Stefan Mot1, Mihai Cocoi1, Alexandra-Florina Cocoi2, Razvan Mada2, Serban Adela1,2
1 CardioTeam Medical Center, Cluj-Napoca, Romania
2 „Iuliu Haţieganu” University of Medicine and Pharmacy, Cluj-Napoca, Romania
Abstract: The safety and feasibility of a same-day discharge (SDD) strategy after percutaneous coronary intervention (PCI) is still a matter of debate as there is a lack of universally accepted protocols and guidelines that address this topic. The aim of our study was to illustrate that SDD after successful elective percutaneous coronary intervention is a valid option for selected non-high risk patients with ischemic heart disease. 441 patients referred for elective PCI to CARDIOTEAM Medical Centre (Cluj-Napoca, Romania) during a time period of 2 years were prospectively observed. Stable subjects without severe comorbidities, radial access and no intra and/or periprocedural complications were considered for same-day discharge after successful PCI procedure done by a high-volume operator. The symptomatic status, need for readmission, renal function and major adverse cardiac events (myocardial infarction, need for repeated percutaneous revascularization or coronary artery bypass grafting (CABG) and death) were assessed one month later. 402 out of 441 patients (91%) were discharged during the same day. Minor puncture site complications occurred in a small number of patients (25), without impacting the discharge strategy. 7 patients needed redo-PCI; there were no deaths, myocardial infarction or need for CABG in the first 4 weeks of follow up. 6 patients developed contrast-induced nephropathy with complete recovery at follow-up. We conclude that same day discharge after successful elective PCI is a safe, feasible and cost-effective strategy for selected patients with ischemic heart disease, when performed by experienced operators. Keywords: same day discharge, PCI, non-high risk patients
INTRODUCTION
The advances in interventional technology and anti-thrombotic/antiplatelet therapy have promoted per-cutaneous coronary intervention (PCI) as a safe and effective treatment strategy in patients with ischemic heart disease1,11. Considering the high prevalence of coronary artery disease around the world, the costs generated by this invasive procedure have a major impact on health care systems2,3.
In elective patients undergoing successful and uneventful PCI, two follow-up strategies are currently being used worldwide: under 24h observation and/or same-day discharge (SDD)4,5,11. Despite the growing evidence in literature supporting the later strategy in carefully selected patients, overnight observation re-mains the standard approach in many centers3,6,11. The main concern is related to potential periprocedural events such as acute stent thrombosis, myocardial infarction or vascular access complications (which were significantly reduced by the use of radial access22). An important argument in favour of SDD in current available studies, is that major acute adverse events occur within the first 6 hours after the procedure7-9,11. Moreover, a SDD-strategy reduces the costs per patient as well as the risk of adverse events associated with prolonged hospitalization11-13.
A SDD-strategy after elective, uncomplicated PCI, has the potential of increasing availability of the procedure10. This is particularly important in areas with a low density of catheterization laboratories, as is Eastern Europe and thus Romania.
In this study we intended to illustrate that SDD after successful elective PCI is a feasible, safe and cost-effective procedure for both low and intermediate risk patients.
MATERIAL AND METHODS
This is a prospective, single-center observational study: we screened 441 consecutive adult patients, with stable CCS classes I-III angina, who underwent elective PCI at CARDIOTEAM Medical Center (Cluj-Napoca, Romania) between January 2015 and December 2016. Criteria used for a SDD-strategy consisted of: both male and female adult patients, with no up-per age limit with a previous diagnosis of stable angina (CCS I-III), on optimal medical therapy according to current practice guidelines, with no important blood-test abnormalities, who signed the informed consent and underwent elective, uneventful PCI for one or more severe (>70%) coronary artery stenosis/occlusion, asymptomatic after PCI, with good mental status, adequate social support and who live within 60 minutes from a primary PCI center. The high risk patient population, who needed overnight hospitalisation and surveillance, consisted of: subjects with acute coronary syndromes or symptomatic heart failure with low-ejection fraction (HFrEF), patients with severely abnormal blood-tests (Hg <10 g/dL, HTC <25%, PLT<100000/uL, positive TnI/T, CrCl <60 mg/dl, INR >2), with lesions unsuitable for PCI, or with intra-procedural complications (acute vessel closure, no-re-flow or slow-flow, coronary dissection or coronary perforation needing urgent treatment), use of atherectomy devices or unsuccessful PCI, persistent chest pain after the procedure, use of glycoprotein (GP) IIb/ IIIa antagonists, altered mental status, decompensated chronic obstructive pulmonary disease (COPD), Body Mass Index (BMI) >40, inappropriate social support or remote location (>60 minutes from a primary PCI center). Also, because at that time we did not use femoral closure devices, all cases with femoral access were excluded, irrespective of access site complications or not. The follow-up period for the study population was one month after the index-PCI. The study was approved by the local Ethical Committee.
Patient preparation: all patients were pretreated with aspirin and statins. A loading dose of 600 mg Clo-pidogrel or 180 mg Ticagrelor was given in the mor-ning of the procedure. Dual antiplatelet therapy was continued for 1 to 12 months after PCI, depending on the type of device used (BMS, DES or BVS), complexity of coronary lesions and comorbidities. Echocardiography, ECG and blood tests were performed in the morning of the intervention. BMI was calculated for each subject. Patients aged >75 years and/or with diabetes mellitus received 500 ml iv saline 0.9% before the procedure. Ambulation was done 2 hours after the procedure and patients were discharged after 6 hours of surveillance. ECG was repeated at the end of the intervention. All SDD patients received a telephone call within 24-48h after the procedure and a clinical follow-up (cardiology consult and standard blood tests) was performed 4 weeks after the procedure, or sooner in case of new onset of symptoms.
Procedural aspects: all procedures were performed by a single experienced operator via a 6F right or left radial/ulnar access with intravenous administration of weight adjusted unfractionated heparin (70-100 IU/ kg). Neither bivalirudin nor post-procedural heparin were used. Sheath removal was performed with manual compression and local haemostatic bands in the catheterisation laboratory after the procedure. The haemostatic devices were removed the morning after the procedure by the patient. Technical aspects such as: number, characteristics and lesion location, number of implanted stents, type of stent and procedural result were recorded. Intra- and post-procedural complications such as coronary dissections, perforation, access site bleeding and other local/general complications were documented. Troponins were not routinely assessed before discharge. The angiographic risk profile was assessed for each subject based on the coronary lesion distribution: patients with single vessel disease (aside from significant left main disease or ostial lesions) were considered to have a low risk profile; the presence of ostial lesions, multivessel disease, bifurcation lesion and chronic total occlusion were considered complex PCI lesions with higher procedural risk profile (Figure 1).
Descriptive statistics were used to analyse the study population.
RESULTS
Demographic cartacteristics of the patients are as follows: the mean (±standard deviation) age of the study population was 64±10 years. 289 were men, 121 were current smokers and 58 were former smokers. 208 subjects had a history of arterial hypertension, 302 had mixed dyslipidemia, 125 were diabetic and 217 had a BMI >25 kg/m2. 112 patients had a history of myocardial infarction, 89 a history of percutaneous coronary revascularization and 18 a history of surgical revascularization.
402 out of 441 patients (91%) were discharged during the same day. 7 patients were excluded due to unsuccessful PCI, 5 due to hospitalisation for close renal function monitoring, 4 due to coronary dissection, treated percutaneously. The femoral access had to be used in 14 patients due to unfeasible radial ulnar or brachial access. In 9 patients successfully treated we preferred overnight surveillance due to lack of social support or remote location.
A total of 639 vessels were treated (1.45 per patient) using 777 stents (1.76 per patient). Complex PCI was performed in 313 patients. Bifurcation lesions were treated in 113 cases. Of these, in 88 cases a provisional strategy was used, while 25 lesions were treated with two stents. Ostial lesions were stented in 67 subjects. PCI for chronic total occlusion was performed in 8 patients. Procedural details such as the type of revascularization and the type of stents used are summarized in Table 1 and Table 2. No GP IIb/IIIa antagonists were used.
Minimal chest pain after PCI was encountered in 17 cases. As nitrates immediately relieved the pain, the patients were discharged after 6 hours of surveillance. No peri-procedural infarction was encountered. No need for readmission within the first 24 hours after PCI occurred. Minor hematomas at the puncture site were found in 25 subjects, without affecting the early discharge strategy. No other bleeding complications occurred. 6 patients developed CIN and were refer-red to the nephrologist.
387 patients returned for the one month follow up, out of witch: 7 patients were readmitted earlier due to recurrent unstable angina (patients who were early-readmitted and underwent a redo-PCI procedure, had multivessel disease or single functional vessel; in those patients, after successful redo-PCI, we replaced Clopidogrel with Ticagrelor); no myocardial infarction occurred; no need for CABG or death occur-red within the first month after PCI. All followed-up patients had a CrCl >60 ml/min.
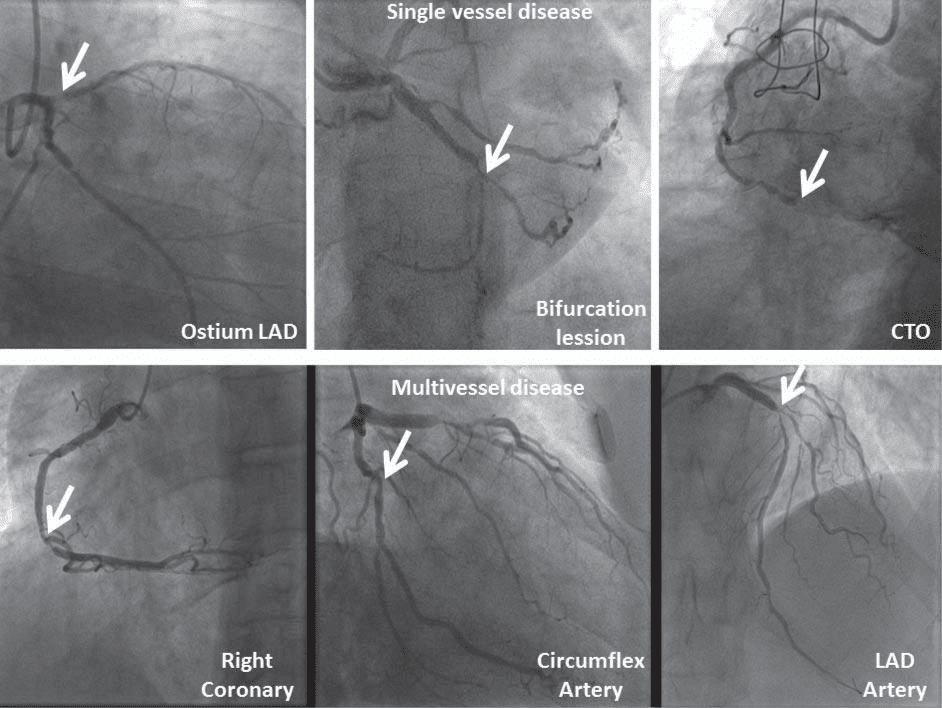
Figure 1. Complex PCI lesion examples. Upper panel: Single vessel disease (Ostium of the LAD); Bifurcation lesion; CTO (Chronic Total Occlusion). Lower panel: Multivessel disease.
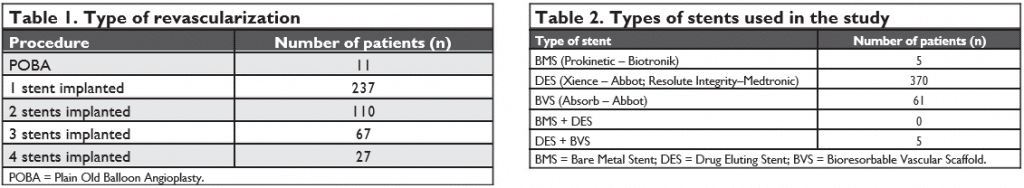
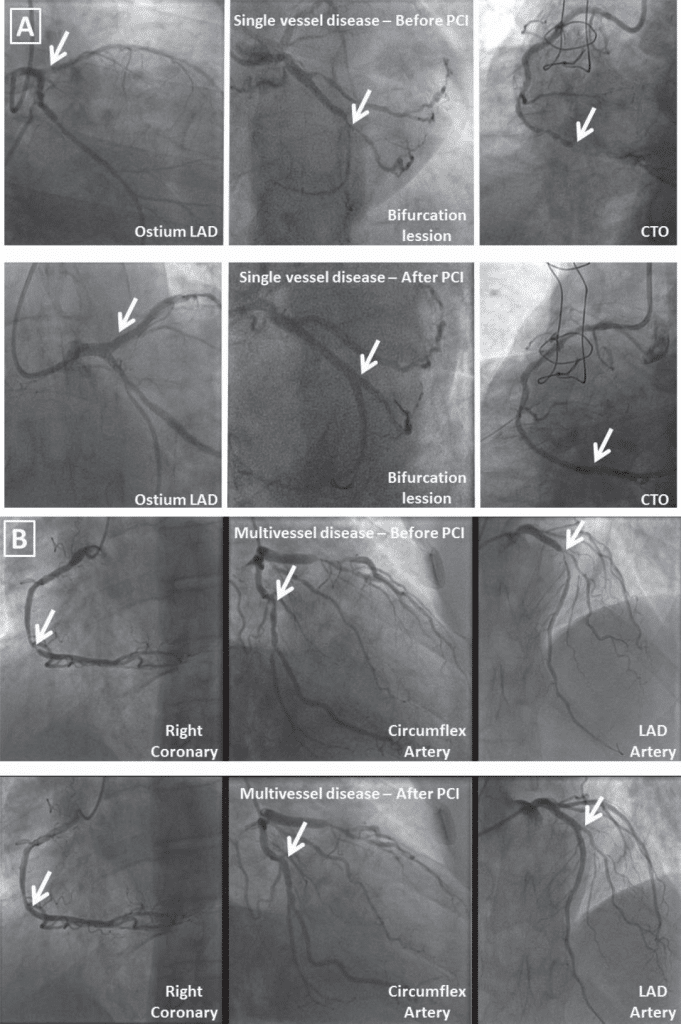
Figure 2. Complex PCI lesions before and after stenting: A. Single vessel disease (Ostium of the LAD), bifurcation lesion; CTO. B. Multivessel disease.
DISCUSSION
The aim of our study was to evaluate the safety and efficiency of SSD-PCI in a selected patient population (non-high risk patients), successfully treated percutaneously.
Current (2018) SCAI Expert Consensus Document11 highlights the importance of patient selection and discharge strategy based on individual patient and procedural factors. Our approach when considering a SSD-strategy follows the consensus recommendations; therefor, when selecting the patients we took into consideration patient, procedure and program factors (for example, subjects with severe chronic kidney disease or HFrEF were not included in the study as these comorbidities were shown to increase the rate of peri-procedural complications14-16). Complex PCI is a parameter which was associated with adverse events in previous studies4,5; however, in contrast to the patient factors, it is highly dependent on the proficiency of the operators and the efficiency of the catheterisation and follow-up team. In our study, complex PCI was not a definitive criteria for deferring a SDD-strategy, as all PCIs were performed by a high-volume opera-tor and experienced team. It is expected that in less experienced hands, the incidence of adverse events could be higher. There was a small number of patients who were readmitted due to recurrent symptoms, but none wi-thin the first 24 hours after discharge; however, no PCI is completely predictable thus, intra and peri-pro-cedural complications can occur17,18, emphasizing the need for available hospitalisation beds even when the procedure is performed electively and a SDD-strategy is chosen.
Subjects who developed CIN had multiple risk factors (age >75 years, diabetes mellitus and arterial hypertension) and complex coronary lesions which needed high contrast volumes (>200 ml). However, after proper treatment their CrCl returned to base-line values.
In Romania, subjects with stable coronary artery disease usually undergo PCI as in-hospital patients. However, the limited number of hospitals where catheterization laboratories and trained operators are available, in addition to emergency priorities, limit the access to interventional treatment for an important number of patients with ischemic heart disease, generating prolonged waiting lists. The SDD-strategy in-creases availability of the procedure as both national and private practice laboratories can implement the strategy, improving medical care. Moreover, several studies have shown that patients’ satisfaction is significantly improved when they were discharged on the same day10,14,15,19-21.
The financial implications of this approach cannot be neglected. Health Care Systems usually reimburse elective PCI as an outpatient procedure, defined as hospitalization <24 hours. Hospitals receive the same amount of money regardless of the length of stay during this time interval11,12. Moreover, it was previously showed in a model from 206489 patients (Victoria, Australia – 2005/2006) that the costs per patient are almost doubled (from 950 to 1850 euros) in the case of overnight stay13.
LIMITATIONS
This is an observational study, therefore a complete statistical comparison between different strategies is difficult. Moreover, the study population is limited, as all procedures were done in a private practice; this makes observing rare complications hard as the number of patients followed is small; the follow-up period was limited to one month therefore late complications (in-stent restenosis or scaffold thrombosis/restenosis) could not be evaluated.
The patients considered for SDD-discharge, were non-high risk subjects; we believe that subjects with high-risk profiles are not suitable for this strategy, therefore a good patient selection is probably the most important factor contributing to the safety of early discharge.
These are the results of one highly experienced, high-volume operator, therefor general conclusions and recommendations cannot be drawn regarding intra and peri-procedural complications in other centers with less experiencer operators. However with good patient selection, and proper follow-up, complication rates can be low enough to support a SDD-strategy in the majority of PCI-cases.
CONCLUSION
For our particular study population (non-high risk patients), same day discharge after successful elective percutaneous coronary intervention was a safe, feasible and cost-effective strategy.
Disclosure: The authors have no conflicts of interest to declare.
References
1. Windecker S, Kolh P, Alfonso F et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Re-vascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) * Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 35(37):2541–2619.
2. Kugelmass AD, Cohen DJ, Brown PP, Simon AW, Becker ER, Cull-er SD. Hospital resources consumed in treating complications associated with percutaneous coronary interventions. Am J Cardi-ol2006;97:322–327.
3. Roger VL, Go AS, Lloyd-Jones DM et al. Heart disease and stroke statistics–2012 update: a report from the American Heart Association. Circulation 2012;125:e2–220.
4. Brayton KM, Patel VG, Stave C, de Lemos JA, Kumbhani DJ. Same-day discharge after percutaneous coronary intervention: a meta-analysis. J Am CollCardiol2013;62:275–285.
5. Abdelaal E, Rao S V, Gilchrist IC et al. Same-day discharge compared with overnight hospitalization after uncomplicated percutaneous coronary intervention: a systematic review and meta-analysis. JACC CardiovascInterv2013;6:99–112.
6. Rao SV, Kaltenbach LA, Weintraub WS et al. Prevalence and out-comes of same-day discharge after elective percutaneous coronary intervention among older patients. JAMA 2011;306:1461–1467.
7. Thel MC, Califf RM, Tardiff BE et al. Timing of and risk factors for myocardial ischemic events after percutaneous coronary intervention (IMPACT-II). Integrilin to Minimize Platelet Aggregation and Coronary Thrombosis. Am J Cardiol2000;85:427–434.
8. Jabara R, Gadesam R, Pendyala L et al. Ambulatory discharge after transradial coronary intervention: Preliminary US single-center experience (Same-day TransRadial Intervention and Discharge Evalua-tion, the STRIDE Study). Am Heart J 2008;156:1141-1146.
9. Small A, Klinke P, Della Siega A et al. Day procedure intervention is safe and complication free in higher risk patients undergoing transradial angioplasty and stenting. The discharge study. Catheter Cardio-vascInterv2007;70:907-912.
10. Banning AP, Ormerod OJM, Channon K et al. Same day discharge following elective percutaneous coronary intervention in patients with stable angina. Heart 2003;89:665-666.
11. Seto AH, Shroff A, Abu-Fadel M, et al. Length of stay following per-cutaneous coronary intervention: An expert consensus document update from the society for cardiovascular angiography and interventions. Catheter Cardiovasc Interv. 2018;00:1-15.
12. Bertrand OF, Gilchrist IC. Interventional cardiology: Time for same-day discharge after uncomplicated PCI? Nat Rev Cardiol2012;9:8-10.
13. Hauck K, Zhao X. How dangerous is a day in hospital? A model of adverse events and length of stay for medical inpatients. Med Care 2011;49:1068-1075.
14. Carere RG, Webb JG, Buller CE et al. Suture closure of femoral arterial puncture sites after coronary angioplasty followed by same-day discharge. Am Heart J 2000;139:52-58.
15. Glaser R, Gertz Z, Matthai WH et al. Patient satisfaction is comparable to early discharge versus overnight observation after elective per-cutaneous coronary intervention. J Invasive Cardiol2009;21:464-467.
16. Chung W-J, Fang H-Y, Tsai T-H et al. Transradial approach percutaneous coronary interventions in an out-patient clinic. Int Heart J 2010;51:371-376.
17. Anderson HV, Shaw RE, Brindis RG et al. A contemporary overview of percutaneous coronary interventions. The American College of Cardiology-National Cardiovascular Data Registry (ACC-NCDR). J Am CollCardiol2002;39:1096-1103.
18. Kutcher MA, Klein LW, Ou F-S et al. Percutaneous coronary interventions in facilities without cardiac surgery on site: a report from the National Cardiovascular Data Registry (NCDR). J Am CollCar-diol2009;54:16-24.
19. Knopf WD, Cohen-Bernstein C, Ryan J, Heselov K, Yarbrough N, Steahr G. Outpatient PTCA with same day discharge is safe and produces high patient satisfaction level. J Invasive Cardiol 1999;11: 290-295.
20. Le Corvoisier P, Gellen B, Lesault P-F et al. Ambulatory transradial percutaneous coronary intervention: a safe, effective, and cost-saving strategy. Catheter CardiovascInterv2013;81:15-23.
21. Khatri S, Webb JG, Carere RG et al. Safety and cost benefit of same-day discharge after percutaneous coronary intervention. Am J Cardiol2002;90:425-427.
22. Jaen EGI, Ruigomez FJG. Same-day Discharge After Elective Percutaneous Coronary Intervention: A Safe Strategy, but for Which Patients? Rev Esp Cardiol. 2017;70(7):524-526.
23. Graziano FD, Banga S, Busman DK et al. Barriers to Early Discharge after Elective Percutaneous Coronary Intervention (BED PCI): A Single-Center Study. Indian Heart Journal; 2017;69:217-222.
 This work is licensed under a
This work is licensed under a