Alexandrina Nastasa1, Corneliu Iorgulescu1, Stefan Bogdan1, Mohamed Dardari1, Stefan Petre2, Tudor Preda3, Radu Vatasescu1
1 Clinic of Cardiologiy, Emergency Clinical Hospital, Bucharest, Romania
2 Biosense Webster
3 Stereotaxis
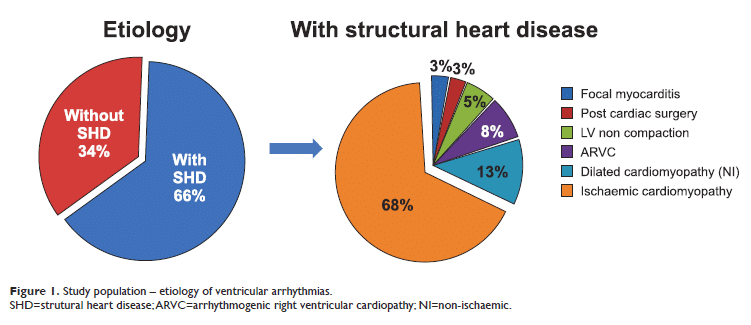
Abstract: Introduction – Remotely-controlled navigation (MNS) has emerged as a novel concept aimed to improve outcomes of catheter ablation for ventricular arrhythmias It has the potential to increase procedural success, decrease procedure time and minimise catheter-related complications. MNS ablation was proved to be as effective and fast compared with manual radiofrequency (RF) but the results regarding unstable and highly mobile cardiac regions are controversial. Purpose – We aimed to describe our experience using magnetic navigation for ablation of ventricular arrhythmias (premature ventricular complexes, sustained ventricular tachycardias or electric storm) in ischaemic and non-ischaemic patients and compare procedural outcomes in relation with arrhythmia type and etiology. Methods – A total of 57 patients (57% males, mean age 51±17 years) with ventricular arrythmias who underwent RF ablation using MNS and CARTO 3 were retrospectively analyzed. Left ventricular sites were targeted by transseptal approach in 53% of the cases, retrograde transaortic in 24% and 8% required epicardial acces via pericardial puncture. Clinical and paraclinical variables as well as procedural aspects were noted and short term screening for reccurence was performed. Results – Acute procedural succes was achieved in 95% of the cases (elimination of clinical arrythmias). Non-inducibility was documented after programmed ventricular stimulation in 80% of the cases. A third of the patients had structurally normal hearts (34%). Among those that had a subsiding cardiopathy, the ischaemic etiology acounted for 68% of the cases where as dilated idiopathic cardiomyopathy was encoutered in 13% of the cases, arrhytmogenic right ventricular cardiopathy 8%, left ventricular non-compaction 5%, postmyocarditis-scar or post-surgical scars in 3%. Difficult ablation sites, such as the proximity of the right bundle branch, coronary cusp or papilary muscle had more frequently previous unsuccessful manual ablations, in all of these cases acute succes was obtained with MNS and the non-inducibility rate was 90% (9 out of 10 patients). Acute succes rates were higher for ischaemic cases but the difference was not statistically signifi cant. Periprocedural complications were noted in 3.5%. Conclusion – MNS is a safe and effective method for catheter ablation for ventricular arrhythmias regardless of etiology or clinical form, with possible superior effects in ischaemic cardiomyopthy with extensive scar and severly dilated LV and for ablation in unstable locations (coronary cusp, papilary muscle).
Keywords: catheter ablation, remote magnetic naviagtion, ventricular arrhythmias
INTRODUCTION
Ventricular arrythmias are increasingly treated by radiofrequency (RF) catheter ablation. In the last 10 years signifi cant technological developments such as electroanatomical mapping, integration of cardiac imaging, and improved catheter design have been implemented to improve procedural outcomes1,2. Proper catheter manipulation to access different areas, very accurate mapping and reliable catheter stability are key issues for a successful treatment in more vulnerable regions (like aortic sinus cusps, which in particular carries a signifi – cant risk for valve perforation or for coronary artery injury) or in diffi cult to reach and/or unstable positions (papillary muscles, very dilated ventricules). The innovation of remote magnetic navigation (MNS) has offered important theoretical advantages in safety due to the atraumatic catheter design, less physical stress and less radiation exposure for physicians3. The magnetic navigation system gives more catheter fl exibility, steering accuracy and reproducibility to navigate to a desired location without the risk of perforation. MNS ablation was proved to be as effective and fast compared with manual RF4 but the results regarding unstable and highly mobile cardiac regions are still debated.
METHODS
All the patients with ventricular arrythmias treated with RF ablation using the magnetic navigation system (Stereotaxis Inc., Niobe II) and CARTO 3 between may 2015 and june 2017 in our laboratory were retrospectively analyzed. The design was descriptive, not comparative (i.e. vs. manual ablation) due to difficulties in selecting a similar control lot and to a high crossover rate for problematic cases (critical ablation sites that had incomplete succes with manual ablation were then re-ablated using MNS). Clinical and paraclinical variables as well as procedural aspects were noted and short term (1 month) screening for reccurence was performed. Results are presented as mean ±SD or median (IQR) and statistical analysis was performed with SPSS 22 and Microsoft Excel Analyse-it software.
STUDY POPULATION
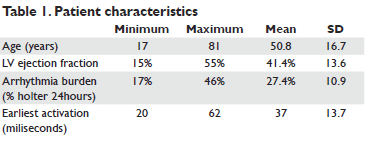
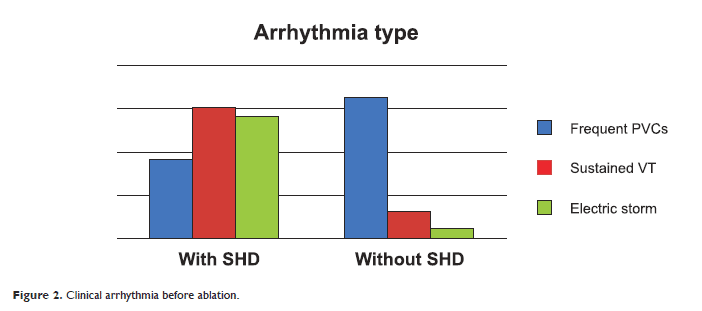
After carefull review of all procedural logs a total of 57 patients with different types of ventricular arrythmias who underwent remote magnetic navigation guided ablation procedures were found. Some of the patients (29%) have had one or more previous manual ablation procedures (mean 1.3±0.5) but experienced arrhythmia reccurence. The study population had predominantly male sex (57%) with a mean age 51±17 years and 34% of the lot had no structural heart disease. Among those that had a subsiding cardiopathy, the ischaemic etiology acounted for 68% of the cases where as dilated idiopathic cardiomyopathy was encoutered in 13% of the cases, arrhytmogenic right ventricular cardiopathy 8%, left ventricular non-compaction 5%, postmyocarditis-scar or post-surgical scars in 3% (Figure 1). Mean left ventricular ejection fraction was 41%±13.6 and the arrhythmia burden on preprocedural holter monitoring was between 17% and 46% with a mean of 27.4±10.9%. Invasive mapping allowed the determination of earliest activation sites of 37±13.7 miliseconds (Table 1). The indication for ablation was sustained ventricular tachycardia in 31%, frequent premature ventricular complexes (PVCs) in 43% and electrical storm in 26% of the cases. Electrical storm was defi ned according to current reccomandations as ≥2 episodes of sustained ventricular tachycardia in 24 hours regardless of the hemodynamic tolerance/ ventricular tachycardia reccuring in less than 5 minutes after conversion or sustained/non-sustained VT for more than 50% of the electrical activity in 24 hours5. In patients with implantable defi brillators the criteria we considered for diagnosis of electric storm were: ≥3 appropriate therapies (including antitachycardia pacing) or ≥2 internal shocks in 24 hours6. In our lot 24% (14 patients) had a previously implanted ICD and 15.5% (9 patients) a CRT-D, the device therapies were programmed “off” durring the procedure and then re-enabled. No periprocedural interference of the magnetic system with device function was observed. In the absence of structural heart disease, clinical arrhythmia was mostly PVCs (16 patients), followed by sustained ventricular tachycardia (3 patients) and one electric storm (Purkinje PVC triggered VF) whereas with structural heart disease the proportions were signifi cantly different: 9 patients with PVC/NSVT, 15 patients with sustained ventricular tachycardia and 13 patients with electric storm as shown in Figure 2
(p=0.0002, Pearson chi-squared test).
RESULTS
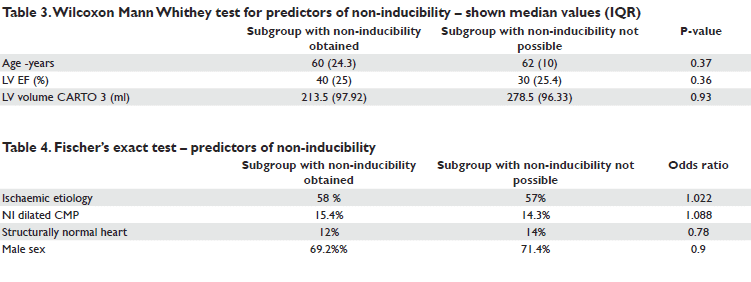
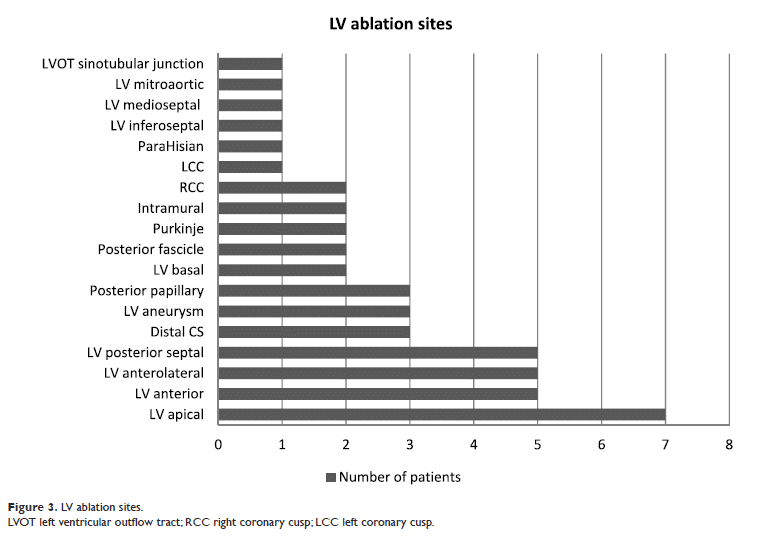
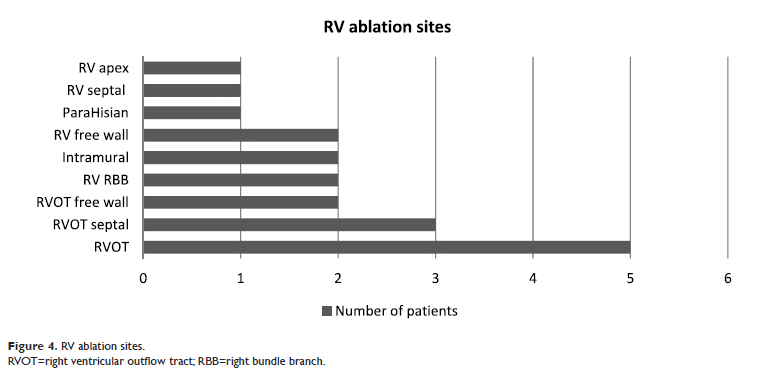
Acute procedural succes was defi ned as complete elimination of the clinical tachycardias and was achieved in 95% (54 of 57 patients) of the cases. Non-inducibility after programmed ventricular stimulation was tested for the patients that presented with sustained or non-sustained VT and was obtained in 80% of the cases. The protocol for stimulation usually included up to three extrastimuli with the coupling interval decreased progressively up to refractory period but not below 200 ms. Patient age had a similar distribution in the two lots (with or without non-inducibility obtained), whereas median left ventricular ejection fraction was smaller and median left ventricular volume was bigger in the subgroup in which non-inducibility was not possible, although not reaching statistic signifi cance – see Table 3. No difference was noted in the frequency of different etiologies between those two subgroups mentioned above (Table 4). Left ventricular sites were targeted by transseptal approach in 63% of the cases, retrograde transaortic in 24%, through coronary sinus ventricular tributaries 4,3% and 8.7% required epicardial acces via pericardial puncture. Among the 3 patients in which acute succes was not possibe, 1 had electrical storm and intramural VT (endo- epicardial mapping was performed, but RF delivery was unsuccesful both endocardially and epicardially) and the other 2 were frequent PVCs with an intramural localisation (LV summit). Classically considered difficult ablation sites, such as the proximity of the His (2 patients) or right bundle branch (2 patients), coronary cusp (3 patients) or papilary muscle (3 patients) had more frequently previous unsuccessful manual ablations and in all cases acute succes was obtained with MNS and the non-inducibility rate was 90% (9 out of 10 patients). Periprocedural complications were noted in 3.5% (2 cases) one was strictly related to the transseptal puncture and the other was an right coronary air embolization throgh pattent foramen ovale during RA-RV mapping in a patient with VT due to ARVC/D (wich was rapidly resolving without any clinical consequence).
DISCUSSION
RF ablation of ischemic ventricular tachycardia has evolved rapidly due to improved technical facilities and understanding of the arrhythmia substrate. The succes rates obtained with remote magnetic navigation for different types of ventricular arrhythmias in our study was 95%, comparable with those described in recent publications. One study reports 80% acute success rate using irrigated magnetic catheters in a small series of 30 patients with ischemic heart disease and electrical storm7. Another publication8 reported a 100% acute success rate using MNS but in a more heterogeneous group including only 30% patients with ischemic heart disease (similar to our study) but in that study, three-quarters of the cases were referred for ablation of ventricular premature beats and only 24% had sustained VT (in our retrospective only 43% of the patients were reffered for PVCs). Our fi ndings suggest that adding remote magnetic navigation has the possibility to increase effectiveness and safety, especially in diffi cult regions (papillary muscle, aortic cusps, His region etc.) but also in patients with very large ventricles. One recent paper that analysed patients with idiopathic ventricular arrhythmias and failed manual ablation that were re-ablated with MNS found that catheter ablation using a MNS system is more effective in selected patients primarily by greater success with ablation in the posterior RVOT and posterior-basal RV (tricuspid annulus)9. In our study, the overall estimated incidence of major procedure related complications was 3.5%, which is comparable to the complication rates in previously reported studies (2.94%)10.
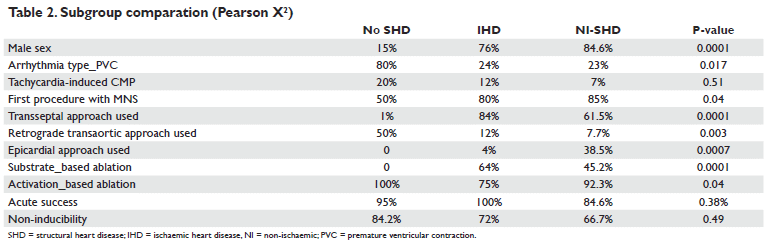
LIMITATIONS
The study was a single-center retrospective study and is subjected to bias typical in retrospective studies. We realize that although no preselection criteria were applied, a certain selection bias could occur. The small number of patients (57 patients) could be also a limitation, although the published studies on this topic are few and also comprised small patient groups. Another important limitation is that effective comparison of ablation results with MNS between subgroups is not possible due to their significant heterogenity (see Table 2) and small number.
CONCLUSION
MNS is a safe and effective method for catheter ablation for ventricular arrhythmias regardless of etiology or clinical form, with possible superior effects in ischaemic cardiomyopthy with extensive scar and severly dilated LV and for ablation in unstable locations (coronary cusp, papilary muscle).
Funding: This work was supported by the Project entitled: “Crearea unui Centru de excelenta in cercetarea clinica si translationala ca suport pentru tratamentul personalizat al urgentelor cardiovasculare – CREDO”
References
1. Khongphatthanayothin A, Kosar E, Nademanee K. “Nonfluoroscopic three-dimensional mapping for arrhythmia ablation: tool or toy?” J Cardiovasc Electrophysiol. 2000;11:239–43
2. Aryana A., d’Avila A, Heist EK, Mela T., Singh JP., Ruskin JN., Reddy VY,. “Remote magnetic navigation to guide endocardial and epicardial catheter mapping of scar-related ventricular tachycardia” Circulation. 2007;115:1191–200
3. Ernst S. “Robotic approach to catheter ablation”. Curr Opin Cardiol. 2008;23:28–31
4. Wu Y., Li KL., Zheng J., Zhang CY., Liu XY., Cui ZM., Yu ZM., Wang RX., Wang W. “Remote magnetic navigation vs. manual navigation for ablation of ventricular tachycardia: a meta-analysis”. Netherlands Heart Journal. 2015;23(10):485-490
5. Sorajja D., Munger TM., Shen WK. “Optimal antiarrhythmic drug therapy for electrical storm”, Journal of Biomedical Research, 2015, 29, 20–34
6. Israel CW., Barold SS., “Electrical storm in patients with an implanted defi brillator: a matter of defi nition”, Annals of Noninvasive Electrocardiology, 2007, 12, 375-82
7. Arya A., Eitel C., Bollmann A.,Wetzel U., Sommer Ph., Gaspar T., Husser D., Piorkowski C., Hindricks G. “Catheter ablation of scarrelated ventricular tachycardia in patients with electrical storm using remote magnetic catheter navigation” PACE 2010;1-7.
8. Di Biase L, Santangeli P., Astudillo V., Conti S., Mohanty P., Mohanty S., Sanches J., Horton R., Thomas B., Burkhardt D., Natale A. “Endoepicardial ablation of ventricular arrhythmias in the left ventricle with the remote magnetic navigation system and the 3.5-mm open irrigated magnetic catheter: Results from a large single-center case-control series” Heart Rhythm 2010;7:1029–1035
9. Kawamura, M., Scheinman, M.M., Tseng, Z.H., Lee BK., Marcus GM., Badhwar N. “Comparison of remote magnetic navigation ablation and manual ablation of idiopathic ventricular arrhythmia after
failed manual ablation J Interv Card Electrophysiol (2017) 48: 35
10. Dinov B., Schönbauer R., Wojdyla-Hordynska A., Braunschweig F., Richter S., Altmann D., Sommer P., Gaspar T., Bollmann A., Wetzel U., Rolf S., Piorkowski C., Hindricks G, Arya A. “Long-term efficacy of single procedure remote magnetic catheter navigation for ablation of ischemic ventricular tachycardia: a retrospective study”, J Cardiovasc Electrophysiol. 2012 May;23(5):499-505.
 This work is licensed under a
This work is licensed under a