Alexandru Mihailovici1, Roxana Enache2, Emanuel Stoica2, Marin Postu2
1 Department of Cardiology, Emergency Country Hospital Craiova, Romania
2 “Prof. Dr. C.C. Iliescu” Emergency Institute for Cardiovascular Diseases, Bucharest, Romania
The coronary arterial fistula is a rare abnormality that links one or more of the coronary arteries, and a cardiac chamber or a great vessel. It is also known as coronary arteriovenous malformation1. The coronary artery fistula’s etiology is not very well known, but most of the fistulas have a congenital origin. Usually they are spotted by accident, after a cardiac surgery (such as valve replacement), angiography, coronary artery bypass grafting and after repeated myocardial biopsies in cardiac transplantation2,3. Clinically, most of the fistulas are asymptomatic in the first two decades, especially when they are small. Indeed, a few of them may close spontaneously. If not, the frequency of both symptoms and complications increases4. The symptoms frequency is increased in older patients, presenting dyspnea or angina of effort and occasionally arrhythmias. Congestive cardiac failure can appear on patients with large left-to-right shunts especially during infancy and occasionally in the neonatal period5. Most of the complications are: ‘steal’ from the adjacent myocardium causing myocardial ischemia, thrombosis and embolism, cardiac failure, rupture of the fistula, endarteritis and arrhythmias (atrial fibrillation)1,6-8. One of the rare complications in the coronary arterial fistula is thrombosis that may cause an acute myocardial infarction, also atrial and ventricular arrhythmias9. Some cases of hemopericardium due to spontaneous rupture of the aneurysmal fistula have been reported10. Another complication is angina that may be due to coronary artery steal.
CASE REPORT
We will present the case of a 66 year old patient, from the country side, with multiple cardiovascular
risk factors (hypertension, dyslipidemia, obesity), with cirrhosis for 9 years, which was transferred through Ro-STEMI program to our unit for chest pain, that appeared 4 hours before the presentation, accompanied by orthopnea.
On admission the patient is in a good clinical condition, aware, oriented to time and space, bilateral vesicular murmur (VM), bilateral basal crepitation, Sa O2 = 96%, blood pressure (BP) 140/80 mmHg, heart rate (HR) 68/min, regular heart sounds without murmurs heart, abdomen distended, hepatomegaly. The ECG reveals a basic sinus rhythm being about a heart rate of 100 bpm, QRS axis at 45°, is observed ST segment elevation in the anterior territory (from V1 to V6) of 5mm, QS from V1 to V4, Q in V5, high P wave in DII. Blood analyses show myocardial necrosis enzymes increased, NTproBNP 6998 pg/ml, Troponin I 4.57 ng/ ml. The Echocardiography finds diastolic LV diameter 42 mm, systolic LV diameter 30 mm, interventricular septum 11mm, posterior wall 10 mm, LA 36 mm, RV 27 mm, Ao ring 20 mm, Ao asc 32 mm, RA 39 mm, LVEF 50%, inferior vena cava 16 mm with inspiratory collapse. Mild mitral regurgitation, inferior wall akinesia, free pericardium. Pulmonary artery with normal dimensions, no pulmonary hypertension.
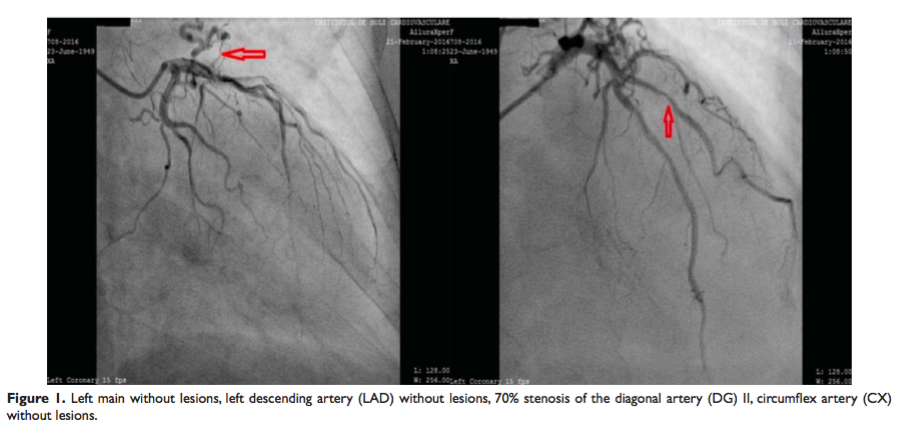
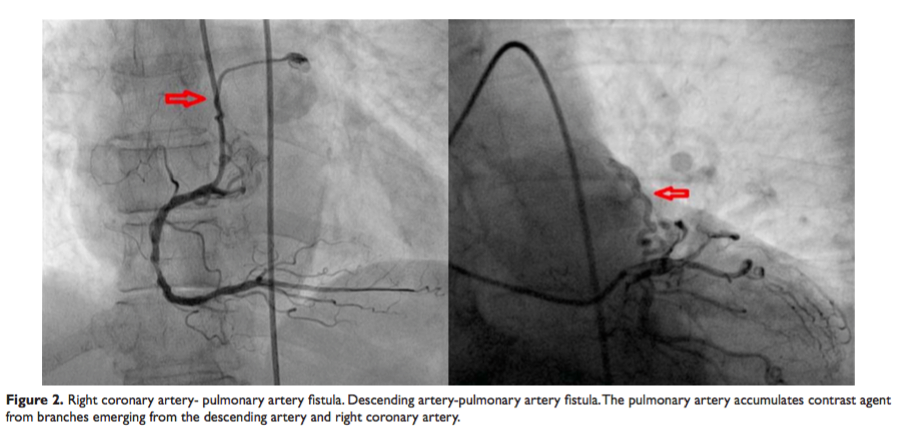
Coronary angiography shows left main without lesions, left anterior descending artery (LAD) without lesion, 70% stenosis of the diagonal artery (DG) II, circumflex artery (CX) without lesions. Also, the angiography has revealed the existence of two fistula (between the proximal segment of right artery coronary and pulmonary artery, left anterior artery descending and pulmonary artery) without hemodynamic significance (Figure 1 and 2).
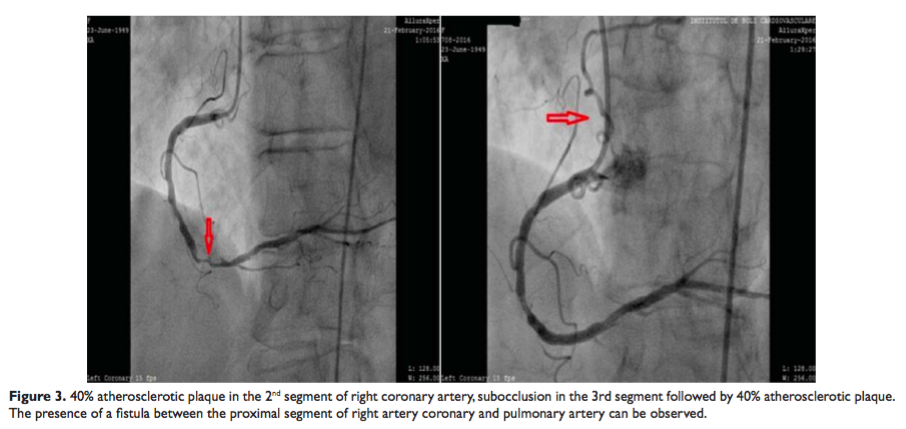
Contrast injection in the right coronary artery shows 40% atherosclerotic plaque in the 2nd segment of right coronary artery, subocclusion in the 3rd segment followed by 40% atherosclerotic plaque (Figure 3).
As a result, an angioplasty with drug eluting stent was performed in a patient with inferior-posteriorlateral STEMI after 4 hours before the presentation. After 2 days the patient was reevaluated by echocardiography, cardiac chambers were within normal limits, aorta and pulmonary artery with normal dimensions, no pulmonary hypertension.
In conclusion, pulmonary arteriovenous fistulae are rare, especially those with a common outflow. Establishing a diagnosis and understanding their haemodynamics are essential, otherwise they would only be a simple scientific curiosity.
Conflict of interests: none declared.
References
1. Wilde P, Watt I. Congenital coronary artery fistulae: six new cases with a collective review. Clin Radiol. 1980;31:301–311.
2. Reidy JF, Anjos RT, Qureshi SA, Baker EJ, Tynan MJ. Transcatheter embolization in the treatment of coronary artery fistulas. J Am Coll Cardiol. 1991;18:187–192.
3. Somers JM, Verney GI. Coronary cameral fistulae following heart transplantation. Clin Radioly. 1991;44:419–421.
4. Liberthson RR, Sagar K, Berkoben JP, Weintraub RM, Levine FH. Congenital coronary arteriovenous fistula: report of 13 patients, review of the literature and delineation of management. Circulation. 1979;59:849–854.
5. Khan MD, Qureshi SA, Rosenthal E, Sharland GK. Neonatal transcatheter occlusion of a large coronary artery fistula with Amplatzer duct occluder. Catheter Cardiovasc Interv. 2003;60:282–286.
6. McNamara JJ, Gross RE. Congenital coronary artery fistula. Surgery. 1969;65:59–69.
7. Alkhulaifi AM, Horner SM, Pugsley WB, Swanton RH. Coronary artery fistulas presenting with bacterial endocarditis. Ann Thorac Surg. 1995;60:202–204.
8. Skimming JW, Walls JT. Congenital coronary artery fistula suggesting a “steal phenomenon” in a neonate. Pediatr Cardiol. 1993;14:174– 175.
9. Ramo OJ, Totterman KJ, Harjula AL. Thrombosed coronary artery fistula as a cause of paroxysmal atrial filbrillation and ventricular arrhythmia. Cardiovasc Surg. 1994;2:720–722.
10. Bauer HH, Allmendinger PD, Flaherty J, Owlia D, Rossi MA, Chen C. Congenital coronary arteriovenous fistula: spontaneous rupture and cardiac tamponade. Ann Thorac Surg. 1996;62:1521–1523.
11. Oshiro K, Shimabukuro M, Nakada Y, Chibana T, Yoshida H, Nagamine F, Sunagawa R, Gushiken M, Murakami K, Mimura G. Multiple coronary LV fistulas: demonstration of coronary steal phenomenon by stress thallium scintigraphy and exercise haemodynamics. Am Heart J. 1990;120:217–219.
 This work is licensed under a
This work is licensed under a