P. Ionescu, Meda Angheluș, Ioana Dinu
1 County Emergency Hospital of Bacău
Contact address:
Paul Ionescu, County Emergency Hospital of Bacau
Summary
“Masked hypertension” is a relatively new entity in the high blood pressure, for which the only way to highlight it is the ambulatory blood pressure (BP) monitoring/24h in the context of a high clinical suspicion. For many of the today patients, the stress of the medical consulting which is the essence of the well-known “white coat hypertension” is much exceeded by the daily stress especially that related the work1. The patient we present is a typical example of “masked hypertension” due to a combination of stress and a disease which is becoming more common lately: sleep apnoea. Modern methods of diagnosis of sleep apnoea and also the accessibility made diagnosis possible in the context of a high clinical suspicion. Recent clinical studies proving important link between cardiovascular disease and sleep apnoea syndrome more than common risk factors, providing explanation of inexplicable nocturnal cardiovascular events: arrhythmia, night hypertension, sudden death2.
Case Presentation
44 year old patient with no subjective complaints comes to a cardiology outpatient consultation after a periodic occupational health consulting which highlighted moderately increased blood pressure (BP 145/95 mmHg). The patient has no significant personal history and from the family history we notice that his father died suddenly at 51 years. As for his life style, we face a dynamic patient, authoritative, irritable, and permanently voyaging across the country and abroad, involved in multiple projects, heavy smoker, especially during the nights, chronic alcohol consumer (~150-200 ml alcohol/day). The patient also speaks about insomnia, nightmares linked to the payment of debts and to the many projects he is involved with a family climate threatened by stress, irritability, travels and lately “long snore, stop breathing sometimes and wakes often” reported by his wife.
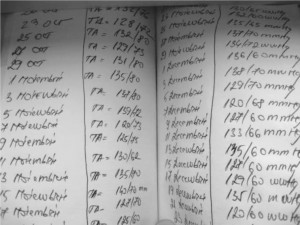
Clinical examination reveals a patient with moderate obesity (body mass index 32) and blood pressure between limits at the moment of the examination (BP 135/80 mmHg) with no other alterations. We notice that our patient is strongly influenced by the fact that he is approaching the age when his father suddenly died and he is obsessed of measuring blood pressure at home (all normal) (Figure 1).
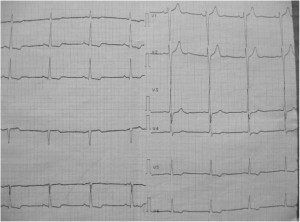
The electrical circuit reveals Synusal Rhythm 70/min, axe QRS 60°, left ventricular hypertrophy (LVH) with secondary terminal modifications (Figure 2). The electrical aspect of the left ventricular hypertrophy is confirmed by the echocardiography examination that shows left cavities to the upper part of the normal limits, Left ventricle (LV) 41/60 mm, Left atrium (LA) 44 mm, concentric left ventricular hypertrophy, interventricular septum (IVS) 15 mm, left ventricle posterior wall (PWLV) 14 mm without segmental kinetic disorders, with global systolic function to the lower part of the normal limits (EF 55%), alterated relaxation type diastolic dysfunction, moderate aortic atheromatosis, right cavities non dilated, normal valvular apparatus, without pericardial fluid (Figure 3, 4).
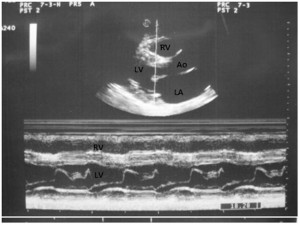
Figure 3. Echocardiography, parasternal long axis, M mode, showing left ventricular hypertrophy and a preserved segmentary systolic function.
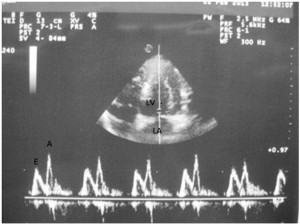
Figure 4. Mitral inflow velocities showing a pattern of grade 1 diastolic dysfunction (impaired relaxation and normal filling pressure).
Biological profile reveals carbohydrate and lipid metabolism in limits (glucose 0.96 mg%, Cholesterol 178 mg%, Low Density Lipoprotein (LDL) 110 mg%, triglycerides 145 mg%), creatinine 0.9 mg%, uric acid 6.8%, normal ionograma, micro albuminuria 140 mg/24h.
We are facing a patient with left ventricular hypertrophy electrical and in ultrasound examination, micro albuminuria but presenting normal blood pressure values during the clinical examination and also during the self-measurements made at home. As the hypertrophy of athlete was excluded from history, hypertrophic or dilated cardiomyopathy and aortic stenosis “clinical silent” were not identified by ultrasound, the clinical suspicion is masked hypertension, and for confirmation, it is necessary to monitor ambulatory BP/24 hours.
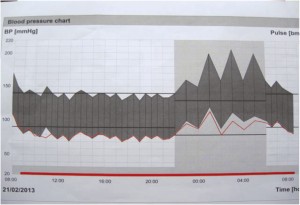
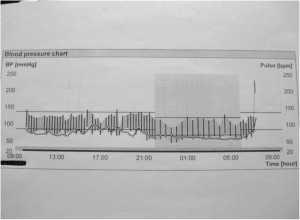
The blood pressure graphic obtained (Figure 5) points out an obviously non-dipper profile tension, with blood pressure values during the daytime of 142/84 mmHg and at night of 178/112 mmHg, hypertensive load during the day at 12% and at night at 100%. The tensional non-dipper profile is associated more frequently with left ventricular hypertrophy, stroke, peripheral arterial disease, albuminuria and cardiovascular mortality. From the circumstances frequently associated with non-dipper profile, some are obviously excluded in this case (preeclampsia, malignant hypertension, diabetic neuropathy), some are excluded after the targeted anamnesis (immunosuppressant such as medication use, corticosteroid, sympathomimetic). As for the secondary hypertension, this was not confirmed by abdominal ultrasound examination which revealed normal kidney size, symmetry, normal urinary ionograma and urinary metanephrines. Sleep apnoea is also one of the causes of secondary hypertension, often associated with non-dipper profile tension, also confirmed by the clinical data. The nocturnal ventilatory polygraphy recommended of the Department of Pneumology confirms the diagnosis of sleep apnoea syndrome (Figure 6) and establishes the indication of night ventilatory assistance with positive expiratory pressure3.
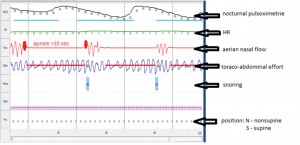
Figure 6. Nocturnal ventilatory polygraphy showing obstructive sleep apnoea with no aerian nasal flow but movements toraco-abdominal.
The diagnosis at this time is:
- Essential 2nd degree hypertension, high added risk (masked hypertension)
- Sleep apnoea syndrome
- 1st Degree Obesity
The therapeutic recommendations implies first, hygienic-dietary measures, significant change in lifestyle including non-smoking, weight loss, physical exercise, reduced alcohol consumption. Taking into account that lifestyle change is extremely difficult to obtain and requires a perfect psychological balance and family support, his wife was called to understand the necessity of lifestyle changing and the importance of the family support. Psychological counselling sessions was also started4,5.
Hypertension medical treatment includes at first angiotensin receptor blockers (ARBs) given the secondary organ damage (micro albuminuria and left ventricular hypertrophy). Knowing that in patients with high blood pressure values and associated risk factors it is difficult to achieve blood pressure control with monotherapy, we preferred a combination with a calcium channel blocker, based on the results of Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT), ABPM subgroup considering its role in controlling night blood pressure6. Considering the patient’s psychological profile and also his tension profile we preferred a fixed combination administered in small doses during the evening.
Regarding the sleep apnoea syndrome, it was initiated a night ventilatory assistance at home with positive expiratory pressure as recommended by the Department of Pneumology, but unfortunately not tolerated by the patient in spite of the repeated adaptation of the parameters.
As an additional advice we underline the effort of discouraging the obsessive self-blood pressure measurement at home, pointing out the doubts concerning the quality of the equipment used, and especially the patient’s anxiety that can lead to the self-modifying of the treatment.
The patient’s evolution was good, he adopted the hygienic-dietary measures and therapy at a satisfactory level, the awareness of the family support and the psychological counselling were very important given the family history. ABPM/24h control performed 3 months after the treatment started reveals a tension profile also non-dipper, but with a noticeably improved night profile (Figure 7).
Discussion
Masked hypertension is a relatively new subcategory of hypertension, diagnosed more and more often because both of stress increasing and of the access to modern methods of diagnosis. It should be considered every time we are in front of unexplained LVH. This form of hypertension is usually diagnosed late and therefore the target organ is more severe damaged. Ambulatory BP monitoring is the only solution for these patients to confirm the suspected diagnosis, being necessary for initiating therapy and improved prognosis7. Sleep apnea may also be envisaged at patients with non-dipper profile tension and smokers patients to whom history can support targeted clinical vigilance.
Conflict of interest: none declared.
References:
1. Bobrie G, Clerson P, Ménard J, Postel-Vinay N, Chatellier G, Plouin PF. Masked hypertension: a systematic review, Journal of Hypertension, September 2008, Volume 26, Issue 9, 1715-1725.
2. Somers VK, White DP, Amin Raouf, Abraham WT et al. Sleep Apnoea and Cardiovascular Disease, Expert Consensus Document, J Am Coll
Cardiol. 2008;52(8):686-717.
3. Aidar NA, Carvalho da Silva MA, Melo e Silva CA, Ferreira Jr PN, Tavares P. ABPM in COPD patients with sleep desaturation, Arquivos Brasileiros de Cardiologia, vol. 93, no.3, São Paulo Sept. 2009.
4. Mancia G, Fagard R, Narkiewicz K et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension. J Hypertens; 2013; 31: 1281-1357.
5. Perk J, De Backer G, Gohlke H et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012).Eur. Heart J; 2012, doi:10.1093/eurheartj/ehs092
6. Sever PS, Chang CL, Gupta AK, Whitehouse A. The Anglo-Scandinavian Cardiac Outcomes Trial, European Heart Journal 2011, 32 (20): 2525-2532.
7. Ohkubo T, Kikuya M, Metoki H, et al. Prognosis of “Masked” Hypertension and “White-Coat” Hypertension Detected by 24-h Ambulatory Blood Pressure Monitoring; J Am Coll Cardiol. 2005;46(3):508-515.
 This work is licensed under a
This work is licensed under a