronary angiography, patients that had to undergo coronary angiography for pre-valvular-surgery protocol were selected. These patients formed the Control group.
The inclusion criteria for Control group patients were:
- The coronary angiography must be performed for the pre-surgery protocol
- Patients that need to have a coronary angiography for the pre-surgical protocol for heart surgery (valvuloplasty / valvular prosthesis). Patients with valvular impairment were selected, in order not to be biased by any coronary flow interference.
- The patient must not have aortic valvular disease
- This criterion is selected in order to eliminate potential biases due to coronary hypo-perfusion; aortic valvular patients were not included in this study.
- The patient must not have coronary lesions
- In order to eliminate any potential bias involving coronary flow analysis, patients with coronary lesions were not included, regardless of the importance and/or the age of the lesions, any coronary lesion being an obstacle for the coronary flow
- The patient must not have pectoral angina
- In order to eliminate any coronary flow bias, patients with pectoral angina symptoms were not include regardless of diagnostic criteria presence or absence, thus not including patients with potential microcirculatory dysfunction, X coronary syndrome, etc.; phyisiopathologic mechanisms involved in all these pathologies not being clearly proven and universally accepted, one cannot exclude coronary flow impairment in these cases, and thus the presence of a potential bias
- The patient must have an intact ventricular function
- This criterion was introduced in order to eliminate potential coronary flow analysis bias due to coronary hypo-perfusion involved in pump-failure.
- Recording quality
- As for the Case group, technical criteria are important and imply:
- Visualization of whole vessel contrast filling
- Recording at a minimal frequency of 30 frames per second
- The filling of the coronary artery must be even, total and antegrade
- As for the Case group, technical criteria are important and imply:
Exclusion criteria for the Control group were:
- Coronary disease or pectoral angina history
- Aortic valvular disease
- Systolic left ventricle impairment
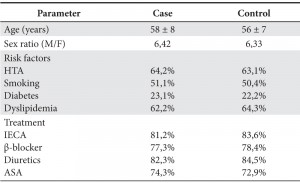
Two patient groups were obtained, groups that were equal from demographical, form cardiovascular risk factors and from preexisting treatment point of view (Table 1).
Table 1. Characteristics of analyzed groups between Aprilie 2006 – Aprilie 2009.
In order to analyze coronary flow as a continuous variable, the corrected TIMI frame count / Minim Luminal Diameter (CTFC/MLD) was chosen, and frame count was manually done through frame-by-frame count. The method proposed by Michael Gibson4 and improved by Goran Stankovic6 was adapted by counting the number of frames needed by the coronary flow to reach the standardized distal markers for the left anterior descending artery and for the right coronary artery, and the analysis of the longest dye path was chosen for the circumflex artery (Figures 1-6). The sizing of the minimal luminal diameter was done using the Quantitative Coronarography Analysis (QCA) method, using the software incorporated in angiography machines.
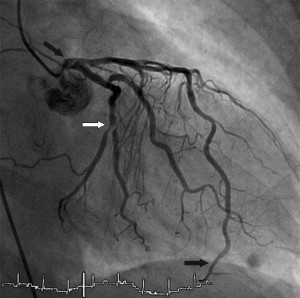
Figure 1. Example of analysis of a Left Anterior Descending artery Acute Coronary Syndrome: the white arrow shows the culprit lesion on the Circumflex artery and black arrows show the markers for flow analysis.

Figure 2. Example of analysis of a non-culprit Circumflex artery: the white arrow shows the culprit lesion on the Left Anterior Descending artery and black arrows show the markers for flow analysis.
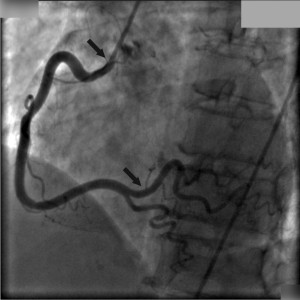
Figure 3. Example of analysis of a non-culprit Right Coronary Artery: black arrows show the markers for flow analysis.

Figure 4. Example of left coronary artery eliminated from the analysis for technical reasons: the distal landmark is not visible.
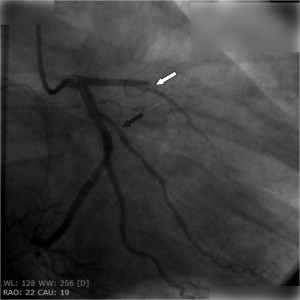
Figure 5. Example of non-culprit Circumflex artery eliminated from the analysis: the white arrow shows the culprit lesion on the Left Anterior Descending artery and the black arrow shows a lesion on the first marginal (Mg1).
Figure 6. Example of Right Coronary Artery eliminated from the analysis for technical reasons: the distal landmark is not visible, the operator has introduced filters/diaphragms that block the visualization of the whole vessel.
In order to validate this method, a sample-group of 10 randomly chosen patients was made in order to verify intra-operator measuring. For these patients, all recordings were copied the names were hidden, then recordings were randomly sent for interpretation, several times, to the initial operator so as to reveal any potential errors due to interpretation. There were no significant differences noticed for the intra-operator interpretation.
Another sample-group of other 10 randomly chosen patients was made in order to verify inter-operator measuring. For these patients, all recordings were copied the names were hidden, then recordings were randomly sent for interpretation to several operators so as to reveal any potential errors due to interpretation. There were no significant differences noticed for the intra-operator interpretation.
DATA CENTRALIZATION AND STATISTICAL INTERPRETATION DESCRIPTION
Data thus obtained were centralized and analyzed using specific calculus and statistical software (Microsoft Excel 2007, SPSS 10).
The statistic tests used were mean and mean square root, Anova or t Student test. These tests ar adapted for continuous variable analysis.
RESULTS
Statistically significant differences were noticed between coronary flow on non-culprit coronary arteries and coronary flow on normal angiographic arteries. These differences are valid as for the global analysis of the three coronary arteries, as well as for each of the three coronary arteries separately analyzed.
Thus the global analysis of coronary flow for all three coronary arteries returns the value of 8,182 ± 2,1112 for non-culprit coronary arteries and the value of 5,441 ± 0,9950 for coronary flow on normal angiographic arteries, in Control group patients, this difference being statistically significant (p<0,005) (Fig. 7).
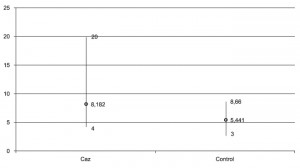
Figure 7. CTFC/MLD values obtained after coronary flow analysis in all coronary arteries for the patients that underwent coronary angioplasty for ACS (Case group), as well as for normal angiographic coronary patients (Control group).
The values obtained for the Left Anterior Descending (LAD) are: 8,121±2,2121 for the Case group (patients that underwent coronary angioplasty for ACS), respectively 5,247±1,0327 for the Control group (patients with normal angiographic coronary arteries). The obtained difference has statistical significance (p<0,005) (Fig. 8).
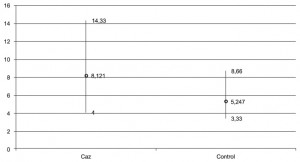
Figure 8. The values obtained after coronary flow analysis for the Left Anterior Descending artery (LAD) for Case group patients, respectively for Control group ones.
As for the circumflex artery (Cx), the results are: 7,972±1,951 for the Case group, respectively 5,584 ± 0,9214 for the Control group (p<0,005) (Fig. 9).
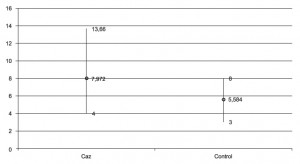
Figure 9. The values obtained after coronary flow analysis for the Cirumflex artery (Cx) for Case group patients, respectively for Control group ones.
The Right Coronary Artery (RCA) analysis obtained the results: 8,244 ± 2,1248 for the Case group, respectively 5,341 ± 0,9752 for the Control group (p <0,005) (Fig. 10).
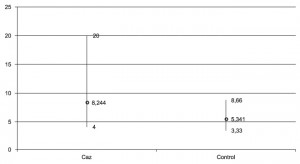
Figure 10. The values obtained after coronary flow analysis for the Right Coronary Arteries (RCA) for Case group patients, respectively for Control group ones.
DISCUTIONS
A statistically significant difference statisticaly proven through the CTFC/MLD method is noticed when analyzing the coronary flow, a deceleration of coronary flow being proven on non-culprit coronary arteries in Acute Coronary Syndrome. Thus, the actual point of view, which states that coronary occlusion on the culprit vessel in Acute Coronary Syndrome will trigger the subsequent myocardial impairment, and the suffering myocardial segment will trigger blood flow intake through collateral circulation, is countered, because, according to this point of view coronary blood flow should have been accelerated on non-culprit coronary arteries.
The fact that coronary flow is slow on non-culprit arteries indicates a suffering of the distal circulatory bed in segments in which normally should not have been affected by Acute Coronary Syndrome.
Thus, the results confirm the initial theory stating that in Acute Coronary Syndrome there is a global myocardial suffering.
Gianmario Sambuceti and Mario Marzilli9,10 have studied the part coronary microcirculation plays in Acute Coronary Syndrome and have proven the existence of paradoxal vasoconstriction of myocardial microcirculation in patients that had a sudden increase in oxygen consumption and in patients with unstable angina, during angina crisis. Also, microcirculation dilatation had a proven benefit on myocardial ischemia severity. Maybe the most important aspect of this article is that it proves the fact that treatment targeting microcirculation significantly ameliorates the result of coronary angioplasty.
Amir Lerman proposed a new vision on myocardial microcirculatory dysfunction12 by challenging the existence myocardial microcirculatory dysfunction in Acute Coronary Syndrome only as a secondary angioplasty, consequence of distal micro-embolic incidents, of the reperfusion lesion, of inflammatory phenomena. Lerman proposes the existence of a possible primary microcirculatory dysfunction, microcirculatory dysfunction that preceded the angioplasty. Maybe the most important aspect of the Amir Lerman article is the fact that the author proposes that this new vision has to become part of patient selection prior to coronary angioplasty and before initiating a coronary angioplasty. The idea of global myocardial impairment is thus supported, impairment with consequences on coronary angioplasty complications and on middle term patient evolution.
There is a theory that ignores the existence of a generalized microcirculatory dysfunction in Acute Coronary Syndrome, a theory that has to be mentioned. This is the theory supported by Francisco Torrent-Guasp, also known as the “ventricular myocardial band”/ the “double helix” / the “Spanish serpentine”16-18. In 1972 Francisco Torrent-Guasp exposed a new theory on ventricular myocardial structure, theory that states that the myocardium is not formed from several muscular layers with different disposition of the fibers, but from a singular band layer disposed as a double-helix. According to this theory, the three-dimensional disposition of myocardial fibers might explain, from a functional point of view, the ventricular suction as well as the ventricular ejection. Also, if this theory was initially an eccentric theory, the development of imagistic techniques, especially echocardiography (speckle tracking method), brought up evidence supporting this theory, today the visualization of left ventricular contraction being possible, contraction that is not predominant circular, nor predominant longitudinal, but is a “spiral torsion”. This theory does not contradict the existence of a global myocardial dysfunction in Acute Coronary Syndrome: according to this theory, a segmental dysfunction leads to a dysfunction / an interruption within the continuity of the myocardial structure, eventually leading to a dysfunction that involves the myocardial function from a global point of view.
Dan Deleanu8 indicated for the first time the problem of the existence of slow coronary flow on non-culprit coronary arteries in Acute Coronary Syndrome when compared with coronary flow on normal angiographic arteries, proving this by CTFC (Corrected TIMI Frame Count) method. The current study continued the study made by Dan Deleanu and supported that data using an improved method to analyze coronary flow.
Neal Uren also proves the existence of myocardial suffering based on the diminished coronary flow reserve and on altered metabolism in myocardial area irrigated by normal angiographic coronary arteries, areas that are not in the neighborhood of the ischemic myocardial area19. Yet, Neal Uren clearly states that the result is valid only for myocardial ischemia and it is not valid in the presence of myocardial necrosis. The Uren study data clearly sustain the idea of global myocardial suffering and (more than that) proves the existence of metabolic and micro-vascular mechanisms that support the hypothesis of the current study.
Eric Topol states the existence of dissociation between the technical result of the angioplasty and the patient evolution; the dissociation implies that the risk must become the target of future research, the main target being long-term survival, without the repetition of coronary events and without the limitation symptoms of cardiac disease20-23.
STUDY LIMITS
An important limit of this study is the fact that the purpose of this research was not to prove in a detailed manner the mechanism(s) involved in global myocardial suffering in Acute Coronary Syndrome, the target of this study being to take a first step towards this theory, having based itself on general indirect evidence.
Another limit regards the inclusion/exclusion criteria, patients without previous coronary disease and myocardial disease being included. If the Control group patients / Normal angiographic coronary arteries were verified from their personal history point of view, for ethical and procedural reasons, patients with Acute Coronary Syndrome were included based on their own statements, and the fact that the patient had no knowledge of previous pathology does not necessarily mean the absence of that pathology.
CONCLUSIONS
- There is a statistical significant slower coronary flow on non-culprit coronary arteries in Acute Coronary Syndromes compared with the coronary flow on normal angiographic arteries, supporting the theory of global myocardial suffering in Acute Coronary Syndrome.
- Coronary flow is slower on non-culprit coronary arteries in Acute Coronary Syndrome when compared with coronary flow on normal angiographic arteries affirmation valid for the flow analyzed in its globality, for all of the three coronary arteries analyzed together, as well as for each coronary artery separately analyzed.
All these partial conclusions support the initial hypothesis stating that Acute Coronary Syndrome leads to global myocardial suffering, suffering proven by slower coronary flow on non-culprit coronary arteries when compared with flow in normal angiographic arteries.
Conflict of interests: The authors declare that no conflict of interest exists.
Bibliography
1. Boersma H, Doornbos G, Bloemberg BPM, Wood DA, Kromhout D, Simoons ML. Cardiovascular diseases in Europe. European Society of Cardiology, 1999.
2. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation (2011). European Heart Journal, 32 (2011) 2999-3054.
3. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation (2012). European Heart Journal, 33 (2012) :2569-2619
4. Gibson CM, Cannon CP, Daley WL, et al. TIMI frame count: a quantitative method of assessing coronary artery flow. Circulation 1996; 93:879-888
5. Gibson CM, Cannon CP, Sabina A, et al. Relationship of the TIMI Myocardial Perfusion Grades, Flow Grades, Frame Count, and Percutaneous Coronary Intervention to Long-Term Outcomes After Thrombolytic Administration in Acute Myocardial Infarction. Circulation 2002; 105:1909-1913
6. Stankovic G, Manginas A, Voudris V, et al. Prediction of Restenosis After Coronary Angioplasty by Use of a New Index : TIMI Frame Count/
Minimal Luminal Diameter Ratio. Circulation 2000, 101:962-968
7. Heusch G, Kleinbongard P, Böse D, Levkau B, Haude M, Schulz R, Erbel R. Coronary Microembolization – From Bedside to Bench and Back to Bedside. Circulation. 2009; 120:1822-1836
8. Deleanu D Angioplastia coronariană percutană în infarctul miocardic acut și angina instabilă postinfarct. Teză de doctorat 2006, Biblioteca UMF Carol Davila București
9. Sambuceti G, L’Abbate A, Marzilli M, Why should we study the coronary microcirculation? Am J Physiol Heart Circ Physiol 2000;279: H2581-H2584
10. Marzilli M, Sambuceti G, Fedele S, L’Abbate A, Coronary microcirculatory vasoconstriction during ischemia in patients with unstable angina. J Am Coll Cardiol 2000;35:327-334
11. ESC Guidelines for the diagnostic and treatment of acute and chronic heart failure (2012) – European Heart Journal, 33 (2012) : 1787 – 1847
12. Lerman A, Holmes DR, Hermann J, Gersh BJ. Microcirculatory dysfunction in ST-elevation myocardial infarction: cause, consequence or both? European Heart Journal : 28 (2008) : 788-97
13. Sambuceti G, L’Abbate A, Marzilli M, Why should we study the coronary microcirculation? Am J Physiol Heart Circ Physiol 2000;279: H2581-H2584
14. Sambuceti G, Marzullo P, Giorgetti A, Neglia D, Marzilli M, Salvadori P, L’Abbate A, Parodi O, Global alteration in perfusion response to increasing oxygen consumption in patients with single vessel coronary artery disease. Circulation 1994;90:1696-1705
15. Sambuceti G, Marzilli M, Marraccini P, Schneider-Eicke J, Gliozheni E, Parodi O, L’Abbate A, Coronary vasoconstriction during myocardial ischemia induced by rises in metabolic demands in patients with coronary artery disease. Circulation 1997;95:2652-2659
16. Torrent-Guasp F, [Macroscopic structure of the left ventricle. II. The basal half] Rev Esp Cardiol. 1972;25(2):109-18
17. Torrent-Guasp F, [Macroscopic structure of the ventricular myocardium] Rev Esp Cardiol. 1980;33(3):265-87
18. Torrent-Guasp F, [Structure and function of the heart] Rev Esp Cardiol 1998;51(2):91-102
19. Uren NG, Marraccini P, Gistri R, de Silva R, Camici PG, Altered coronary vasodilator reserve and metabolism in myocardium subtended by normal arteries in patients with coronary artery disease elsewhere. J Am Coll Cardiol 1993;22:650-653
20. Topol EJ, Nissen SE, Our preoccupation with coronary luminology: the dissociation between clinical and angiographic findings in ischemic heart disease. Circulation 1995;92:2333-2342
21. Ginghină C, Patriche M, Chreih R, Popescu BA, Deleanu D, Noi perspective privind microcirculația coronariană Rev Med Chir Soc Med Nat Iași 2008;112(3):711-718
22. Modavu I, Deleanu D, Chreih RM, Ginghină C, Semnificația circulației colaterale coronariene asupra prognosticului pacienților cu STEMI revasculariați prin angioplastie coronariană Revista Română de Cardiologie 2009;25(1)1-8
23. Apetrei E, Rugină M, Jurcuț R, Ce trebuie să știți despre infarctul miocardic? Ghidul pacientului Editura Medicală Antaeus, București 2006
 This work is licensed under a
This work is licensed under a