Rodica Radu1,2, Ovidiu Mitu2, Igor Nedelciuc2, Cătălina Arsenescu-Georgescu1,2
1 “Grigore T. Popa” University of Medicine and Pharmacy, Iași, Romania
2 ”Prof. Dr. G. I.M. Georgescu” Institute of Cardiovascular Diseases, Iași, Romania
Contact address:
Rodica Radu. Tel: +40 745 637157
E-mail: rodiradu20@gmail.com
Received on 11 January 2014. Revised on 2 February 2014. Accepted on 4 February 2014.
We present the case of a 44 year old man, 5-month non-smoker, with treated hypertension and undertreated hyperlipidemia, who underwent a percutaneous transluminal coronary angioplasty (PTCA) on the 2nd marginal artery (M2) 3 years ago (the only coronary stenosis that time), and who was admitted in our service for daily, recurrent, spontaneous episodes of retrosternal chest pain appearing at rest, day and night, lasting for no more than one minute and resolving spontaneously. His treatment included Bisoprolol 5 mg/day, Aspirin 75 mg/day and Simvastatin 20 mg/day.
Clinical examination on admission revealed a blood pressure of 130/70 mmHg, heart rate 60 bpm, regular pulse, good clinical condition. The electrocardiogram (ECG) showed sinus rhythm, 59 bpm, intermediate axis, qR in DII, DIII and aVF. The transthoracic echocardiogram revealed a moderate concentric left ventricle (LV) hypertrophy, mild hypokinesis of the LV lateral wall, and preserved ejection fraction.
In order to gather evidence of ischemic ECG changes, we performed an ECG exercise stress testing that reached 89% of maximum heart rate, with a work-load of 200 W and 14.3 METS, that was negative for myocardial ischemia and/or angina. The ergonovine maleate provocation test (successive iv bolus doses, injected every 5 minutes: 0,05 mg, 0,1 mg, 0,15 mg and 0,2 mg respectively) revealed a mild ST segment elevation of maximum 1 mm in DII, DIII and aVF but was negative for chest pain throughout the whole test. The 24-hour ECG Holter monitoring was negative for ST segment changes.
Since all of the up-mentioned tests were inconclusive, we performed the coronary angiography (Figure 1, Figure 2), that revealed mild (30%) stenosis inside the stent on the M2, and two new culprit lesions: 85-90% stenosis on the first diagonal artery and occlusive stenosis, TIMI grade 0 flow, of the proximal left anterior descendent coronary artery (LAD), appearance that was first interpreted as chronic occlusion. Because the patient accused a new unset chest pain during the procedure, intracoronary nitroglycerine was injected, followed by the prompt remission of chest pain and concomitant appearance of the previously “missing” LAD, with a proximal critical (95%) stenosis (Figure 3). Successful PTCA with Everolimus eluting stent was accomplished on the LAD and with a bare metal stent on the first diagonal (Figure 4).

Figure 1. Contrast injection in the left coronary system: progressive occlusive stenosis on the LAD with TIMI 0 distal flux (white arrow) and 85-90% stenosis on the first diagonal artery (black arrow).

Figure 2. Contrast injection in the right coronary artery (RCA): ulcerated plaque 40% on the first segment of RCA, 95% stenosis of posterior left ventricular artery in distality and 75% stenosis of posterior interventricular artery in the proximal segment.

Figure 3. After intracoronary nitroglycerine administration: we can visualize the LAD course with 90% stenosis at the place of initial complete occlusion (arrow) and general coronary vasodilatation.
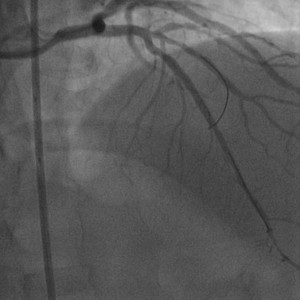
Figure 4. Final result after stent implantation on LAD and first diagonal, with TIMI III distal flux.
The following months, the patient’s frequent, spontaneous chest pain episodes were reduced almost completely with optimized medical therapy: Amlodipine besylate titrated up to 10 mg/day, Isosorbide mononitrate 40 mg/day, Bisoprolol 5 mg/day, dual antiplatelet therapy with Aspirin 75 mg/day and Clopidogrel 75 mg/day and high-dose Atorvastatin 80 mg/day.
Thus, the non-invasive tests were inconclusive in detecting ECG changes of myocardial ischemia. In our patient, with angiographically documented coronary spasm, the classical Ergonovine test failed to induce the coronary spasm. The final diagnosis for the mechanisms of chest pain needed the invasive approach. Moreover, increased attention should be paid at coronary angiography as severe spasm could be misinterpreted as an occlusive atherosclerotic lesion with a different final approach (medical treatment only) and practically worse prognosis for the patient.
Keywords: coronary spasm, coronarography, variant angina
Conflict of interests: The authors declare no conflict of interest.
 This work is licensed under a
This work is licensed under a