Marin Postu1, I. Calin1, A. Postu-Plugaru2, Adrian Bucsa1, Lucian Zarma1, Marian Croitoru1, Pavel Platon1, Dan Deleanu1
1 Emergency Institute for Cadiovascular Diseases “Prof. Dr. C. C. Iliescu”, Bucharest, Romania
2 ARES Centers for Excellences in Interventional Cardiology and Radiology, Bucharest, Romania
Contact address:
Marin Postu, MD
Emergency Institute for Cadiovascular Diseases “Prof. Dr. C. C. Iliescu”
Sos. Fundeni 258, sector 2, 022328. Bucharest, Romania
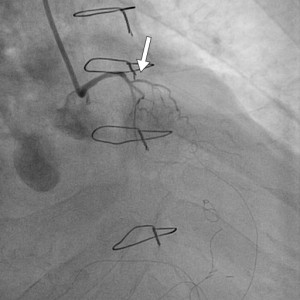
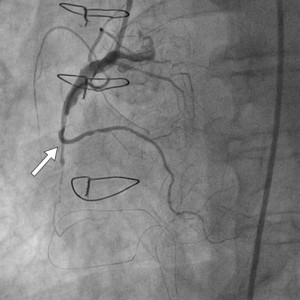
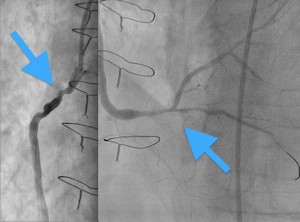
We present a case of a 79 years old male, with CABG intervention 12 years ago, admitted with inferior STEMI, 5 hours from onset. At that time, the patient was in a critical condition, presenting acute pulmonary edema and impaired ventricular rhythm in the form of sustained ventricular tachycardia. The coronary angiography demonstrated chronic total occlusions (CTO) of both native vessels (Figure 1, 2), functional bypass at the left anterior descending artery (LAD) level with left interior mammary artery (LIMA) (Figure 3), the absence of circumflex artery bypass, and acute thrombotic occlusion of the saphenous vein grafts (SVG) bypass for right coronary artery (RCA) (Figure 4).
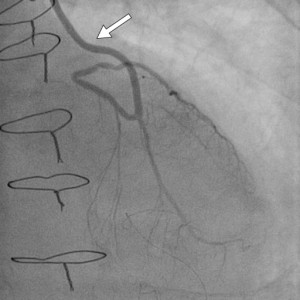
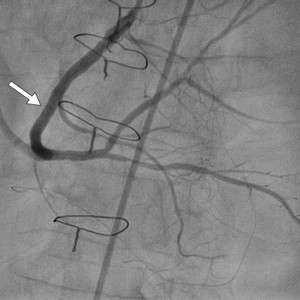
Figure 3. Permeable left interior mammary artery (LIMA) (arrow) to left anterior descending artery (LAD).
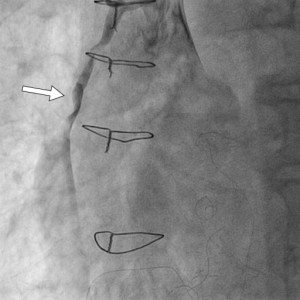
Figure 4. Thrombotic occlusion on the saphenous vein grafts (SVG) bypass for right coronary artery (RCA).
First, manual thromboaspiration with 6 Fr catheter was performed, with extraction of thrombotic material. The resumption of distal flow in the native vessel through SVG was obtained; however, significant stenosis in the proximal segment and at the distal anastomosis of the bypass persisted (Figure 5). Our decision was to postpone the stent implantation1,2. We started anticoagulant therapy and decided to repeat coronary angiography after 2 days.
Following PCI, patient was stable, with a good evolution. After treatment with anticoagulants the patient was readmitted to cath-lab for angiographic control. Because of high distal embolization risk, known on the intervention on the bypass3, the PCI for CTO on RCA was decided. After crossing occlusion zone with hydrophilic guide wire and predilatation, 3 stents were implanted with very good final result (Figure 6). The patient was discharged after 8 days of hospitalization, hemodynamically stable, asymptomatic with LVEF 35% and grade II mitral regurgitation.
Conflict of interests: none declared.
References:
1. Carrick D, Oldroyd KG, McEntegart M, et al. A randomized trial of deferred stenting versus immediate stenting to prevent no- or slow-reflow in acute ST-elevation myocardial infarction (DEFER-STEMI). J Am Coll Cardiol. 2014;
2. Xavier Freixa, MD; Loic Belle, MD; Lawrence Joseph, PhD; Jean-François Tanguay, MD; Géraud Souteyrand, MD; Philippe L. L`Allier, MD; E. Marc Jolicoeur, MD, MSc, MHS. Immediate vs. delayed stenting in acute myocardial infarction: a systematic review and meta-analysis. EuroIntervention 2013;8
3. Michael S. Lee, MD; Seung-Jung Park, MD; David E. Kandzari, MD; Ajay J. Kirtane, MD, SM; William F. Fearon, MD; Emmanouil S. Brilakis, MD, PhD; Paul Vermeersch, MD; Young-Hak Kim, MD; Ron Waksman, MD; Julinda Mehilli, MD; Laura Mauri, MD; Gregg W. Stone, MD. Saphenous Vein Graft Intervention. J Am Coll Cardiol Intv. 2011;4(8):831-843. doi:10.1016/j.jcin.2011.05.014
 This work is licensed under a
This work is licensed under a