Irina-Elena Dumitrescu1, Madalina Duna1, Lavinia Stanescu1, Denisa Predeteanu1
1 Clinic of Internal Medicine and Rheumatology, “Sf. Maria” Clinical Hospital, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania
Abstract: Rheumatoid arthritis (RA) is a rheumatic inflammatory disease mainly characterized by chronic synovitis of peripheral joints leading to osteoarticulardistructions which consequently involves the decrease in the joint function.RA is frequently associated with a high cardio-vascular (CV) risk involved in an increased CV morbidity and mortality of such pa-tients compared with general population.The traditional risk factors for atherosclerosis are more prevalent in RA patients, but they do not completely explain the excess of CV risk. Early and accelerated atherosclerosis in patients with active RA may cause frequent CV events, the common element of these two diseases being chronic inflammation.We present a case of active RA complicated with acute myocardial infarction developed when the patient discontinued the immunosuppressive therapy with conventional synthetic Disease-Modifying AntiRheumatic Drugs (cs DMARDs) treated with inserting a coro-nary stent; a stent thrombosis appeared because the patient was noncompliant and discontinuated the indicated treatment. Keywords: rheumatoid arthritis, cardiovascular risk, chronic inflammation, Treat-to-Target.
INTRODUCTION
Rheumatoid arthritis (RA) is a chronic rheumatic in-flammatory disease, predominantly affecting periphe-ral joints with their possible anatomical distruction and reduction of function. It is now well established that RA is associated with increases in morbidity and mortality compared with general population. RA in-creases CV morbidity and mortality by up 50% com-pared with general population and CV disease (CVD) is the leading cause of death in RA1,2.
There is a high risk of acute myocardial infarction (AMI) in patients with RA and this risk is similar with the risk of AMI in diabetes mellitus and it generally coresponds with the risk of AMI in non-RA subjects 10 years older3.There is a nationwide retrospective cohort study which indicates that AMI risk increased by 38% in RA patients compared to the general population and the presence of comorbidities increased the AMI risk independently4.
Early and accelerated atherosclerosis is considered to be responsible for the more frequent CV events in RA patients. Traditional risk factors for atherosclero-sis do not entirely explain the high risk of CV events in patients with RA. Chronic infl ammation is a common feature of both RA and atherosclerosis due to many similarities between RA and atherosclerosis. The pathologic processes in both RA and atherosclerosis are similar, if not common, being immune mediated by Th1 and Th175. Common infl ammatory mediators such as tumor necrosis factor (TNF), Receptor acti-vator of NF-kB ligand (RANKL)/Receptor activator of NF-kB (RANK)/osteoprotegerin (OPG) system, CD40/CD40 ligand orchestrate pathophysiological processes in RA and atherosclerosis6.
Growing evidence suggests that this excessive in-flammatory burden is accountable for the “lipid para-dox” in RA, in which cholesterol-an important CV risk factor in the general population-is inversely related to CV risk in patients with untreated RA. In contrast, suppression of RA-associated inflammation coincides with some increases in lipid values, but also a reducti-on in CV events7.
As the CV risk in RA patients is high especially in active disease a strict monitoring of patient in viewof a correct treatment to reduce disease activity is manda-tory in clinical practice.
There is also known that treatment with statins de-creases the risk of AMI not only in general population, but also in RA patients. A population-based cohort study showed that RA patients who discontinue sta-tins have increased risk of AMI8.
There is a different pattern of the CVD in RA com-pared with general population characterized by a greater risk for patients to develop heart failure or sudden death. No differences were found regarding the number of acute coronary lesions or the degree of stenosis in patients with RA and AMI, but different histological characteristics of atherosclerotic plaques were described; the plaques tend to have a greater de-gree of inflammation and instability making them more prone to rupture and consecutive thrombosis9.
It also known that many scores are used to evaluate CV risk in general population, but a complete score whichtakes into account both traditional risk factors for atherosclerosis and specific factors for RA is still expected being necessary in clinical practice.
CASE REPORT
Wepresent the case of a 64 year old female, ex-smo-ker, having no family history of cardiovascular or rheu-matic diseases who is currently admitted to “Sf. Maria” Clinical Hospital for clinical and biological reassess-ment of her underlying disease – seropositive RA.
The symptoms of the patient started in June 1999 when she accused painful swelling of both knees and ankles. The symptoms at that time were interpreted as the onset ofspondiloarthritis as the patient was tes-ted positive for the presence of HLA-B27 antigen. She was given immunosuppressive treatment with sulfa-salazine (3 g/day) and nonsteroidal anti-infl ammatory drugs (NSAIDs).
In January 2000 she was admitted for the first time to “Sf. Maria” Clinical Hospital with the same art-hralgias but also with swelling and inflammatory pain in her metacarpophalangeal (MCP) and proximal in-terphalangeal (PIP) joints of both hands. She also had high levels of the inflammatory tests (ESR, C reactive protein, fibrinogen) and high titer of rheumatoid fac-tor (RF). Given these findings she was then diagnosed with seropositive RA and the treatment was initiated with methotrexate (5 mg/week) plus sulfasalazine (1 g/ day) and prednisone (20 mg/day).
Between 2000 and 2007, the patient’s disease took various aspects requiring small changes in the corti-costeroid dosage or the sulfasalazine dosage based on the fact that sulfasalazine is the choice immunosuppre-ssive for peripheral articular infl ammatory symptoms and the patient’s major pain was in her right knee.
In July 2012, after more than 10 years of evolution of rheumatic disease, the patient was diagnosed with coronary artery disease after she experienced an epi-sode of cardiac-type chest pain which brought her to the emergency room of a country hospital. A possible myocardial infarction was eliminated from the diffe-rential diagnosisat that time because the ECG showed no signs of coronary acute obstruction and myocardial enzymes were negative.
In July 2013 (one year later), the patient stopped taking any kind of immunosuppressive medication out of personal reasons; she only took NSAIDs such as Diclofenac (150 mg/day) during periods of severe joint pain.
All this led to the main CV event that happened in August 2014, an infero-lateral AMI which was ra-pidly treated by primary percutaneous transluminal coronary angioplasty (PTCA) and a drug-eluting stent (DES) was embedded at the thrombosis site on the right coronary artery.
Unfortunately, the patient is uncompliant to the double antiplatelet therapy (both clopidogrel and aspirine), therefore two weeks after the CV event she suffers a new one, thrombosis in the newly implanted DES stent, also being quickly treated by balloon an-gioplasty with the restoration of a satisfactory coro-naryblood flow TIMI 3. After 3 weeks the patient’s rheumatic disease was reassessed at “Sf. Maria” Cli-nical Hospital and, asexpected at this moment, the Disease Activity Score 28 (DAS28) indicated a highly active disease (DAS28=5.3). Immunosuppressive the-rapy was restarted with methotrexate (20 mg/week).
The subsequent check-ups revealed a similar clinical picture: inflammatory arthralgias mostly of the radio-cubitocarpal (RCC) and metacarpophalangeal (MCP) left joints with synovitis demonstrated by muscu-loskeletal ultrasound, but the markers of infl ammation (ESR, C reactive protein and fi brinogen) were within normal range.
Remission of the disease for early RA and low di-sease activity for established RA represents the goal of treatment in accordance with Treat-to-Target stra-tegy. For our patient who has an established form of the disease, targeting the low disease activity represents the target of the therapy. The absence of biological inflammatory syndrome made it impossible to prescri-be biological treatment in accordance with National Protocol for Biological Therapies in RA, therefore a triple immunosuppressive therapy was given (metho-trexate plus sulfasalazine plushydroxichloroquine) as the last resort; she became intolerant to sulfasalazi-ne and hydroxichloroquine proved to be inefficient in her case, so she is currently on methotrexate (20 mg/ week) and prednisone (10 mg prednisone) alongside her conventional CV treatment which consists of dou-ble antiplatelet therapy, a beta blocker and a statin; her evolution has been uneventful ever since.
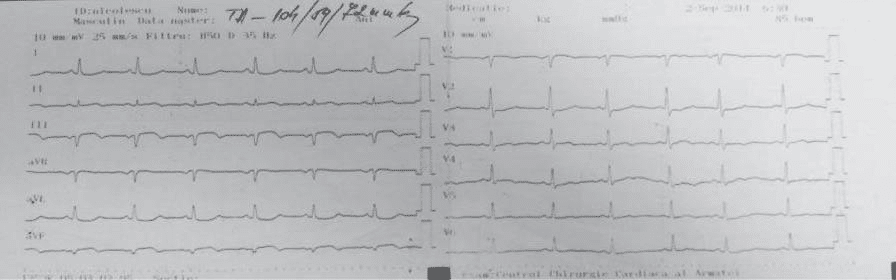
Figure 1. ECG tracing from 2014 (one and a half week after the myocardial infarction) – Q waves in DIII, aVF, ST elevation in DII, DIII, aVF and negative T waves in DII, DIII, aVF.

Figure 2. Radiocubitocarpian (RCC) joint swelling and atrophy of the in-terosseusmuscles.

Figure 3. Swelling of the bilateral knees (right>left) with valgus deformity.

Figure 4. Permanent proximal interphalangian (PIP) fl exion in 2nd and 3rd fingers of bothfeet; right hallux valgus.
DISCUSSION
We felt the need to present this clinical case of a fe-male patient diagnosed with RA who developed an AMI ten years after the positive diagnosisat a time when she discontinued immunosuppressive treatment taking only diclofenac (150 mg/day) well known for its CV adverse effects. We consider it a very complex because the solution of the AMI in this female patient with longstanding, active form of RA was PCTA com-plicated with thrombosis of the stent, also because of her own decision to interrupt the indicated treatment.
Our case confirms once againthe data in literature regarding the increased CV risk in patients with RA as well as high incidence of AMI, especially in patients with active RA. The significance of this problem drew European League Against Rheumatism s (EULAR s) at-tention which published in 2009 and 2016 two sets of recommendations CV risk management in patients with RA and other forms of infl ammatory disease. Unlike to 2009 recommendations10 which multiply by 1.5 the CV risk in patients with RA having special fea-tures such as extraarticular manifestations, high levels of Rheumatoid Factor (RA) and anti-CyclicCitrullina-ted Peptide (CCP) antibodies and a longer than 10 years evolution, the 2016 recommendations11 recon-sider this situation, mentioning that these RA specific features should no longer be considered necessary for the application of that multiplication factor as there is a CV risk even in patients in the early stages of the disease without extraarticular manifestations.
Within this context our case report underlines once again the CV risk in RA patients and more than that stresses that factors involved in this CV risk such as activity of the disease, improper medication and uncompliances to treatment are very important in this setting as our title suggests: RA-an enemy of the heart.
In the case of our patient the fact that the target of low disease activity had not been reached she experi-enced an AMI after giving up treatment during the high activity of the disease.
Besides the high activity of the disease other con-tributing factors leading to AMI include the treatment with diclofenac known for its CV risk and the fact that she was noncompliant to her doctor’s advice and she stopped immunosuppressive treatment before rea-ching the target.
The presented clinical case reveals a RA patient who suffered an AMI fifteen years after she was di-agnosed with RA. The CV event happened during an active phase of the disease (DAS28=5.3) and when no immunosuppressive therapy was present.
The treatment of RA in accordance with the prin-ciple of “Treat to Target” is very important in decre-asing the CV risk in patients with active form of the disease. In the context of the treatment, Methotrexa-te (MTX), considered a mainstay of therapy for RA, can ameliorate some of this excess CV risk, an effect that has not been seen consistently with other disea-se-modifying antirheumatic drugs (DMARDs). The cardioprotective action of MTX may occur through reducing systemic inflammation and by directly affec-ting some of the cellular mechanisms that lead to athe-rosclerosis. There are several effects of MTX in CV di-sease: MTX reduce all-cause CV disease, heart failure (strong strength of effect), AMI and stroke (moderate strength of effect). It is very important to add that MTX increase hyperhomocysteinaemia, but this effect is ameliorated by folic acid supplementation (strong strength off effect)12,13.
A study designed to explore the effect of disease modifying anti-rheumatic drugs (DMARDs) on synovi-al infl ammation as well as on atherosclerotic indices in patients with early rheumatoid arthritis shows that af-ter 1 year of treatment there is a signifi cant improve-ment of variables like erythrocyte sedimentation rate (ESR) and high sensitivity C-reactive protein (hsCRP), DAS28, HAQ-DI and a significant decrease carotid in-tima-media thickness (cIMT) from the baseline14.
In the treatment of the RA, NSAIDs represent another very important medication used to decrease the signs and symptoms of the inflammation, but un-fortunately they are associated with a high risk of CV diseases: arterial hypertension, ischaemic heart disea-se, heart failure. In order to best choice of a NSAID in patients with RA is very important to take into consideration not only the type of the drug (COX-1, COX-2), but also the profile of the patient with this rheumatic disease. If NSAIDs use is unavoidable, blood pressure must be checked regularly and in this situation naproxen is probably the fi rst choice. Furt-hermore, the combination of NSAIDs and aspirin is not advisable, since NSAIDs may impair the antiplate-let function of aspirin15.
At the same time, the glucocorticosteroids are very powerful anti-inflammatory drugs and are com-monly used as treatment for patients with RA. They have strong anti-inflammatory properties which co-uld mean that GCs have anti-atherosclerotic effects. However, in the general population, therapeutic do-ses of oral GCs (≥7.5 mg/day) have been associated with increased CV disease and all-cause mortality. The effect of GCs on the CV risk probably depends on several factors, such as the population of RA patients, the circumstances and way it is used, the dosage and treatment duration16.
For all reasons stated before, it is important to have tools that help in assessing the CV risk in pa-tients with RA. Though it may seem that in medical literature exist more than one score that can predict one’s CV risk (for instance: SCORE, Framingham BMI, Framingham lipids, etc), it is also true that these sco-res take into consideration only traditional risk factors like hypertension, diabetes, smoking, cholesterol level, etc. In 2008 in BMJ was published an article about the development of a new CV risk score named QRISK2 which has proven to be most complete one until now and the one which considers RA among the CV risk factors. The results of the calibration and discriminati-on statistics for QRISK2 were significantly better than those for the modified Framingham score in the vali-dation sample. At the 10 year risk threshold of 20%, the population identified by QRISK2 was at higher risk of a CV event than the population identifi ed by the modifi ed algorithm17.
There are several studies showing the pleiotropic effect of statins as adjunctive therapy to specific treat-ment in patients with RA. A double-blinded, randomi-zed placebo-controlled trial that included 116 patients with RA randomised to receive 40 mg atorvastatin or placebo in association with DMARDs showed that after 6 months of treatment there was a significant improvement of DAS28 on atorvastatin group com-pared to placebo and a decrease of CRP and ESR by 50% and 28%, respectively in treated group compared to placebo18.
The implication of our case for the time being lies in the fact that close monitoring of the RA and the correct treatment not only of the rheumatic disease both also of the CV diseaserepresents a proper solu-tion of the case leading to survival and even to a good quality of life.
We consider that futher presentations of similar cases and longer studies on case series and clinical stu-dies on population in Romania will be beneficial for rheumatologists and cardiologists.
CONCLUSIONS
1. There is an increased risk for developing coro-nary artery disease secondary to early and ac-celerated atherosclerosis in RA patients as de-monstrated once again by the case of our patient.
2. A strict therapeutic monitoring of this patient should be made in accordance with “Treat-to-Target” strategy in order to obtain sustained low disease activity.
3. Of all the CV risk scores, QRISK2 which also in-cludes RA as a CV risk factor, seems to be the most proper.
4. A collaboration between rheumatologists and cardiologists has proved important for improving the patients condition in saving her life.
5. Our case report is in agreement with published medical literature and other similar cases should be further made known to clinicians for a better management of the patients.
Conflict of interest: none declared.
References
1. Avina-Zubieta JA, Choi HK, Sadatsafavi M, et al. Risk of cardiovascu-larmortality in patients with rheumatoid arthritis: a meta-analysis of observational studies.Arthritis Rheum2008;59(12):1690-1697
2. Meune C, Touze E, Trinquart L, Allanore Y. Trends in cardio-vas-cular mortality in patients with rheumatoid arthritis over 50 years: a systematic review and meta-analysis of cohort studies. Rheuma-tol2009;48(10): 1309-13
3. Lindhardsen J, Ahleholff O, Gisloson GH, et al. The risk of myocar-dial infarction in rheumatoid arthritis and diabetes mellitus: a Danish nationwide cohort study. Ann Rheum Dis2011 Jun;70 (6):929-34
4. Chung WS, Lin CL, Peng CL, Chen YF, et al. Rheumatoid arthri-tis and risk of acute myocardial infarction-a nationwide retrospec-tive cohort study.Int J Cardiol. 2013;168(5):4750-4. doi: 10.1016/j. ijcard.2013.07.233. Epub 2013 Aug 2.
5. Choy E, Ganeshalingam K, Semb AG, et al. Cardiovascular risk in rheumatoid arthritis: recent advances in the understanding of the pivotal role of inflammation, risk predictors and the impact of treat-ment. Rheumatology2014;53(12):2143-2154
6. Montecuco F, March F. Common inflammatory mediators orches-trate pathophysiological processesin rheumatoid arthritis and ath-erosclerosis. Rheumatology 2009, 48 (1):11-12
7. Myasoedova E, Crowson CS, Kremers HM, etal.Lipid paradox in rheumatoid arthritis: the impact of serum lipid measures and system-ic infl ammation on the risk of cardiovascular disease. Ann Rheum Dis2011;70:.482-7
8. De Vera MA, Choi H, Abrahamowicz M, et al. Statin discontinua-tion and risk of acute myocardial infarction in patients with rheuma-toid arthritis: a population-based cohort study. Ann Rheum Dis2011 Jun;70(6):1020-4. doi: 10.1136/ard.2010.142455. Epub 2011 Mar 6.
9. Nicola PJ, Maradit-Kremers H, Roger VL, et al.The risk of congestive heart failure in rheumatoid arthritis : a population based study over 46 years. Arthritis Rheum2005 Feb;52 (2)412-20
10. Peters MJL,Symmons DPM,McCareyD, et al.EULAR evidence-based recommendations for cardiovascular risk management in patients with rheumatoid arthritis and other forms of inflammatory arthritis. Ann Rheum Dis, Feb 2010; 69: 325-331 Published Online First 22 September 2009
11. Agca R, Heslinga S.C., Rollefstad S, et al. EULAR recommendations for cardiovascular disease risk management in patients with rheu-matoid arthritis and other forms of inflammatory joint disorders: 2015/2016 update, Annals of the Rheumatic Diseases Published On-line First: 03 October 2016. doi: 10.1136/annrheumdis-2016-209775.
12. Marks J.L. and Edwards C.J., Protective effect of methotrex-ate in patients with rheumatoid arthritis and cardiovascular co-morbidity, Ther Adv Musculoskelet Dis. 2012 Jun; 4(3): 149–157. doi: 10.1177/1759720X11436239.
13. Rezus C, Cardoneanu A, Dima N, et al. Myocardial ischemia in rheu-matic inflammatory diseases, RCC, vol 26, 2016, 263-268.
14. Guin A, Adhikari C.M, Chakraborty S, Sinhamahapatra P, Ghosh A. Effects of disease modifying anti-rheumatic drugs on subclini-cal atherosclerosis and endothelial dysfunction which has been detected in early rheumatoid arthritis: 1-year follow-up study, Se-min Arthritis Rheum. 2013 Aug;43(1):48-54. doi: 10.1016/j.semar-thrit.2012.12.027. Epub 2013 Feb 12.
15. Catella-Lawson F, Reilly MP, Kapoor SC, Cucchiara AJ, DeMarco S, Tournier B, Vyas SN, FitzGerald GA. Cyclooxygenase inhibitors and the antiplatelet effects of aspirin, N Engl J Med. 2001 Dec 20; 345(25):1809-17.
16. Ruyssen-Witrand A, Fautrel B, Saraux A, Le Loët X, Pham T. Car-diovascular risk induced by low-dose corticosteroids in rheumatoid arthritis: a systematic literature review, Joint Bone Spine. 2011 Jan; 78(1):23-30.
17. Hippisley-Cox J, Coupland C, Vinogradova Y, et al. Predicting car-diovascular risk in England and Wales: prospective derivation and validation of QRISK2:BMJ 2008;336:a332 doi:10.1136.
18. McCarey DW, McInnes IB, Madhok R, Hampson R, Scherbakov O, Ford I, Capell HA, Satt. Trial of Atorvastatin in Rheumatoid Ar-thritis (TARA): double-blind, randomised placebo-controlled trial, Lancet. 2004 Jun 19;363(9426):2015-21.
 This work is licensed under a
This work is licensed under a