Alina Oprescu*, Emanuel Stoica*, Daniela Anghelina*, Dan Deleanu*, Cristina Popică*, Iulian Călin*, Mihaela Rugină*, Carmen Ginghină*, Eduard Apetrei*
* “Prof. Dr. C. C. Iliescu” Emergency Institute of Cardiovascular Diseases from Bucharest
CASE 1
D.E – woman, 57 years old, presentation at 8:30 am. Diagnosis: Acute coronary syndrome with ST segment elevation in the inferior-posterior-lateral territory at 3 hours Killip class I, Mild mitral regurgitation, Grade II essential arterial hypertension with high additional risk, Chronic smoking, Obesity, Dyslipidemia. Cardiovascular risk factors: arterial hypertension, smoking, obesity. Retrosternal pain onset 3 hours prior to presentation, accompanied by nausea and vomiting. Affirmative in-between episodes of angina the day prior to presentation. Clinical examination: hemodynamically stable, BP = 160/90 mmHg, HR (heart rate) = 55/min, without cardiac murmurs, without systemic or pulmonary congestion. ECG on admission: sinus rhythm (SR) with heart rate (HR (heart rate)) = 55/min, ST-segment elevation in DII, DIII, avF, V5-V9. 10 minutes after presentation a third-degree atrioventricular block is with HR (heart rate) = 35/min and systolic hypotension = 80 mmHg, Atropine 1 mg is administered i.v. with resumption of sinus rhythm with HR (heart rate) = 80/min. Echocardiography on admission: ejection fraction (EF) = 50%, akinesia of the apex, inferior wall and 1/3 bazal lateral wall, mild mitral regurgitation. Laboratory tests: positive troponin (1.90 ng/ml), NTproBNP = 389 pg/ml. Coronary angiography reveals 70% stenosis of right coronary artery (RCA) in segment III with an appearance of unstable plaque and thrombus, primary angioplasty with stent placement is performed at this level with good fi nal result, without any peri-procedural complications. On the Holter EGG monitoring she did not repeat the atrioventricular block episodes. Subsequent evolution was favorable, without angina, without heart failure symptoms.
CASE 2
R.F – man, 57 years old, presentation at 9:15 am Diagnosis: Acute coronary syndrome with ST segment elevation in the inferior territory and right ventricle at 3 hours Killip class IV, Transient third degree atrioventricular block, Grade III Mitral regurgitation, Grad II Tricuspid insufficiency, Grade III essential arterial hypertension with high additional risk, Smoking. Cardiovascular risk factors: arterial hypertension, smoking Retrosternal pain onset 3 hours prior to presentation, accompanied by cold sweats, pain with paresthesia and abolition of sensibility in the left calf. Note that the patient does not present a history of intermittent claudication. Clinical examination: mediocre general condition, conscious, cooperative, BP=80/40 mmHg, HR (heart rate)=41/min, grade II/VI systolic murmur in the mitral area, weak femoral pulse in the right femoral artery and absent in the left femoral artery, without systemic or pulmonary congestion Echocardiography on admission: EF=45%, basal inferior wall and 1/3 posterior wall akinesia, dilated (45 mm) right ventricle (RV) with global systolic dysfunction, grade III mitral regurgitation, grade II tricuspid regurgitation, pulmonary artery systolic pressure (PAPs)= 42 mmHg. Laboratory tests: positive troponin (2.5 ng/ml), NTproBNP 7500 pg/ml In the catheterisation lab the patient develops grade III atrioventricular block with HR (heart rate)=35/min and BP= 80/40 mmHg, requiring a temporary pacing to be performed before the start of coronary angiography.
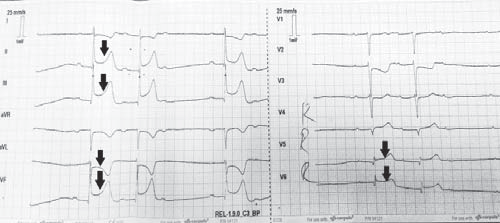
Figure 1. ECG on admission: junctional rhythm with HR (heart rate)= 41/minute, ST- segment elevation in DII, DIII, AVF, V3R-V4R, ST-segment depression in avL.
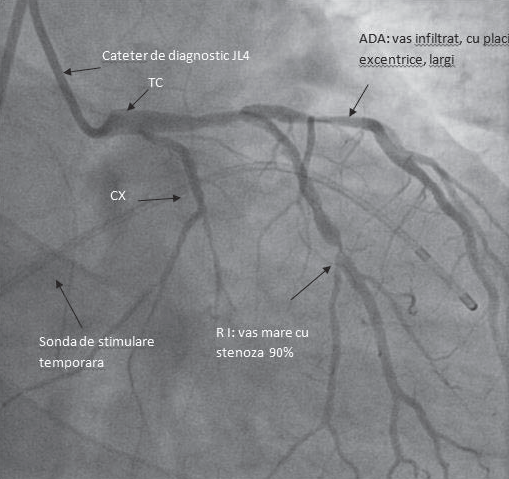
Figure 2. RAO (20°) caudal (29°) incidence. Atheromatous inflitration of the left main (LM). CXA – small caliber vessel (hypoplastic). Intermediary branch with a large caliber has a 90% focal stenosis in the medium segment. ADA- atheromatous infiltrated vessel in the proximal and the medium segments with excentric plaques without significant stenosis. This incidence
is used to study the LM, CXA, the intermediary branch and the proximal segment of the ADA (the lesions in the middle segment of ADA are oft en over-estimated).
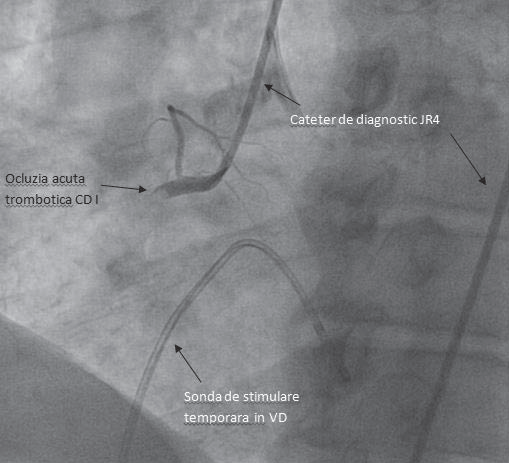
Figure 3.LAO (34°) incidence: acute thrombotic occlusion of the proximal RCA(right coronary artery).
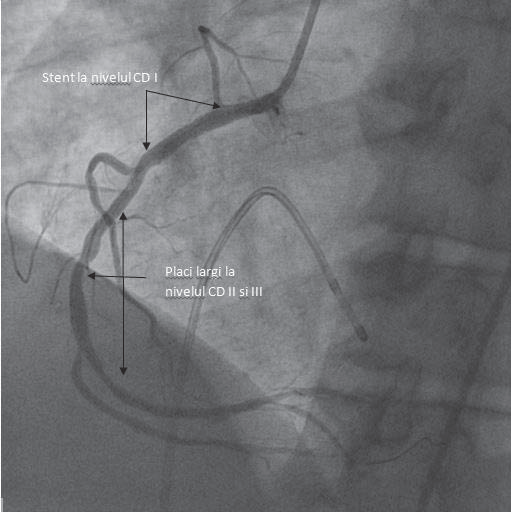
Figure 4.RAO (30°) incidence: Very good final result after implantation of a stent at the RCA proximal level. In the medial and distal segments the vessel is infiltrated with small plaques with a stable aspect, which don’t require stents.
The coronary angiography reveals acute thrombotic occlusion of the right coronary artery (RCA) (Figure 3), thromboaspiration with primary angioplasty with stent at the level of RCA is performed with a good final angiographic result (Figure 4), without peri-procedural complications. The patient has remaining lesions in the anterior descending artery, 60-70% stenosis on bifurcation with the first diagonal (Dg 1), 90% stenosis Dg 1 in the middle segment and 40% stenosis in the circumflex artery ostium, but with no indication for revascularization at this time (Figure 2). In the catheterization lab the patient claims pain in the left lower limb, aggravated gradually, followed by paresthesia, hypoesthesia and functional impotence. The skin of the left thigh, and foot were marbled, cold, with abolished sensitivity and mobility in the foot; left femoral artery pulse was absent. Vascular surgery consultation is sought (MD Claudiu Vasile), who considers this episode to be caused by an acute ischemia due to low cardiac output and recommends hemodynamic rebalancing and heparin therapy. The vascular Doppler ultrasound performed afterwards revealed that the cause of this complication was a significant stenosis of the left tibioperoneal trunk, overlapped by the low cardiac output. After angioplasty the patient resumed the sinus rhytm, for which reason pacing was suppressed. Subsequent evolution was favorable, without angina, without heart failure symptoms. The episode of acute ischemia in the left lower limb resolved after resolution of hypotension and heparin therapy.
CASE 3
N.E, woman, 60 years old, presentation at 9:30 am. Diagnosis: Unstable angina, Bicoronary lesions of borderline hemodynamic significance, Major left bundle branch block (LBBB), Grade II essential arterial hypertension, Very high additional risk, Dyslipidemia, Obesity, Lumbar discopathy. Cardiovascular risk factors: overweight, arterial hypertension, diabetes. Pathological personal history: bicoronary lesions of borderline hemodynamic significance (2010) (40% stenosis of anterior descending artery (ADA) II, 60-70% stenosis of diagonal artery (Dg) I, 50% stenosis of marginal artery (Mg) in segment I), LBBB. Precordial pain like a „claw” on effort and at rest, worsened in the last week. Clinical examination hemodynamically stable, BP = 120/60 mmHg, HR (heart rate) = 80/min, rhythmic heart sounds, without cardiac/vascular murmurs, pulsatile peripheral arteries, without pulmonary or systemic congestion. ECG on admission: sinus rhythm, HR (heart rate) = 75/min, QRS axis = -45 degrees, LBBB (160 ms) with secondary changes in repolarization phase. Laboratory tests: negative troponin; NTproBNP 157 pg/ml. Modified basal glycaemia. Echocardiography on admission: nondilated left ventricle with concentric hypertrophy (interventricular septum = 15 mm, posterior wall = 14 mm) with preserved global systolic function (EF-50%). Apical hypokinesia. Diastolic dysfunction type delayed relaxation. No hemodynamically significant valvulopathy. Coronary angiography is indicated for risk stratification in patients with severe stable angina (Canadian class 3) or occurring in patients that present a high risk profile for cardiovascular events, especially if the symptoms do not respond adequately to drug therapy – Class of recommendation I, level of evidence C1. In our patient it was decided to perform coronary angiography 48 hours after admission, which revealed a stationary aspect of coronary lesions, thus choosing for optimizing the drug therapy. Evolution was favorable under drug therapy without recurrence of angina.
CASE 4
M.G, man, 68years old, presentation at 10:00 am Diagnosis: Acute coronary syndrome with ST segment elevation in the inferior territory at 11 hours Killip class I, Grade II-III Mitral regurgitation, Grade II essential arterial hypertension high additional risk. Risk factors: arterial hypertension, gender, age. Angina for about 3 days, he presents for intense epigastric pain accompanied by sweating and breathlessness, for 11 hours ago, a retrosternal painful discomfort persists upon presentation. Clinical examination: hemodynamically stable, BP = 160/100 mmHg, HR (heart rate) = 80 b/min, systolic murmur grade 3/6 in the mitral focus, without pulmonary or systemic congestion. ECG on admission: RS, HR (heart rate) = 80 b/min, ST-segment elevation stage DII, DIII, avF. Echocardiography on admission: normal sized left ventricle, EF=50%, inferior wall akinesia and 2/3 basal interventricular septum, mitral regurgitation grade II-III. Coronary angiography revealed tricoronary lesions (ADA: 60% stenosis in the proximal segment, 80% stenosis with an appearance of unstable plaque and thrombus on the distal segment circumflex artery (CXA) before the emergence of the branch playing the role of posterior retroventricular artery (PRA), hypoplastic RCA with critical stenosis in the medium segment. Stent angioplasty was performed on the lesion held responsible on the CXA with a very good final result. Evolution was favorable during hospitalization, with no recurrence of the angina and without heart failure symtoms. The patient was taken on record for revascularization of the remaining lesions.
CASE 5
M E, woman, 90 years old, presentation at 10:20 am. Diagnosis: Acute cardiogenic pulmonary edema, Moderate aortic regurgitation, Moderate mitral regurgitation, Moderate tricuspid regurgitation, Grade III essential arterial hypertension with very high added risk, Stage V chronic kidney failure, Gastroduodenal ulcer, Normocytic hypochromic anemia. Risk factors: arterial hypertension, chronic kidney disease. Dyspnea with orthopnea, claiming retrosternal pain for about 3 days, refusing hospitalization at that time. Clinical examination: pale, conscious, BP = 177/114 mmHg, HR (heart rate)-120/min, rhythmic heart so un ds, diastolic murmur in the aortic focus, systolic murmur II/VI in the mitral focus, decreased left basal vesicular murmur, disseminated sibilant rales, wheezing, crackles bilaterally, discrete calf edema. Laboratory tests: NTproBNP >30000 pg/ml, slightly elevated troponin (0.112 ng/ml), leucocytosis with neutrophilia, normocytic hypochromic anemia, nitrogen retention (CrCl =13.4 ml/min/1.73m2). ECG on admission: sinus tachycardia with HR (heart rate) = 120/min, biphasic T waves V1-V3. Echocardiography on admission: normal sized left ventricle, biatrial dilatation, EF=45%, LV apex and apical 1/3 anterior wall akinesia. Grade III mitral regurgitation, grade III aortic regurgitation, grade III tricuspid regurgitation. Hypertensive patient with anemic syndrome presents herself for heart failure symtoms, probably caused by uncontrlled hypertension due to non-adherence to the treatment at home. She received anticoagulant therapy during hospitalization, loop diuretics, beta blockers, calcium channel blockers, antibiotics. Given the low value of hemoglobin (initial=7.2 g/dl, then 6.1g/dl) we decided to administer 2 units of erythrocyte mass which increased hemoglobin level to 10.4 g/dl. During in hospitalization the nitrogen retention syndrome maintained with an average of creatine clearance of approx. 12.47 ml/min. Evolution during hospitalization was favorable with improvement of dyspnea, disappearance of pulmonary congestion and improvement of her overall condition. The patient will be taken on record in the nephrology clinic on discharge.
CASE 6
S A, man, 55 years old, presentation at 4:30 pm. Diagnosis: Type A aortic dissection, Cardiac tamponade. Cardiovascular risk factors: therapeutically neglected arterial hypertension. Emergency hospitalization by transfer from Braila County Hospital with suspected type A acute aortic dissection, initially presenting himself with anterior chest pain accompanied by syncope. The echocardiography performed in Braila reveald a dilatation of the ascending aorta, aortic arch and circumferential pericardial fluid. Clinical examination on admission: lethargic patient without motor deficits, cold sweaty skin, breathing spontaneously, SpO2 =99% with extra O2, SBP= 70 mmHg under inotropic support with dopamine, HR (heart rate) = 90 bpm, bilateral femoral artery pulses present, hardly perceptible radial arteries. ECG on admission: sinus rhythm with HR (heart rate)-100/min, elements suggestive of left ventricular hypertrophy with secondary changes of terminal stage. The patient was transported to the ICU and monitored invasively (left femoral arterial catheter and central venous catheter) and noradrenalin pressor therapy was instituted for severe hypotension (SBP=55 mmHg). In hemodynamically unstable patients, the Aortic Dissection European Guide of 2014 indicates transesophageal echocardiography (class of recommendation I, level of evidence C) 2.
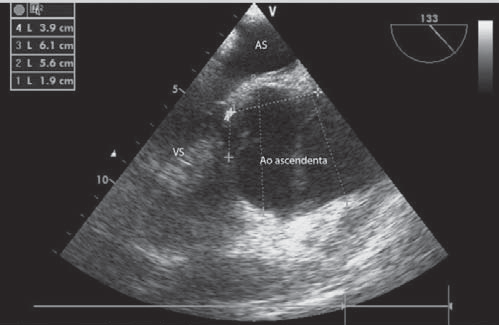
Figure 5. Transoesophageal echocardiography- midoesophageal section long axis at 133°- shows dilatation of the Valsalva sinuses(56 mm) and of the ascending aorta(61 mm). LA-left atrium, LV-left ventricle.
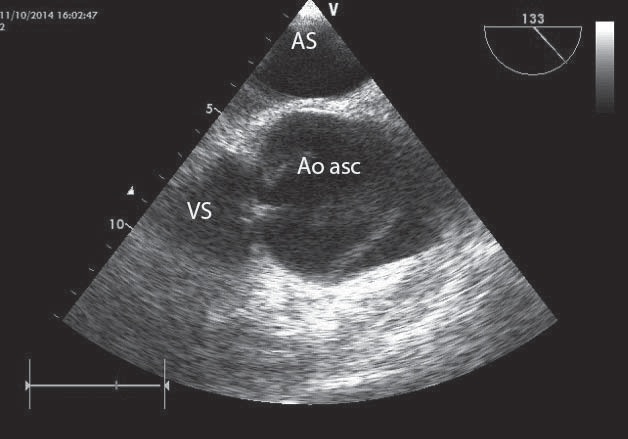
Figure 6. Transoesophageal echocardiography – mid-oesophageal section long axis at 133 degrees – shows a dissection flap at the level of the ascending aorta-linear echo at this level. LA-left atrium, LV- left ventricle.
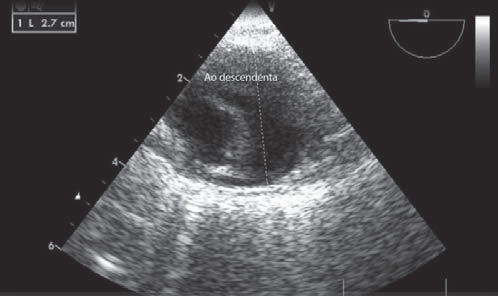
Figure 7. Transoesophageal echocardiography-transversal section at the level of the descending aorta 0 degrees- shows a dissection fl ap – linear anteroposterior echo which separates the true from the false lumen.
In the case of our patient transesophageal echocardiography was performed highlighting: dilatation of the aorta at the sinus of Valsalva and ascending aorta (Figure 5). Visible dissection flap 4 cm away from the aortic annulus (Figure 6). Descending aorta (27 mm) with dissection fold (Figure 7). In patients with type A aortic dissection the European Guide recommends its surgical cure (class I indication, level of evidence B) 2. Cure of acute ascending aorta dissection is performed by Bentall procedure (MD Cristi Voica): Replacement of the aortic valve and ascending aorta with valve conduit no. 27/30; coronary ostia reimplantation in the valve duct. Postoperatively, massive bleeding occurs on withdrawal of extracorporeal circulation without surgical solution. The patient is readmitted to intensive care with serious evolution marked by significant bleeding, marked hemodynamic instability SBP=70 mmHg under maximal inotropic and vasopressor support, metabolic acidosis with hyperlactatemia. Oliguria with hematuria, accompanied by severe hypotyension with bradycardia which lead to asystole unresponsive to resuscitation maneuvers followed by exitus.
CASE 7
D I man, 86 years old, presentation at 5:20 pm. Diagnosis: Acute coronary syndrome with ST segment elevation in the inferior territory at 11 hours Killip class I, Mild mitral regurgitation, Right bundle branch block (RBBB), Grade II essential arterial hypertension with very high added risk, Dyslipidemia. Cardiovascular risk factors: arterial hypertension, dyslipidemia. Retrosternal pain onset 11 hours ago, presenting himself initially at Sf. Pantelimon Hospital, he was subsequently sent to our clinic within the STEMI program. The patient claims the presence of angina episodes of short duration for approximately 3 weeks. Clinical examination on admission: average general state, conscious, cooperative, BP=130/70 mmHg, HR (heart rate)=63/min, without heart murmurs, vesicular murmur present bilaterally, without systemic or pulmonary congestion. ECG on admission: sinus rhythm with HR (heart rate)=63/min, RBBB, ST-segment elevation in DII, DIII, AVF Echocardiography on admission: nondilated left ventricle with EF=50%, inferior and posterior wall hypokinesia, mild mitral regurgitation. Laboratory tests on admission: positive troponin=0.99 ng/ml, NTproBNP=1482 pg/ml.The coronary angiography reveals a circumflex artery occlusion at the origin of the first marginal (Mg) and a primary angioplasty with a stent at this level is performed. A distal no-reflow phenomenon is found, deciding the implantation of a second stent proximal to the first one with obtaining a TIMI II flow, no periprocedural complications, having remaining lesions on 50% stenosis on left main, 75% stenosis on RCA II and 70% on ADA I. Evolution was favorable, without angina, without heart failure symptoms. The patient will be subsequently reassessed for determining the opportune timing for surgical revascularization of the remaining lesions.
CASE 8
MI. woman, 37 years old, presentation at 5:35 pm. Diagnosis: Myopericarditis. No significant pathological personal history, without cardiovascular risk factors. Pain of angina type for approx. 48 hours, intensified in the last 12 hours. Clinical examination on admission: hemodynamically stable, BP = 120/70 mmHg, HR (heart rate) = 80/min, rhy th mic heart sounds, pericardial friction rub, no signs of systemic or pulmonary congestion. Laboratory tests: positive troponin (4.2 ng/ml), normochromic, normocytic anemia. Inflammatory syndrome: increased C-reactive protein and fibrinogen, white blood cells within normal limits. Echocardiography on admission: normal sized left ventricle, EF=55%, posterior and 1/3 basal inferior wall hypokinesia, small quantity of pericardial fluid. Given the ECG aspect and positive troponin, and persistent pain we decided to do a coronary angiography to exclude possible coronary leasions. This highlighted permeable epicardial coronary arteries. We interpret the case as a myopericarditis with positive inflammatory biological samples, positive myocardial necrosis enzymes, permeable epicardial coronaries, with good evolution under anti-inflammatory therapy.
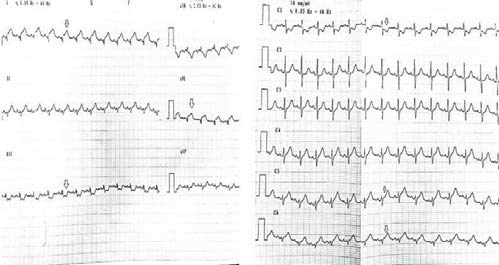
Figure 8. ECG: sinus rhythm, HR (heart rate)-80/min, narrow QRS, ST elevation of approx. 1 mm in the D1, AVL, V5-V6 derivations.
CASE 9
B G, man 59 years old, presentation at 5:40 pm. Diagnosis: Acute coronary syndrome with ST segment elevation in the anterior territory at 7 hours Killip class II, Thrombolysis after 2 hours, Newly discovered Type II Diabetes, Grade II mitral insufficiency, Chronic smoking. Cardiovascular risk factors: smoker, newly discovered diabetes. Transfer from Constanta County Hospital 7 hours after the onset of retrosternal pain. The patient underwent Rapylisine thrombolysis 2 hours after onset. Clinical examination: hemodynamically stable, BP=136/100 mmHg, HR (heart rate)=100 b/min, left ventricle ga llop, without pulmonary or systemic congestion. Laboratory tests: positive troponin (>50 ng/ml). ECG on admission: accelerated idioventricular rhythm, HR (heart rate)=100 b/min, RBBB, ST-segment elevation V1-V6. Echocardiography on admission: nondilated left ventricle with concentric (display); EF=35%; Akinesia of the anterior interventricular septum, apical 2/3 anterior wall, left ventricular apex. Grade II mitral regurgitation. Normal pericardium. Coronary angiography revealed 80% stenosis in the ADA II/III with an aspect of unstable plaque. A stent was implanted with good final result. Evolution was favorable during hospitalization, without repeating angina under therapy.
CASE 10
I E, woman, 73 years old, presentation at 8:15 pm. Diagnosis: Acute coronary syndrome with ST segment elevation in the inferior-posterior-lateral territory at 9 hours Killip class I, Thrombolysis 6 hours after onset with reperfusion criteria, Mild mitral regurgitation, Grade II essential hypertension with high additional risk, Obesity, Dyslipidemia, Diabetes controlled by diet Cardiovascular risk factors: Arterial hypertension, dyslipidemia, obesity, diabetes. Retrosternal pain onset 9 hours before presentation, she was diagnosed with myocardial infarction, with ST-segment elevation in the inferior-posterior territory that was thrombolysed 6 hours of onset, with clinical and electrical reperfusion criteria, she is sent to our clinic within the STEMI program. Clinical examination on admission: good general condition, conscious, cooperative, BP=130/80 mmHg, HR (heart rate)=55/min, without cardiac murmurs, without pulmonary or systemic congestion. ECG on admission: sinus rhythm with HR (heart rate)=55/min, ST-segment elevation in DII, DIII, AVF, V5-V9, decreased by approx. 50% compared to the initial ECGs. Laboratory tests: positive troponin (47.5 ng/ml). Echocardiography on admission: EF=50%, posterior wall and lateral will akinesia, mild mitral regurgitation. Coronary angiography reveals 80% stenosis of RCA in the proximal and medial segment, primary angioplasty is performed with 2 stents at the level of the lesions with a good final result, without peri-procedural complications. She has remaining lesions, 70% stenosis on ADA I and another 50-60% stenosis on ADA II. Evolution was favorable, without angina, without heart failure symptoms. The patient will return at a later time for the revascularization of the remaining lesions.
CASE 11
M D man, 50 years old, presented at 10:45 pm. Diagnosis: Acute coronary syndrome with anterior ST elevation at 2,5 hours Killip class II, Grade II Mitral regurgitation, Acute coronary syndrome without ST-segment elevation (NSTEMI)(04.2013) – angioplasty with stent on ADA-04.2013, Chronic smoking, RBBB with uncertain onset, Obesity, Newly discovered Type II Diabetes. Cardiovascular risk factors: smoking, arterial hyper tension, obesity, type 2 diabetes. Pathological personal history: N-STEMI and angioplasty with BMS stent (stent metal bars) on the ADA II in 04.2013. Suddenly installed retrosternal pain, accompanied by diaphoresis for about 2 hours and 30 minutes. Note that the patient has discontinued for the last 6 months, out of his own initiative, the treatment with aspirin and clopidogrel.
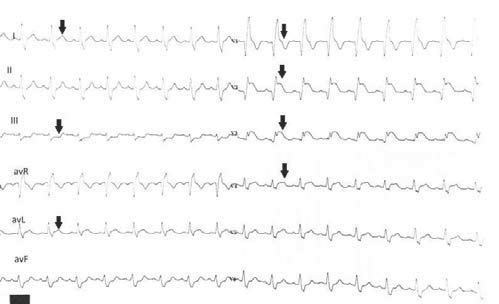
Figure 9. ECG on admission: SR with HR=90/min, RBBB, ST segment elevation V1-V6, DI, avL, ST depression in DIII.
One of the factors considered responsible for the late intra-stent thrombosis is the premature premature discontinuation of the dual antiplatelet therapy 3. Clinical examination: hemodynamically stable, BP = 130/90 mmHg, HR (heart rate) = 90b/min, left ventricular ga llop, systolic murmur in the mitral focus, pulsatile peripheral arteries, bilateral basal subcrepitant rales. Laboratory tests: positive troponin (0.41 ng/ml), glu cose = 520 mg/dl. Echocardiography on admission: nondilated left ventricle, EF=35%, akinesia in the anterior territory and in the LV apex; grade I mitral regurgitation, free pericardium. Coronary angiography revealed an intrastent thrombotic occlusion of the anterior descending artery, implanted for NSTEMI in 04.2013 (Figure 10). Thromboaspiration and balloon angioplasty was performed at the level of the stent on the anterior descending artery (Figures 12 and 13), the patient having tricoronary lessions with occlusion of the right coronary artery in segment II – hypoplastic vessel (Figure 11) and significant serial stenoses in the circumflex artery. Another factor responsible for late intra-stent thrombosis is the underexpansion of the stent – for which reason a balloon angioplasty was performed to our patient 3. Evolution was favorable during hospitalization without repeated angina, without heart failure symptoms. He will return later for interventional revascularization of the circumflex artery lesions.
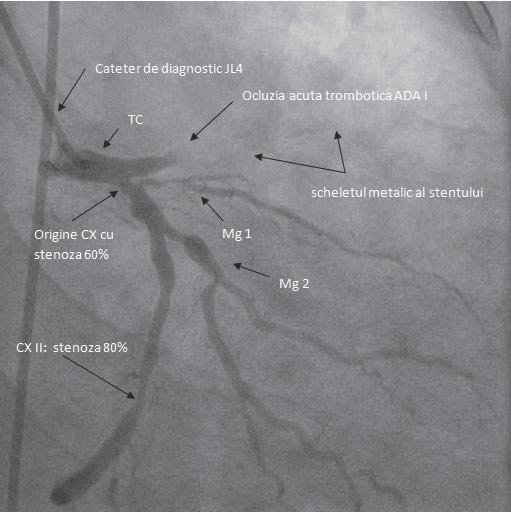
Figure 10. RAO caudal incidence- we identify a permeable left main. The proxial ADA has a stent (we identify the metallic part of the stent), but just before the stent, right after the ADA origin the vessel has an acute thrombotic occlusion (probably by intrastent thrombosis). CXA – dominant vessel is diffusely infiltrated with a 60% stenosis at the origin , and a 80% stenosis inthe medium segment. The first marginal – small vessel with a significant stenosis in the proximal segment. The second marginal – important vessel with atheromatous plaques but without any significant stenosis.
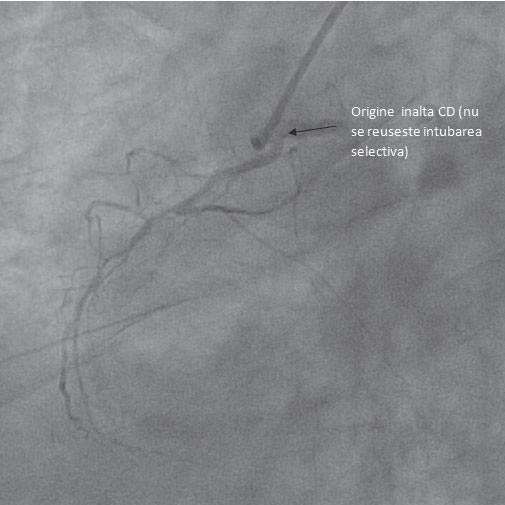
Figure 11. LAO 36° incidence. RAA hypoplastic vessel with an abnormal origin (high) difficult to intubate, has diffuse atheromatous infiltration in the medium and distal segments.
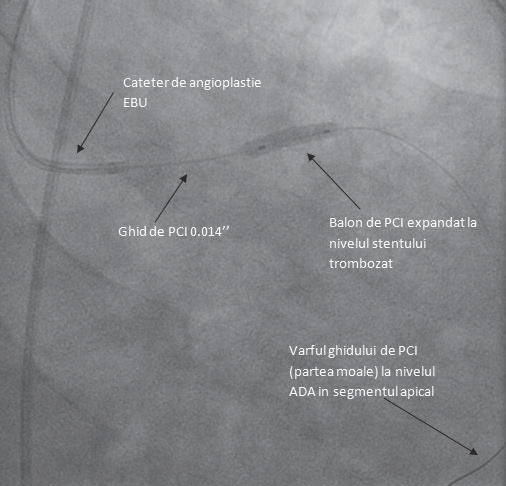
Figure 12. Balloon angioplasty at the level of the stent in order to break down the thrombus, open the vessel and also to better expand the stent.
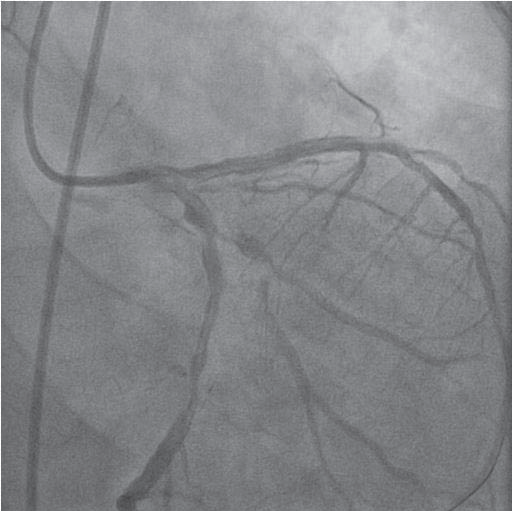
Figure 13. The result after the balloon angioplasty: TIMI 3 distal flux, without a residual lesion at the occlusion level. We confirm the diagnosis of intrastent thrombosis.
CASE 12
RF, man, 66 years old, presentation at 02:10 am. Diagnosis: Acute coronary syndrome without ST elevation, Triple aorto-coronary bypass (2002) with occluded venous grafts on the right coronary artery and Marginal I and permeable arterial graft on the anterior descending artery, Old myocardial infarction (1994), LV apical aneurysm, Grade III mitral regurgitation, Grade III essential arterial hypertension very high added risk, Type II diabetes, Dyslipidemia, Chronic kidney disease stage III. Cardiovascular risk factors: arterial hypertension, type 2 diabetes, dyslipidemia, chronic kidney disease Pathological personal history: old anterior-septal myocardial infarction (1994), triple aorto-coronary bypass (2002) without angina until 3 years ago, assessed by coronary arteriography in another clinic 3 days prior to hospitalization for unstable angina, when occlusion of venous bypass (Figure 14) and tricoronary lesions were detected (occlusion of ADA I, 60-70% stenosis of Mg I and 60-70% stenosis of distal circumflex artery, occlusion of RCA II) (Figure 15).
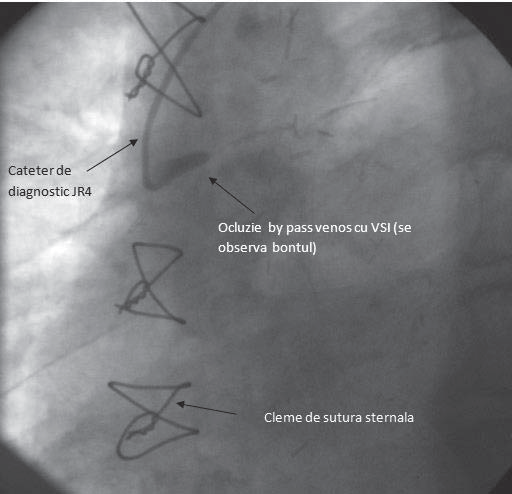
Figure 14. Venous by-pass on the CAX occluded (the image shows the blunt).
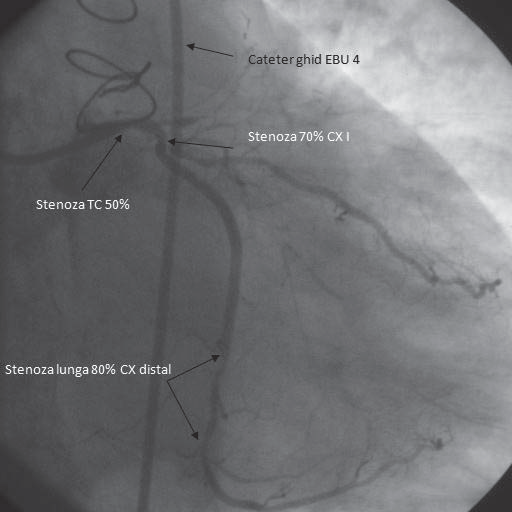
Figure 15. RAO (13°) caudal (30°) incidence. Injection in left coronary artery. Left main short with a 50% stenosis in the medio-distal segment. 70% stenosis in the proximal CXA in a curving area. Atheromatous infiltration with a long stenosis of 80% in the distal CXA. Late filling of a marginal branch of the CXA from the occluded CXA (towards which the venous bypass
was going ). ADA occlusion in segment I.
He was admitted for repeated episodes of angina at rest. Clinical examination on admission: mediocre general condition, conscious, cooperative, BP=150/90 mmhg, HR (heart rate)=80/min, systolic murmur grade 3/6 in the mitral focus, without systemic or pulmonary congestion. Echocardiography on admission: normal sized left ventricle, EF=40%; dyskinesia of the LV apex, hypokinesia of the inferior and lateral wall. Left atrium dilatation. Grade III mitral regurgitation, grade II tricuspid regurgitation; PAPs=28 mmHg. Normal pericardium.
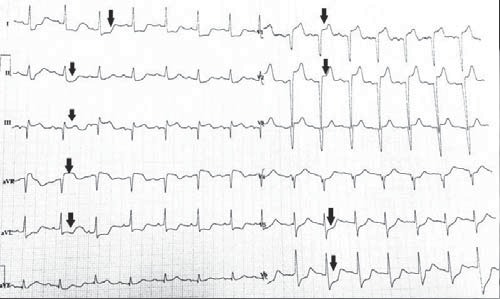
Figure 16. ECG on admission: Sinus rhythm with HR (heart rate)=100/min, QS V1-V3, aspect of „frozen” ST elevation in V1-V2, ST elevation in avR, Q wave in DIII, ST depression V5-V6, DI,DII, aVL.
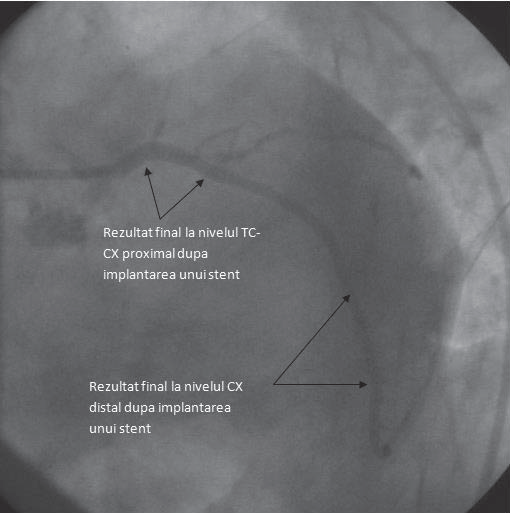
Figure 17. LAO incidence (36°) caudal (37°). Final result after the angiplasty with implantation of 2 stents: for the distal lesion and the one at the left main
towards CXA with a very good final result.
Laboratory tests: positive troponin (1 ng/ml), NT proBNP = 4564 pg/ml. 48 hours after admission, given the persistent episodes of angina refractory to maximal drug therapy, it is decided to perform angioplasty, implanting two stents in the lesions on the circumflex artery (Figure 17). Invasive strategy is indicated in the first 72 h from presentation in patients with at least one high risk factor or recurrent symptoms (class of indication I recommendation level A) 4. Interventional invasive revascularization of the vessel in question is usually the first option in most patients with multivessel ischemic heart disease according to the ESC/EACTS Guidelines on myocardial revascularization from 2014 5. Evolution was favorable during hospitalization, the patient did not repeat the angina episodes after angioplasty.
CASE 13
W I, woman, 87 years old, presentation at 03:00 am. Diagnosis: Acute coronary syndrome without ST-segment elevation in the inferior-posterior-lateral territory at 2,5 hours Killip class III, Grade IV mitral insufficiency, Grade IV tricuspid insufficiency, Severe pulmonary hypertension, Grade III essential arterial hypertension with high added risk. Cardiovascular risk factors: hypertension, age. Retrosternal pain onset 2 hours and 30 minutes before presentation. She claims intermittent episodes of angina the day prior to presentation.
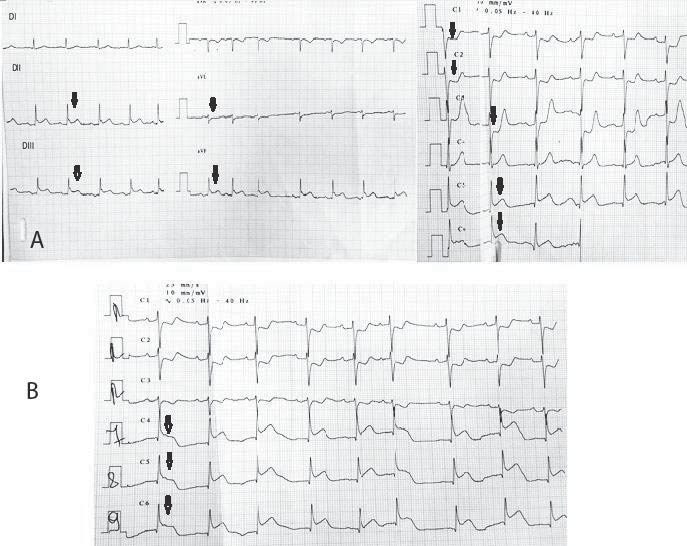
Figure 18. ECG on admission: sinus rhythm with HR (heart rate)=75/min, ST-segment elevation in DII, DIII, avF, V5-V6, mirror ST depression in avL, V1-V3 (A), ST elevation V7-V9 (B).
Clinical examination on admission: mediocre general condition, conscious, cooperative, BP-150/76 mmHg, HR (heart rate)=75/min, grade III/VI systolic murmur in the mitral focus irradiating in the armpit, subcrepitant pulmonary rales in the basal 2/3, 82% oxygen saturation corrected with O2 on the mask with 10 l/min to 86%, turgescent jugular veins. Echocardiography on admission: EF=40%, akinesia of inferior wall and 2/3 apical lateral wall, severe mitral regurgitation, severe tricuspid regurgitation, severe pulmonary hypertension, bilateral pleural fluid. Coronary angiography reveals subocclusion of the circumflex artery and 80-90% stenosis of anterior descending artery in the first segment (Figures 19 and 20). Primary balloon angioplasty is performed in the circumflex artery (small caliber vessel) (Figure 21) and it is decided to perform stent angioplasty of the lesion on the anterior descending artery (Figure 22) due to the patient’s hemodynamic instability, with a good final result. Immediate revascularization of the significant lesions that are not incriminate in causing STEMI during the same procedure with primary angioplasty of the incriminated vessel may be considered in some patients (class of indication IIb recommendation level B) according to the ESC/EACTS Guidelines on myocardial revascularization – 2014 5.
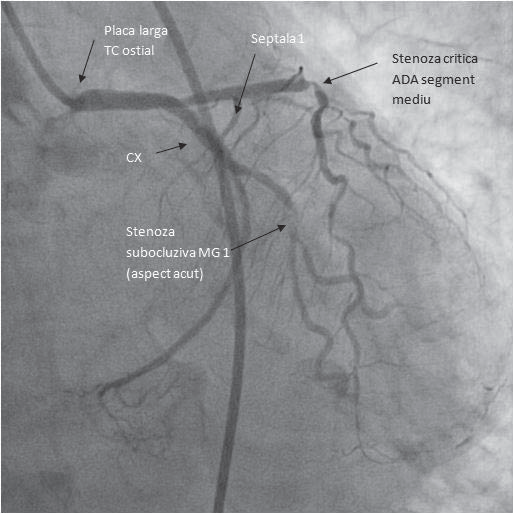
Figure 19. Caudal incidence (34°). Left main with a plaque at the origin. CXA with a subocclusive stenosis at the marginal I. Critical stenosis at the medium segment of ADA.
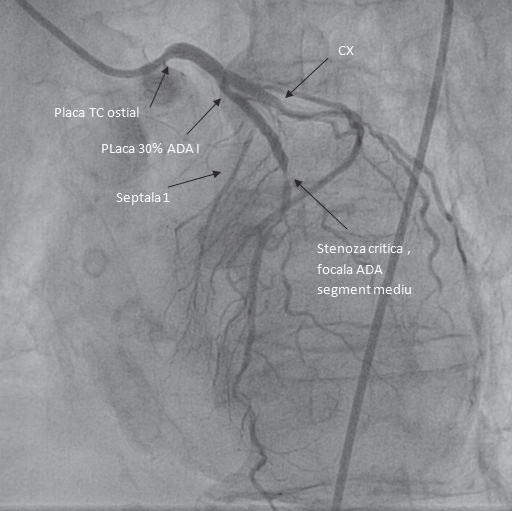
Figure 20. LAO (25°) cranial (35°). Left main with a plaque at the origin. ADA with a 30% plaque after its origin and a 90% stenosis in the middle segment.
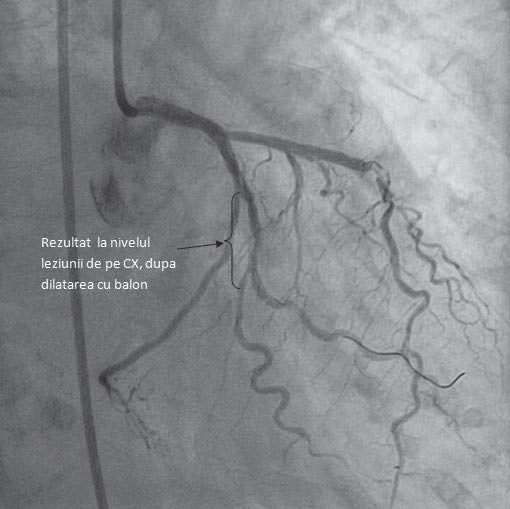
Figure 21. RAO (20°) caudal (34°) incidence. Th e result at the CXA level after the ballon dilatation. No stent was implanted. TIMI 3 flux without a significant dissection at the angioplasty place and with a 30-40% residual stenosis.
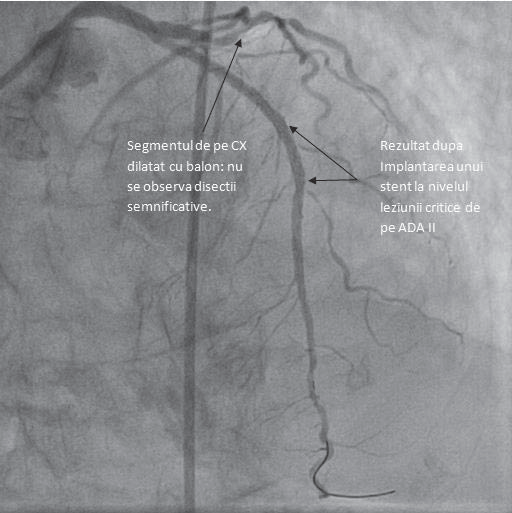
Figure 22. LAO (20°) cranial (30°) incidence. Very good final result after the stent implantation at the level of the lesion on ADA.
According to the PRAMI (Preventive Angioplasty in Acute Myocardial Infarction) study, adopting a strategy of preventive angioplasty with revascularization of significant lesions (>50%) at the time of revascularization of the lesion incriminated for STEMI resulted in significant decrease of primary outcome (consisting of cardiac death, non-fatal myocardial infarction and refractory angina) 6. Given the fact that the patient is in acute pulmonary edema, she is transferred to the ICU ward, and 24 hours later she is admitted to USTACC (monitoring and advanced treatment units for critical cardiac patients), because the pulmonary edema remitted, being hemodynamically stable. Evolution was favorable, without angina, with remission of the heart failure symptoms.
CASE 14
C F, man, 73 years old, presentation at 3:45 am. Diagnosis: Acute coronary syndrome with ST segment elevation in the inferior territory at 4 hours Killip class III, Tricoronary lesions, Aortic disease with severe aortic stenosis and grade II-III aortic insufficiency, Grade III mitral insufficiency, Grade III tricuspid insufficiency, Moderate pulmonary hypertension, Grade III essential arterial hypertension with high added risk, Dyslipidemia. Cardiovascular risk factors: Arterial hypertension, age, gender, dyslipidemia. Pathological personal history: with severe aortic stenosis and tricoronary lesions with valvular prosthesis indication and aorto-coronary bypass timed by the patient. Retrosternal pain onset 4 hours before presentation, accompanied by cold sweats. Clinical examination on admission: mediocre general condition, conscious, cooperative, BP = 140/70 mmHg, HR (heart rate) = 75/min, and under nitroglycerin BP falls to 60 mmHg, and HR (heart rate) = 41/min, with a subsequent increase of BP = 120/60 mmHg and HR (heart rate) = 75/min after discontinuation of nitroglycerin, grade III/VI systolic murmur in the aortic and mitral focus, 2/3 basal subcrepitant rales, discrete leg edema.
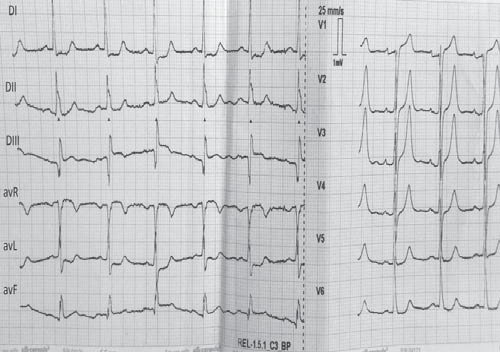
Figure 23. ECG on admission: sinus rhythm with HR (heart rate)=75/minute, ST-segment elevation in DIII, avF, avR, Q wave in DIII, avF.
Echocardiography on admission: nondilated left ventricle, concentric, EF=45%, akinesia of inferior wall, inferior septum and apex, grade III mitral regurgitation, severe aortic stenosis, grade II-III aortic regurgitation, grade III tricuspid regurgitation, PAPs = 42 mmHg, free pericardium. Laboratory tests on admission: positive troponin (22.3 ng/ml), NTproBNP-1548 pg/ml. Emergency coronary angiography reveals 70-80% stenosis of proximal left main (Figure 24), 80% stenosis of anterior descending artery in segment II, 70% stenosis of circumflex artery in segment I, interventricular posterior 70% stenosis (Figure 25).
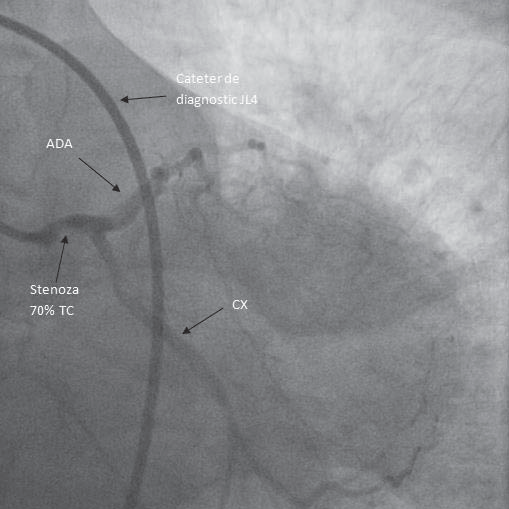
Figure 24. Caudal incidence (34°). Difficult to obtain an angiographic image: patient with a severe aortic stenosis and a significant left main stenosis(70%).
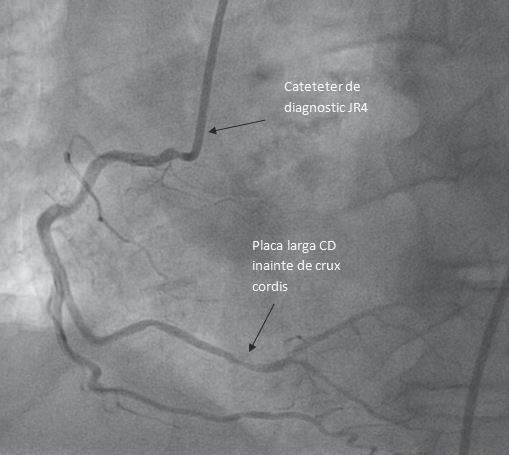
Figure 25. LAO (22°) cranial (25°) RCA with a plaque in the III segment before the crux cordis.
Because there was no lesion identified to be responsible for the acute coronary syndrome, no interventional revascularization was performed and is was decided to admit the patient in the ICU ward because he was in acute pulmonary edema for hemodynamic stabilization and after about 30 hours he is admitted to the USTACC for further treatment, seen as the clinical status improved. The evolution was favorable, without angina and with remission of the heart failure symptoms. The patient has indication for surgery – aortic prosthesis and aorto-coronary bypass which he delays again.
CASE 15
G V, woman, 69 years old, presentation at 5:20 am. Diagnosis: Acute coronary syndrome with inferior-posterior-lateral ST-segment elevation at 11 hours Killip class IV, Grade III essential arterial hypertension with very high added risk, Dyslipidemia, Grade II mitral regurgitation, Grade IV tricuspid regurgitation, Colon cancer operated and treated by chemotherapy with ileostomy. Cardiovascular risk factors: Arterial hypertension, dyslipidemia. Pathological personal history: operated colon cancer (2007), treated by radio- and chemotherapy. She was brought with the helicopter from Caracal hospital, where she presented herself initially for retrosternal pain with hemodynamic deterioration and syncope. The patient required intubation and mechanical ventilation during transportation, due to the deterioration of the neurological status. Clinical examination: severe clinical status, intubated and mechanically ventilated, SBP=80 mmHg under positive inotropic support with dobutamine and dopamine, HR (heart rate)=40/min without pulmonary rales.
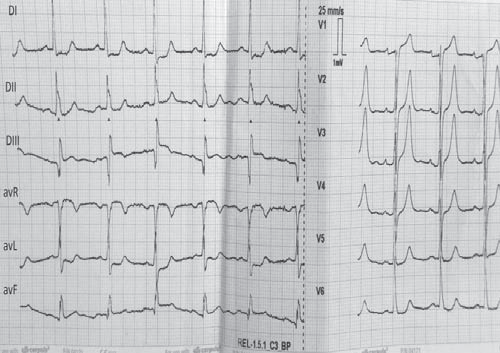
Figure 26. ECG on admission:third-degree atrioventricular block with junctional escape rhythm, HR (heart rate)=40/min, narrow QRS complex, STsegment elevation DII, DIII, avF, V7, V8, V9(a,b,c,d) ST depression in aVL (b).
Laboratory tests: positive troponin (1 ng/ml), NT-proBNP = 1450 pg/ml. Echocardiography on admission: nondilated left ventricle, EF=40%, 2/3 basal inferior wall akinesia, left atrium dilatation, grade II mitral regurgitation, right ventricular dilatation (48 mm), moderate RV global systolic dysfunction. Grade IV tricuspid regurgitation, PAPs=37 mmHg. Normal pericardium. The patient required temporary endocavitary pacing before starting the coronary angiography in order to perform it under safe conditions, suppressing the positive inotropic support after pacing. The coronary angiography reveals tricoronary lesions (right coronary artery with acute thrombotic occlusion in segment I (Figure 29); 50-60% stenosis of the left main segment I, 50% stenosis of the anterior descending artery II (Figure 27), 80-90% stenosis of the circumflex artery II (Figure 28), the implantation of 2 stents on the right coronary artery was decided (Figures 30 and 31) with a very good final result. The patient is transferred after performing the coronary angiography in the ICU ward, where she presents 4 episodes of ventricular fibrillation remitted after electrical shock delivered externally. Conduction abnormalities resolved subsequently, so that the temporary pacing could be interrupted. During her follow-up in the ICU ward the patient became agitated, showing focal neurological signs. Cerebral computer tomography was performed, leading to the diagnosis of ischemic stroke subsequently transformed into hemorrhagic stroke, requiring the discontinuation of heparin, the patient remaining only on low molecular weight heparin in a prophylactic dose.
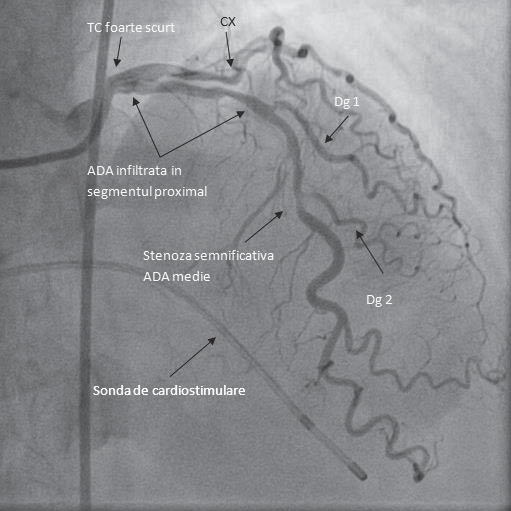
Figure 27. RAO (130°) cranial (40°) incidence. ADA infiltrated from its origin but with the most important stenosis in the middle segment before the diagonal 2 branch. It shows the pacing catheter at the apex of the right ventricle.
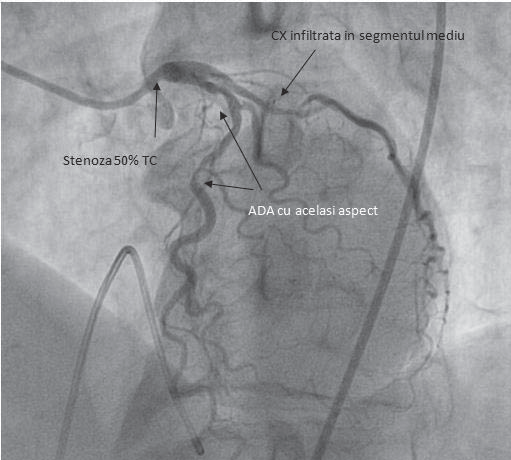
Figure 28. LAO (300°) cranial (270°) incidence. In this incidence we see the left main infi ltrated with a 40-50% stenosis and CXA with a long stenosis in the middle segment of about 70-80%. The same aspect in the ADA. We can’t see a retrograde filling of the RCA.
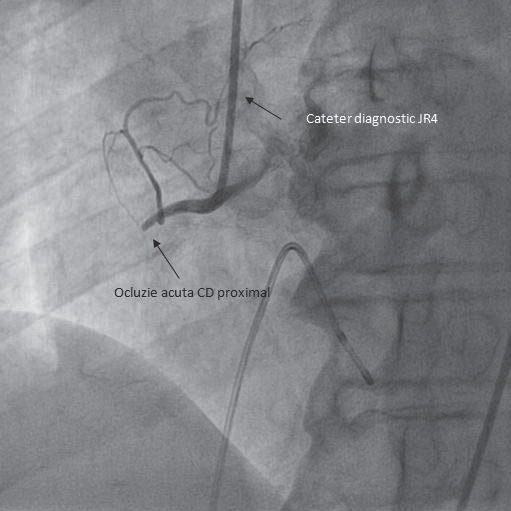
Figure 29. RAO (30°) incidence. Acute thrombotic occlusion of the proximal RCA.
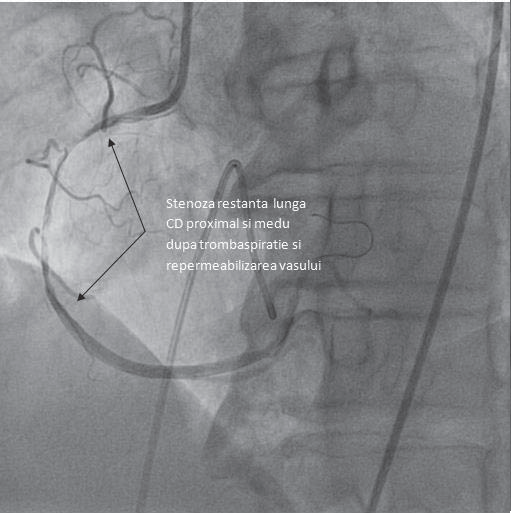
Figure 30. RAO (30°) incidence. After crossing with the guiding angioplasty catheter the vessel opens and we see a very long stenosis in the proximal and middle segment.
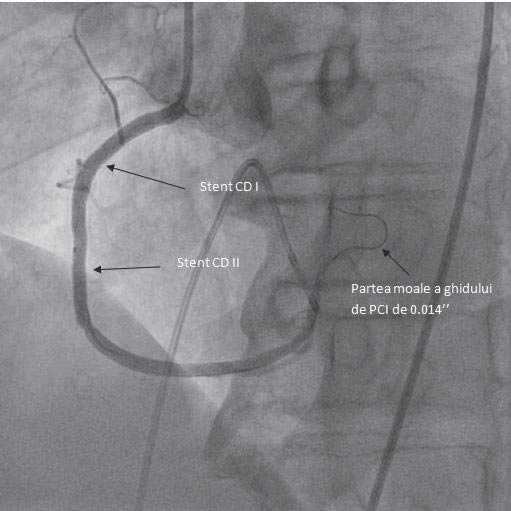
Figure 31. RAO (30°) incidence. Very good fi nal result after the implantation of 2 stents, which cover the whole lesion. No distal embolisation is present.
The patient also presented intense abdominal pain with reduced intestinal transit, the surgical consultation did not indicate surgery, subsequently the transit was spontaneously resumed. The patient has no solution of interventional myocardial revascularization of the remaining lesions, because they are calcified. She will be reassessed later to take a decision in respect of the surgical myocardial revascularization. The team on duty on the day when the ”Prof. Dr. C. C. Iliescu” Emergency Institute of Cardiovascular Diseases received the myocardial infarctions with ST-segment elevation (11th October 2014) was formed of Stoica Emanuel MD, Oprescu Alina MD, Anghelina Daniela, MD. The doctors on duty in the catheteriza-tion lab: Dan Deleanu MD, Cristina Popică MD, Călin Iulian MD. On duty for transesophageal echocardiography: Mihaela Rugină MD. On duty for cardiovascular surgery: Cristian Voica MD, on duty for ICU: Scarlat Costin MD.
Conflict of interest: none declared.
References
1. Montalescot, G. et al. ‘2013 ESC Guidelines On The Management Of Stable Coronary Artery Disease: The Task Force On The Management Of Stable Coronary Artery Disease Of The European Society Of Cardiology’. European Heart Journal 34.38 (2013): 2949-3003.
2. Erbel, R. et al. ‘2014 ESC Guidelines On The Diagnosis And Treatment Of Aortic Diseases: Document Covering Acute And Chronic
Aortic Diseases Of The Thoracic And Abdominal Aorta Of The Adult * The Task Force For The Diagnosis And Treatment Of Aortic Diseases Of The European Society Of Cardiology (ESC)’. European Heart
Journal 35.41 (2014): 2873-2926.
3. Holmes, David R. et al. ‘Stent Thrombosis’. Journal of the American College of Cardiology 56.17 (2010): 1357-1365.
4. Hamm, C. W. et al. ‘ESC Guidelines For The Management Of Acute Coronary Syndromes In Patients Presenting Without Persistent STSegment Elevation: The Task Force For The Management Of Acute
Coronary Syndromes (ACS) In Patients Presenting Without Persistent ST-Segment Elevation Of Th e European Society Of Cardiology (ESC)’. European Heart Journal 32.23 (2011): 2999-3054.
5. Windecker, S. et al. ‘2014 ESC/EACTS Guidelines On Myocardial Revascularization: The Task Force On Myocardial Revascularization Of The European Society Of Cardiology (ESC) And The European Association For Cardio-Thoracic Surgery (EACTS) * Developed With The Special Contribution Of The European Association Of Percutaneous Cardiovascular Interventions (EAPCI)’. European Heart Journal
35.37 (2014): 2541-2619.
6. Wald, David S. et al. ‘Randomized Trial Of Preventive Angioplasty In Myocardial Infarction’. New England Journal of Medicine 369.12 (2013): 1115-1123.
 This work is licensed under a
This work is licensed under a