Maria Meda Angheluş
County Emergency Hospital of Bacau
Angheluş Meda Maria, MD, County Emergency Hospital of Bacau
Summary: Sudden cardiac death is associated with the emergency services and intensive coronary therapy unit. We present a case similar to the thousands of cases seen daily in cardiology outpatient clinics, a 52 years patient in apparently healthy with multiple cardiovascular risk factors (hypertensive, dyslipidemic, obese and smoker) with partial compliance treatment and high variations of blood pressure, which despite an adequate treatment and a favorable initial evolution dies suddenly while talking on the phone. Besides the philosophical and spiritual aspect for us as humans in front of this case, we are facing a very important medical problem regarding the attention and concern that we, as doctors, have to pay each patient apparently healthy, who steps into our cabinet, even just for a routine consult!
Case presentation
52 year old patient with high blood pressure values (max anamnestic 180-200/100-110 mmHg BP) with intermittent treatment and ventricular extrasystole arrhythmia treated intermittently with propafenone 2 cp/day is coming for a routine cardiological evaluation during the annual medical balance.
We notice some dizziness, palpitations and headache all moderate in intensity and frequency that motivate the patient’s detached attitude on the history or cardiovascular disease. He doesn’t describe retrosternal pain or exertional dyspnea. He is considering him self to be in good health and during a period of high physical activity and mental efficiency, showing for a routine cardiological evaluation.
The cardiovascular clinical examination is normal with BP 140/80 mmHg, FC 75/min, rhythmic heart sounds, without murmurs, with no signs of IC, peripheral pulse present bilaterally symmetrical.
As family history, we have notice: diabetic mother, with hypertension, stroke, father without known heart disease, two healthy brothers and a 17-year-old daughter with common atrioventricular canal and surgical correction during childhood that represent the reason for the family annual cardiology consultation. Among the cardiovascular risk factors we mention hypertension, dyslipidemia (total Cholesterol 280 mg/dl, HDL C 28 mg/dl, triglycerides 158 mg/dl, LDL C 180 mg/dl), obesity (Weight 120 kg, T 1.92 m, BMI 33.2 kg/m2, abdominal circumference 124 cm), smoker (one pack / day for 25 years). Except the lipid profile, the biological balance is normal (Cr 1.1 mg / dl, glucose 90 g /dL, liver enzymes, complete blood count and ionograma in normal limites).
The ECG reveals 95/min sinus tachycardia, left axis, left ventricular hypertrophy and isolated premature heart beat (Fig. 1). The echocardiography exam reveals normal cavities, moderate concentric left ventricular hypertrophy (IV septum 14 mm, posterior wall 13 mm, LV mass 136 g/m2), preserved global systolic function (EF 70%), delayed relaxation type diastolic dysfunction without signs of pulmonary hypertension without pericardial fluid, valves with normal morphology and function (Figure 2, 3, 4).

Figure 1.
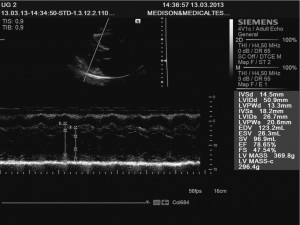
Figure 2. Transthoracic echocardiography -long axis parasternal view of the left ventricle.
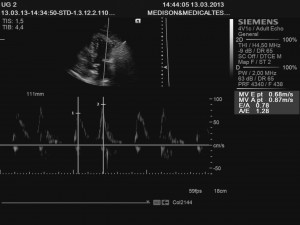
Figure 3. Transthoracic echocardiography -transmitral flow velocity patterns to left ventricular diastolic function.
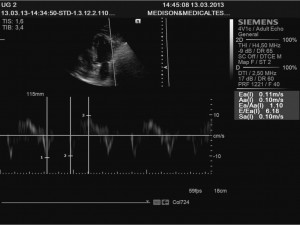
Figure 4. Transthoracic echocardiography -Tissue Doppler imaging.
The diagnosis is 3rd degree hypertension very high added risk, dyslipidemia,1st degree obesity, extrasystolic ventricular arrhythmia. Treatment recommendations include, first, cover hygienic-dietary measures plus medical treatment with beta blockers (bisoprolol 5 mg), ACEI (perindopril 5 mg), antiplatelet (aspirin 100 mg) and statin (atorvastatin 10 mg).
The cardiological balance was completed with urinary metanephrines and urinary ionograma which proved to be normal, abdominal echography that revealed normal kidney size, symmetry. 24hr Holter ECG monitoring justified by the history of extrasystole arrhythmia and antiarrhythmic therapy objectifies permanent sinus rhythm with rare ESV (27/24 h) without sustained arrhythmias or conduction disturbances. The 24 h ambulatory monitoring of blood pressure values marked variability, non-dipper profile tension, maximum tension values 180/110 mm Hg and average pressure values 140/90 mmHg (Fig. 5).
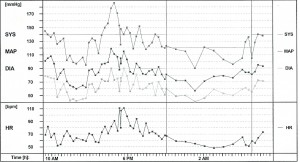
Figure 5.
After a month, we notice a good tolerance of the treatment, marked variability both on MAPA basis and anamnestic, systolic values widely varying between 120 and 170 mmHg and a slight improvement of the clinical symptoms, BP 130/80 mmHg and AV 65/min in the objectif exam.
Despite the partial compliance to the drug treatment, the hygienic-dietary measures and the active participation in the discussions, the patient keeps a detachment, relaxation and even disinterest on a possible heart condition. To increase the patient’s awareness for the treatment and of the risk factors control, we analyzed together the SCORE chart for fatal CV event risk at 10 years, which was 12% in his case.
Given the current data on the role of calcium channel blockers in reducing blood pressure variability and its negative prognostic role, the treatment was adjusted by adding Amlodipine 5 mg.
After 3 months we’ve got a relatively good control of blood pressure, which varies between 120 and 150 mmHg TAs and of biologically improving lipid profile (total chol 210 mg / dl, HDL chol 32 mg/dl, LDL chol 109 mg/dL, TG 150 mg/dl), creatinine 1.2 mg/dl and hepatic enzymes unchanged after the statine treatment.
After about 1 year of evolution apparently favorable with the above-mentioned treatment, possibly intermittent, partial compliance with hygienic-dietary measures prescribed (5 kg weight loss, walking to work and diet but without giving up smoking) the patient died suddenly during the evening, while talking on the phone.
Discussion
The percentages presented in the diagram SCORE on fatal CV event risk is not abstract. The patient is, unfortunately, one of the cases proving negative prognostic value associated with BP variability. This case also reminds us once more that sudden cardiac death is a reality in clinical practice even for patients who are in a state of apparently health.
An important role in the unfortunate outcome of the patient can have his detached attitude concerning his cardiovascular risk that is probably related to therapeutic discontinuities which emphasized the natural tendency to the variability of the blood pressure. This is why each of us has to get more involved in the patient’s awareness of the disease, not only in diagnosis and treatment, and we have to share with our patients the responsibility for the adherence to the treatment.
Conflict of interests: The authors declare that no conflict of interest exists.
 This work is licensed under a
This work is licensed under a