Zoltán Salló1, Nándor Szegedi1, István Osztheimer1, Vivien Klaudia Nagy1, Katalin Piros1, Péter Perge1, Tamás Tahin1, Pál Ábrahám1, Béla Merkely1, László Gellér1
1 Semmelweis University, Cardiovascular Center, Budapest, Hungary
INTRODUCTION
Catheter ablation is a well established treatment in atrial fibrillation (AF). Pulmonary veins (PV) play an important role as arrhytmia triggers in AF1 , therefore PV isolation became a standardized strategy in the treatment of AF. Electroanatomical mapping seems to have important role in the identifi cation of the appropriate ablation sites2-4. PV isolation could be challenging in patients after pneumonectomy, due to the changes in the anatomical position of the heart.
CASE REPORT
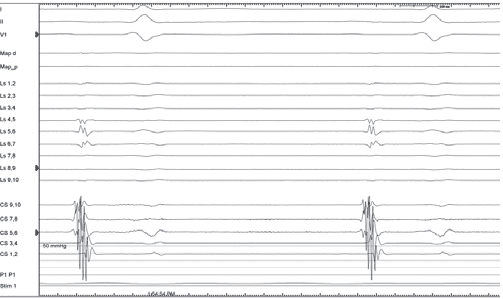
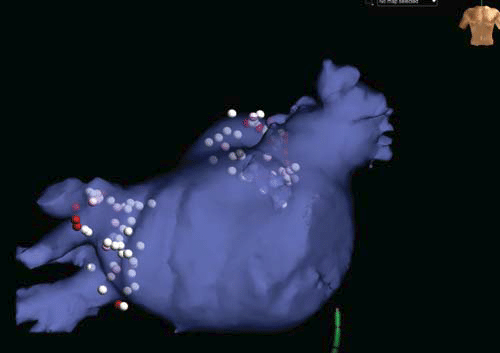
We present a case of a 64-year-old male patient who has symptomatic paroxysmal AF for almost 2 years, despite anti-arrhytmic treatment. Seven years ago, complete left-sided pneumonectomy was performed for resection of tumor (small cell lung cancer). Considering the risk of thromboembolism (CHA2DS2-Vasc score = 2) warfarin was administered. Prior the ablation procedure the left atrial (LA) anatomy was assessed via 256-slice computed tomography, which showed PVstumps on the left side. The ejection fraction (55 %) and the LA dimensions (39×37 mm) was measured by transthoracic echocardiography. Prior the transseptal puncture, LA thrombus was excluded by intracardiac echocardiography (ICE). Catheter position inside the coronary sinus indicated unusual post-operative cardiac position. After the two transseptal punctures, which was guided also by ICE, an ablation catheter (AlCath Flux Blue G eXtra, Biotronik) through a steerable sheath (Agilis NXT, St. Jude Medical), and a diagnostic ’lasso’ catheter (Inquiry Optima 10 pole, St. Jude Medical) through a transseptal sheath (Swartz SL0, St. Jude Medical) were introduced into the left atrium. A three-dimensional LA fast anatomical map was performed (EnSite Velocity, St. Jude Medical). The lasso catheter was inserted into the PVs and recorded PV signals in all PVs including PV stumps. Circumferential radiofrequency lesions (30W, 20 mL/min) were made isolating both ipsilateral PVs (full ablation time = 2302sec). Entrance and exit blocks were verified in all PVs. In both left PV stumps, which were electrically active before the procedure, complete isolation was obtained after the radiofrequency ablation. In the PV remnants, frequent electrical discharges with subsequent exit block were observed. Fluoroscopy and procedure time was 12.1 and 90 min, respectively. No recurrence of AF was observed until the 6 months check-up (24 h Holter after 3 months).
DISCUSSION
Our report describes a technically challenging case of pulmonary vein isolation after complete left-sided pneumonectomy. In this situation, it was crucial to identify the PV ostia carefully, to avoid right PV stenosis. The merge of the preoperative CT and the electro-anatomical map might have a great importance in a special patient like this. In our patient, all PVs were electrically active, including the PV remnants – such as in a multicenter study5 – and we sucessfully isolated all of them. The observation that after the ablation, the PV remnants showed electrical activity with exit block, further supports the importance of PVI as a main endpoint in the ablation strategy of AF.
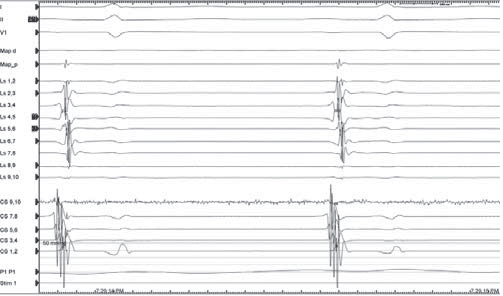
Figure 1. Fast anatomical map (FAM, on the left) and CT angiography (CTA) image (on the right) of the left atrium
Figure 2. EGMs on the lasso catheter placed into the left sided PV stumps, before the ablation. The PV stumps are electrically active.
Figure 3. EGMs on the lasso catheter placed into the left sided PV stumps, after the successful ablation. Only far fi eld EGMs are visible on the lasso catheter
Figure 4. Ablation points after the procedure on the merged map (FAM and CTA).
CONCLUSION
Catheter ablation of AF in patients with pneumonectomy is feasible and safe procedure. Due to the difficulties in the anatomy, it could be technically challenging, and the appropriate identification of the PV anatomy seems to be crucial to identify the PV ostia and to isolate the PV stumps also.
Conflict of interest: none declared.
References
1. Haissaguerre, M., et al., Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med, 1998. 339(10): p. 659-66.
2. Szegedi, N., et al., Radiofrequency ablation of focal atrial tachycardia: Benefi t of electroanatomical mapping over conventional mapping. Acta Physiol Hung, 2015. 102(3): p. 252-62.
3. Szeplaki, G., et al., Respiratory gating algorithm helps to reconstruct more accurate electroanatomical maps during atrial fibrillation ablation performed under spontaneous respiration. J Interv Card Electrophysiol, 2016. 46(2): p. 153-9.
4. Ozcan, E.E., et al., Isolation of persistent left superior vena cava during atrial fibrillation ablation. Indian Pacing Electrophysiol J, 2015. 15(2): p. 130-2.
5. Kanmanthareddy, A., et al., Pulmonary vein isolation for atrial fibrillation in the postpneumonectomy population: a feasibility, safety, and outcomes study. J Cardiovasc Electrophysiol, 2015. 26(4): p. 385-9

 This work is licensed under a
This work is licensed under a