Florin Purcarea¹, Adrian Negoita¹, Marin Postu¹
1 “Prof. Dr. C.C. Iliescu” Institute of Emergencies for Cardiovascular Diseases, Bucharest, Romania
Abstract: Myocardial infarction with normal coronary arteries is a syndrome resulting from numerous conditions but the exact cause in a majority of the patients remains unknown. Cigarette smokers and cocaine users are more prone to develop this condition. The possible mechanisms causing myocardial infarction with normal coronary arteries are hypercoagulable states, coronary embolism, an imbalance between oxygen demand and supply, intense sympathetic stimulation, non-atherosclerotic coronary diseases, coronary trauma, coronary vasospasm and endothelial dysfunction. It primarily affects younger individuals and the clinical presentation is similar to that of myocardial infarction with coronary atherosclerosis. Coronary vasospasm can be a cause of life-threatening arrhythmias and cardiac arrest in patients with acute coronary syndrome and no hemodynamically signifi cant coronary artery disease.
Keywords: myocardial infarction, vasospasm, normal coronary arteries, cardiac arrest
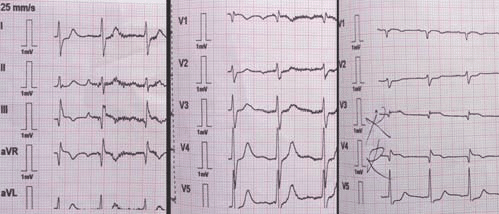
We present a case of a 59-year-old man, smoker, without any relevant medical history, who described intermittent chest pain at rest for 2 hours. The ambulance found the patient at home in cardiac arrest with ventricular fibrillaton on ECG and he was resuscitated after 20 minutes. Post resuscitation ECG showed sinus rhythm, AV=90 bpm, 2 mm ST elevation in avR, DIII and
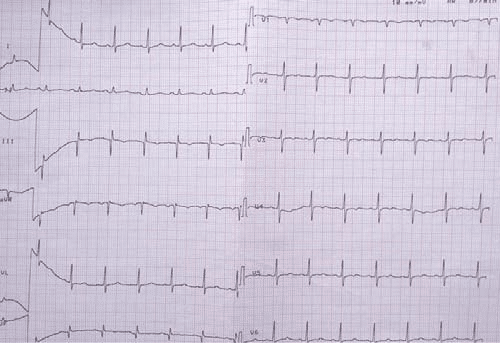
right precordial leads and 1 mm ST segment depression in DI, AVL, V5,V6 (Figure 1). At hospital the pacient was mechanically ventilated, blood pressure was 90/60 mmHg with inotropic support. The ECG was repeted at the emergency room and the ST segment modifications disappeared (Figure 2). Echocardiography showed a mild left ventricular dysfunction – LVEF=50%, inferior
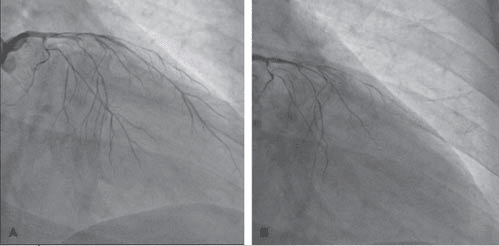
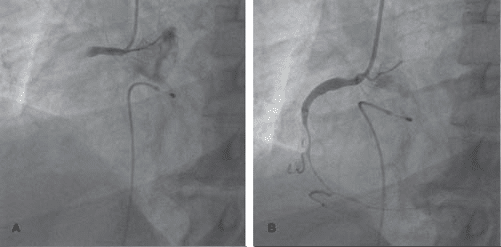
wall hypokinesia, type I diastolic dysfunction, mild mitral regurgitation, normal right ventriculat function. Cardiac troponin was elevated 1.3 ng/ml. The pacient had very-high-risk crietria like hemodynamic instability with life-thereatening arrhytmias and resuscitated cardiac arrest with intermittent ST-elevation. He recived dual antiplatelet therapy and was transferred in the cath lab for emergency coronarography. The first injection in left main showed diffuse severe coronary spasm with occlusion at distal left anterior descending artery and left circumflex artery (Figure
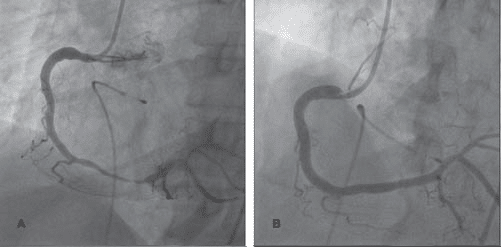
3A,B). After intracoronary nitoglycerine injection, the spasm disappeared and the left coronary artery opened, with normal fl ow (TIMI-3) distally (Figure 4A,B). We didn’t saw hemodynamically significant coronary artery lesions, except a myocardial bridge in the second LAD segment with 40% systolic compression.
Figure 1. Ambulance ECG – sinus rhythm, AV=90 bpm, 2 mm ST elevation in avR, DIII and right precordial leads and 1 mm ST segment depression in DI, AVL, V5,V6.
Figure 2. Hospital ECG – sinus rhythm, AV=90 bpm and the ST segment modifications disappeared.
Figure 3. First injection in left coronary artery – severe difusse vasospasm with distally left anterior descending artery and circumglex artery occlusion.
Figure 4. After intracoronary nitoglycerine injection, the spasm disappeared and the left coronary artery opened, with normal flow (TIMI-3) distally.
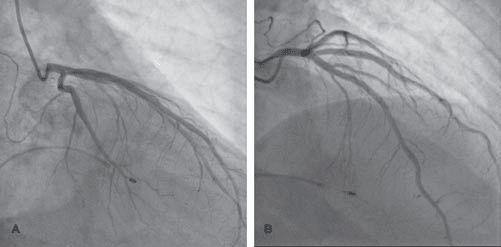
Figure 5. Injection in the right coronary artery showed acute occlusion in the first segment, distal flow TIMI 0-1.
Figure 6. After intracoronary nitoglycerine injection, the spasm disappeared and the right coronary artery opened, with normal flow (TIMI-3) distally.
Before injection in the right coronary artery the ECG showed severe bradycardia with third degree AV block and temporary cardiac stimulation was done. The injection in the right coronary artery showed acute occlusion in the first segment, distal flow TIMI 0 (Figure 5A,B). At that moment we had a problem to decide if that was a thrombotic occlusion or a severe spasm similar to the left coronary artery. The first step was to inject intracoronary nitroglycerine. After that, the right coronary artery opened and after few minutes the distal flow was normal (TIMI-3) witout any hemodynamically significant coronary artery lesions (Figure 6A,B). We considered the severe coronary spasm responsible for the right coronary artery oclusion and we fi nished our job in the cath lab. The patient was transferred in the critical care unit.
The clinical evolution was good, he was discharged after 1 month, hemodynamically stable with normal left ventricular function, but with neurological sequelae postresuscitation and was transferred in a neurological rehabilitation center. The medical treatment at discharge was duble antiplatelet therapy with aspirin and clopidogrelum, calcium channel blocker – diltiazem
and statin.
DISCUSSIONS
Although plaque rupture is the major cause of acute myocardial infarction, vasospasm is also known as a potential cause of that pathology. However, it is very rare and is sometimes difficult to diagnose correctly. Coronary artery vasospasm, or smooth muscle constriction of the coronary artery, is an important cause of chest pain syndromes that can lead to myocardial infarction, ventricular arrhythmias and sudden death. Cigarette smokers and cocaine users are more prone to develop this condition. Our patient was a smoker but we didn’t have laboratory tests to confirm cocaine use as a potentially cause of vasospasm. We initially thought plaque rupture with thrombus formation might be the cause of acute myocardial infarction judging from the angiogram of the right coronary artery. This patient had been diagnosed as having vasospasm using the nitroglycerine intracoronary injection response. It is not easy to judge from the angiogram that the cause
of coronary occlusion in patients with acute myocardial infarction is vasospasm and sometime you have to use special invasive techniques. We didn’t use intravascular ultrasound or OCT to check the coronary wall structure because the fi nal angiographic result was a good one after nitroglycerine injection and we consider the patient hemodynamic instability in that moment needed urgent transfer to intensive care unit. Arrhythmias may occur with severe vasospastic angina. Both atrioventricular conduction abnormalities and ventricular arrhythmias can cause life-threatening hemodynamic deterioration and syncope. Coronary vasospasm has been identifi ed as an important cause of out-of-hospital cardiac arrest. The risk of sudden death is approximately 2% and is most common in patients with multi vessel spasm as it happened in our patient.
Conflict of interest: none declared.
References
1. Yasue H, Nakagawa H, Itoh T, Harada E, Mizuno Y. Coronary artery spasm-clinical features, diagnosis, pathogenesis, and treatment. J Cardiol. 2008 Feb. 51(1):2-17
2. Onaka H, Hirota Y, Shimada S, et al. Prognostic significance of the pattern of multivessel spasm in patients with variant angina. Jpn Circ J. 1999 Jul. 63(7):509-13
3. Kobayashi N, Hata N, Shimura T, et al. Characteristics of patients with cardiac arrest caused by coronary vasospasm. Circ J. 2013. 77(3):673- 8
4. Stern S, Bayes de Luna A. Coronary artery spasm: a 2009 update. Circulation. 2009 May 12. 119(18):2531-4.
5. Hung MJ, Hu P, Hung MY. Coronary Artery Spasm: Review and Update. Int J Med Sci 2014; 11(11):1161-1171
6. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation Restricted accessMarco Roffi , Carlo Patrono, Jean-Philippe Collet, Christian Mueller, Marco Valgimigli, Felicita Andreotti, Jeroen J. Bax, Michael A. Borger, Carlos Brotons, Derek P. Chew, Baris Gencer, Gerd Hasenfuss, Keld Kjeldsen, Patrizio Lancellotti, Ulf Landmesser, Julinda Mehilli, Debabrata Mukherjee, Robert F. Storey, Stephan Windecker DOI: http://dx.doi.org/10.1093/eurheartj/ehv320 267-315.
 This work is licensed under a
This work is licensed under a