Larisa Anghel1, Liviu Macovei1,2, Cătălina Arsenescu Georgescu1,2
1 Cardiovascular Diseases Institute ,,Prof. Dr. George I. M. Georgescu”, Iaşi, Romania
2 University of Medicine and Pharmacy „Grigore T. Popa”, Iaşi, Romania
Abstract: Objectives – The aim of our study was to analyze how an increase in QRS complex duration in left bundle branch block (LBBB) patients infl uence the risk for coronary lesions or arrhythmias. Methods – We prospectively studied 323 left bundle branch block patients admitted from January 2011 to June 2013 in Georgescu Institute of Cardiovascular Diseases. The median follow up was 7 days (hospitalization period). Patients were divided into two groups according to their QRS duration (<140 ms=”” and=”” 140=”” ms=”” in=”” order=”” to=”” analyze=”” how=”” an=”” increase=”” in=”” qrs=”” complex=”” duration=”” affects=”” mortality=”” and=”” br=””> baseline data in the study population. Results – The first important fi nding of our study is that prolonged QRS duration in LBBB patients is associated with a higher risk of coronary lesions, two and especially three coronary artery disease, an increased left ventricular systolic and diastolic dysfunction and an elevated risk of ventricular tachycardia. Those with a QRS duration ≥140 ms were more likely to have a decreased ejection fraction (EF) <50% (p= 0.001), more than half of them having an ejection fraction less than 30%. Conclusions – Our study demonstrates that a prolonged QRS duration is associated with a more reserved prognostic in LBBB patients.
Keywords: prognostic, LBBB, coronary lesions
INTRODUCTION
The relation of QRS duration, specifically those with left bundle branch block (LBBB), to adverse outcome is controversial, but most studies show LBBB to be an independent prognostic marker for mortality1. In previous studies a prolonged QRS interval on a 12-lead electrocardiogram (ECG) has been associated with a higher incidence of sudden cardiac death and decrease in overall survival2,3. The aim of our study was to analyze how an increase in QRS complex duration in left bundle branch block (LBBB) patients affects the left ventricular function and the risk for arrhythmias or coronary lesions.
METHODS
With a view to assessing the meaning of left bundle branch block associated with ventricular dysfunction and atherosclerotic coronary disease, we prospectively studied all the patients admitted from January 2011 to June 2013 in Georgescu Institute of Cardiovascular Diseases and 323 of them had left bundle branch block. All electrocardiograms were analyzed and the treating cardiologist determined the presence of left bundle-branch block. The electrocardiograms were classified according to the standardized guidelines, including LBBB not otherwise known to be old (new or presumably new LBBB) or LBBB known to be old. LBBB chronicity was determined by comparison with the most recent ECG available. If no prior ECG was available for comparison, patients were classified as having a presumably new LBBB. The ECG QRS duration was obtained from the ECG performed at admission, and was recorded based on the treating physician interpretation of QRS width. Patients were excluded if they were younger than 30 years, have myocardial infarction, moderate or severe aortic or mitral stenosis, because their heart failure
may have been at least partially by another etiology. We excluded patients with previous placement of a permanent pacemaker or automated implantable cardiac defibrillator (as ECG tracings were unavailable for review to assess whether cardiac pacing could have artifi cially widened the QRS interval). Also, we excluded patients which declined authorization for the use of their medical records for research. According to their QRS duration (QRS duration <140 ms and QRS ≥140 ms), 323 patients with left bundle-branch block who met the inclusion and exclusion criteria mentioned above were divided into two groups: – 159 patients with a QRS complex duration between 120-140 ms; – 164 patients with a QRS complex duration ≥140 ms. There wasn’t a specific reason for a cutoff of 140 ms and this arrangement was made in order to be able to analyze how an increase in QRS complex duration affects mortality and baseline data in the study population. The median follow up was 7 days (hospitalization period). Data collected included basic demographic information, characteristics of chest pain and associated symptoms, cardiac history and risk factors, medications, treatment, disposition, ECG, echocardiography, cardiac markers and angiographic data. All subjects were reviewed for the existence of hypertension, diabetes
mellitus, hyperlipidemia, smoking, ischemic heart disease, cardiomyopathy, valvular heart disease and cerebrovascular disease. Statistical analyzes were performed using the Statistical
Program for Social Sciences (version 17.0 SPSS Inc.). Data were labeled as nominal or quantitative variables. Nominal variables were described using frequencies. Quantitative variables were tested for nominality of distribution by means of Kolmogorov-Smirnov test and were described by median and percentiles or by mean and standard deviation, whenever the case. The frequencies of nominal variables were compared with a chi-square test. Comparisons were made among patients with QRS duration <140 ms and those with QRS duration ≥140 ms. A p value of <0.05
was considered statistically signifi cant. The study was approved by the Committee on the Conduct on Human Research of University of Medicine and Pharmacy, Iaşi.
RESULTS
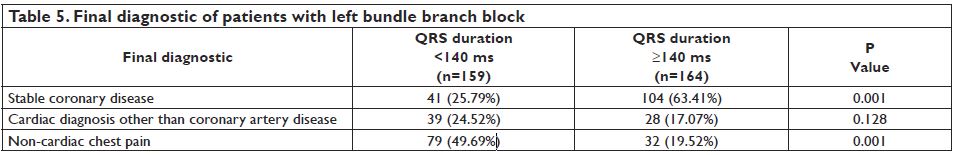
A sum-total of 402 patients with left bundle branch block was admitted between January 2011 and June 2013 in the Cardiovascular Diseases Institute Iasi, but only 323 were finally included in the study, after exclusion of subjects with valvular heart disease, permanent pacemaker or automated implantable cardiac defibrillator or myocardial infarction. According to the QRS duration using a cutoff of 140 ms, we divided the patients in two groups. A total of 159 subjects had QRS duration <140 ms and 164 had QRS duration ≥140 ms. The baseline characteristics of patients with QRS
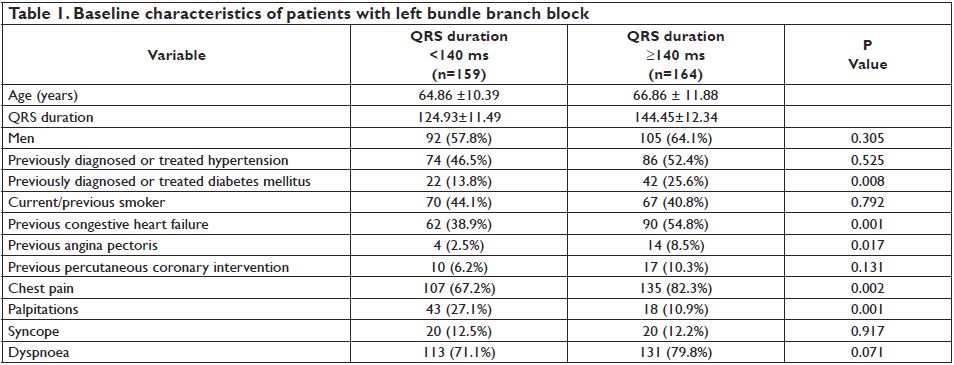
duration <140 ms and those with QRS duration ≥140 ms are shown in Table 1. Patients with QRS duration ≥140 ms were older, predominantly males and with new or presumably new left bundle branch block. They were more likely to have a prior history of diabetes mellitus and cardiovascular events, including hypertension, congestive heart failure, angina and percutaneous coronary intervention. Statistically significant differences in terms of baseline characteristics were found in previously diagnosed or treated diabetes mellitus, prior congestive heart failure and angina pectoris, common in patients with QRS duration ≥140 ms (p = 0.008, p = 0.001 and p = 0.017). Most of the previous percutaneous coronary interventions in patients with QRS duration ≥140 were made on the left anterior descendent artery (LAD). Chest pain and dyspnoea were the most frequent symptoms at presentation. Out of the 323 LBBB patients in our study, 242 (74.92%) reported chest pain at presentation and 244 (75.54%) reported dyspnoea. Of the patients with QRS duration ≥140 ms, 135 (82.3%) presented with chest pain and 82 (60.74%) were men. The other symptoms, in order of frequency were palpitations and syncope, with statistically significant differences only for chest pain and palpitations (Table 1). We also studied the echocardiographic characteristics of patients with left bundle branch block. Patients with QRS duration ≥140 ms were more likely to have a decreased ejection fraction (EF) <50% (111 patients (67.7%) vs. 81 (50.9%), p= 0.001), more than half of them having an ejection fraction less than 30%. There were also statistically signifi cant differences between end-diastolic and end-sistolic diameters and volumes
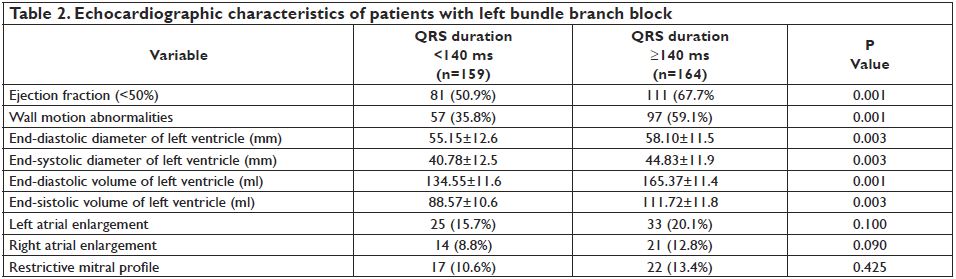
which were more elevated in those with QRS duration ≥140 ms (p = 0.003). We performed on each study participant the left atrial (LA) volume. Approximately 1 of 5 patients with QRS duration ≥140 ms had LA enlargement, but without statistically signifi cant differences between the two groups (20.1% vs. 15.7%, p = 0.100). The baseline echocardiographic characteristics of patients with left bundle branch block divided in two groups are shown in Table 2. In order to study the in-hospital outcome of patients with left bundle branch block according to their QRS duration, we found a more frequent association between a prolonged QRS duration ≥140 ms and the risk of ventricular tachycardia, but without statistically significant differences between the two groups, as
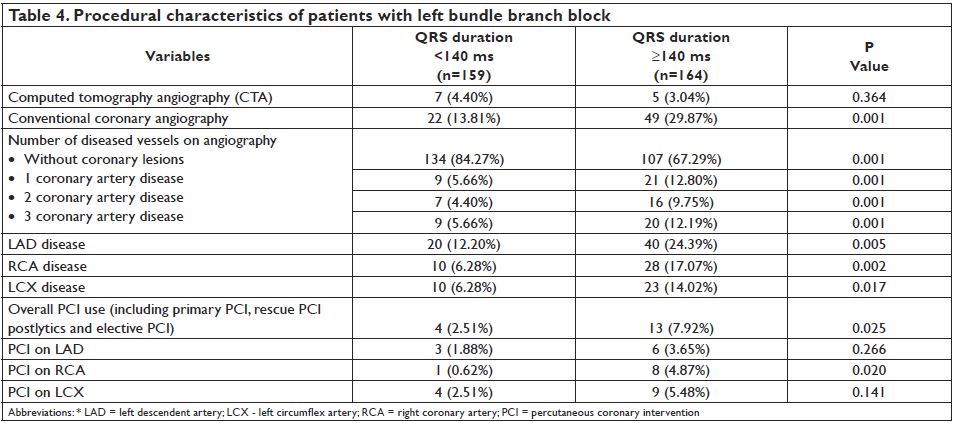
shown in Table 3. All the patients were on telemetry wards and in all cases ventricular tachycardia was monomorphic, sustained or nonsustained, but hemodynamically stable. In our study, conventional coronary angiography was performed in 49 (29.87%) patients with QRS ≥140 ms and 5 (3.04%) patients were evaluated using computed tomography angiography (CTA). This may be explained by the fact that in our study we excluded patients with myocardial infarction and almost half of patients with chest pain and new left bundle branch block have a myocardial infarction. Most of the patients with a QRS duration ≥140 ms, had no vessel disease (67.29%) and when this was the case, it was frequently localized on the left descendent artery (24.39%). In contrast, only
15.72% of patients with a QRS duration <140 ms, had coronary lesions. The majority of patients with QRS duration ≥140 ms had two or three-vessel coronary lesions (12.19% vs. 5.66%) (Table 4).
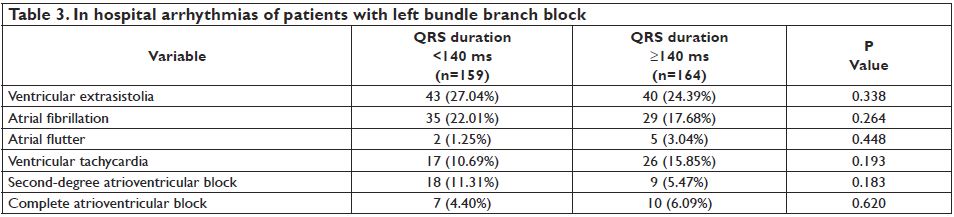
Of the patients with QRS duration ≥140 ms, 104 (63.41%) had final diagnoses of stable angina, 28 (17.07%) had cardiac diagnoses other than coronary artery disease and 32 (19.52%) were diagnosed with noncardiac chest pain. In patients with QRS duration <140 ms the most frequent fi nal diagnostic was noncardiac chest pain (49.69%) and the differences were statistically significant between stable angina and noncardiac chest pain in these two groups (Table 5). Patients with QRS ≥140 ms were more likely to receive diuretics, angiotensin converting enzime-inhibitors, beta-blockers, calcium channel blockers, aspirin, clopidogrel and statins. There was no difference in the utilization of antiaritmics and oral antiplatelet agents, between the two groups.
In this study we noticed that a prolonged QRS duration in patients with left bundle branch block is associated with an increased risk of coronary lesions and stable coronary disease. Also, patients with a QRS duration ≥140 ms had more severe coronary lesions, especially two or three-vessel coronary lesions. In the same time, these patients commonly receive coronary angioplasty as compared with patients with a QRS duration <140 ms.
DISCUSSION
The first important finding of our study is that prolonged QRS duration in patients with LBBB is associated with a higher risk of coronary lesions and stable coronary artery disease. Furthermore, in our study, patients with QRS duration ≥140 ms had more frequently critical coronary lesions, two and especially three coronary artery disease. In the same time, these patients were reffered for percutaneous coronary intervention more frequently that those with QRS duration <140 ms. In previous studies, prolonged QRS duration was an independent predictor of cardiac death and nonfatal infarction6-9 in patients referred for noninvasive evaluation of myocardial ischemia, and in patients with suspected acute coronary syndrome, QRS prolongation predicted in-hospital and 1-year mortality10. Because the rate of cardiovascular mortality in patients with coronary artery disease (CAD) and concomitant LBBB is higher than that of patients with a similar extent of CAD but without LBBB an effective method of identifying CAD in those with LBBB might be helpful10. QRS duration is a readily available “front-line” clinical indicator of increased risk of sudden cardiac death, suggesting consideration of cardiac function assessment or evaluation of coronary artery disease in patients with suspected heart failure in particular11-15. In our study patients with QRS duration ≥140 ms were more likely to have a prior history of angina pectoris which may be a marker of an underlying coronary artery disease that progresses to adverse outcomes. However, several studies have failed to identify a relationship between the location of coronary stenosis and the presence of LBBB16, and in a Framingham Study cohort, QRS duration was not a precursor of coronary disease over 18 years of follow-up17. In a recent study published by Aro et al. it has been suggested that, in a general population, intraventricular conduction delay, including LBBB is associated with an increased risk of cardiac and arrhythmic death. Although there were no differences in the history of myocardial infarction or angina pectoris between the groups, it is possible
that LBBB to be a marker of an underlying subclinical coronary artery disease that progresses to adverse outcomes18. Another important fi nding from our study was that a QRS duration of ≥140 ms in patients with left bundle branch block is associated with an increased left ventricular systolic and diastolic dysfunction and an elevated risk of ventricular tachycardia. It has long been recognized that when associated with heart disease, prolonged QRS duration in an ECG is an independent predictor of adverse outcome. In most patients with systolic left ventricular dysfunction,
QRS prolongation presents as LBBB3, and in these patients, increased QRS duration is associated with a worse prognosis6,7. For patients with coronary artery disease plus depressed ventricular function and nonsustained ventricular tachycardia, QRS prolongation resulting from LBBB has been associated with a 50% increase in the risk of both arrhythmic and total mortality8. The link between this ECG pattern and malignant arrhythmias is supported by accentuated repolarization abnormalities before the onset of arrhythmia. The prolonged QRS with the perturbed depolarization may play a direct role in sudden cardiac death via the facilitation of reentrant tachyarrhythmias2. In our study, there was no difference in the mortality, applied only to the hospitalization, between the two groups, only one person from each group died. Our study is one of the fewest studies that evaluated the risk of atrioventricular blocks in patients with LBBB and we observed a more elevated, but not statistically significant, risk of third degree atrioventricular block in patients with a QRS duration ≥140 ms. Bradyarrhythmias may not be the most probable explanation for the increased mortality associated with prolonged QRS duration either in the previous studies. Even though future high-degree atrioventricular block is strongly associated with the presence of bundle branch block, especially LBBB, the risk of sudden death due to bradyarrhythmia is low even with high-risk BBB, and pacemaker treatment has not been found to diminish
the risk of death in these patients19-23. The strengths of our study include the large number of baseline and echocardiographic characteristics of subjects. The diagnostic of coronary artery disease was based not only on past medical history and clinical examination, but also by conventional coronary angiography and computed tomography angiography. A limitation of our study is the impossibility of long and complete follow-up of these subjects. In conclusion, the results of our study sustain that patients with left bundle branch block in the setting of a prolonged QRS duration have a more reserved prognosis because of the left ventricular dysfunction and in-hospital arrhythmias. On the other hand, any patient with chest pain and LBBB should be evaluated through coronary angiography because of the high risk of critical coronary lesions, two and especially three coronary artery disease. In particular, LBBB in a 12-lead ECG carries a substantial risk of subsequent cardiac death and sudden arrhythmic death, and its presence should alert physicians to the need for a careful evaluation, including echocardiography, of subclinical heart disease even in asymptomatic subjects.
Acknowledgements and declarations: No persons other than those listed as authors have made substantial contributions to this manuscript. The study is not supported by granting or commercial sources of funding. All authors had access to the data, participated in the preparation of this manuscript and meet criteria for authorship as established by the International
Committee of Medical Journal Editors.
Conflicts of interest: none declared.
References
1. Badheka AO, Singh V, Patel NJ, Deshmukh A, Shah N, Chothani A, Mehta K, Grover P, Savani GT, Gupta S, Rathod A, Marzouka GR, Mitrani RD, Moscucci M, Cohen MG. QRS duration on electrocardiography and cardiovascular mortality (from the National Health and Nutrition Examination Survey-III). Am J Cardiol 2013; 112:671-677.
2. Kurl S, Mäkikallio TH, Rautaharju P, Kiviniemi V, Laukkanen JA. Duration of QRS complex in resting electrocardiogram is a predictor of sudden cardiac death in men. Circulation 2012; 125: 2588-2594.
3. Brenyo A, Zaręba W. Prognostic significance of QRS duration and morphology. Cardiol J 2011; 18:8-17.
4. Kushner FG, Hand M, Smith SC, King SB, Anderson JL, Antman EM, Bailey SR, Bates ER, Blankenship JC, Casey DE, Green LA, Hochman JS, Jacobs AK, Krumholz HM, Morrison DA, Ornato JP, Pearle DL, Peterson ED, Sloan MA, Whitlow PL, Williams DO. 2009 Focused Updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2009; 54: 2205-2241.
5. The Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC). Eur Heart J 2012; 33: 2569–2619.
6. Anghel L, Arsenescu Georgescu C. The LBBB-biased CAD, Romanian Journal of Artistic Creativity 2013; 1: 160-166.
7. Wang NC, Maggioni AP, Konstam MA, Zannad F, Krasa HB, Burnett JC, Grinfeld L, Swedberg K, Udelson JE, Cook T, Traver B, Zimmer C, Orlandi C, Gheorghiade M. Clinical implications of QRS duration in patients hospitalized with worsening heart failure and reduced left ventricular ejection fraction. JAMA 2008; 299: 2656 –2666.
8. Anghel L, Arsenescu Georgescu C. Particularities of coronary artery disease in hypertensive patients with left bundle branch block, Maedica- a Journal of Clinical Cardiology 2014; 9: 333-337.
9. Schinkel AF, Elhendy A, van Domburg RT, Biagini E, Rizzello V, Veltman CE, Ten Kate GL, Sijbrands EJ, Akkerhuis KM, Geleijnse ML, Ten Cate FJ, Simoons ML, Bax JJ, Poldermans D. Prognostic significance of QRS duration in patients with suspected coronary artery disease referred for noninvasive evaluation of myocardial ischemia. Am J Cardiol 2009; 104: 1490–1493.
10. Baslaib F, Alkaabi S, Yan AT, Yan RT, Dorian P, Nanthakumar K, Casanova A, Goodman SG. QRS prolongation in patients with acute coronary syndromes. Am Heart J 2010; 159: 593–598.
11. Anghel L, Arsenescu Georgescu C. Intermittent left bundle branch block – a diagnostic dilemma. Romanian Journal of Cardiology 2015; 25(2): 175-179.
12. Yeo KK, Li S, Amsterdam EA, Wang TY, Bhatt DL, Saucedo JF, Kontos MC, Roe MT, French WJ. Comparison of clinical characteristics, treatments and outcomes of patients with ST-elevation acute myocardial infarction with versus without new or presumed new left bundle branch block (from NCDR). Am J Cardiol 2012; 109:497–501.
13. Neeland IJ, Kontos MC, de Lemos JA. Evolving considerations in the management of patients with left bundle branch block and suspected myocardial infarction. J Am Coll Cardiol 2012; 60:96-105.
14. Jain S, Ting HT, Bell M, Bjerke CM, Lennon RJ, Gersh BJ, Rihal CS, Prasad A. Utility of left bundle branch block as a diagnostic criterion for acute myocardial infarction. Am J Cardiol 2011; 107:1111-1116.
15. Mehta N, Huang HD, Bandeali S, Wilson JM, Birnbaum Y. Prevalence of acute myocardial infarction in patients with presumably new left bundle-branch block. J Electrocardiol 2012; 45: 361-367.
16. Freedman RA, Alderman EL, Sheffi eld LT, Saporito M, Fisher LD. Bundle branch block in patients with chronic coronary artery disease: angiographic correlates and prognostic signifi cance. J Am Coll Cardiol 1987; 10:73–80.
17. Kreger BE, Anderson KM, Levy D. QRS interval fails to predict coronary disease incidence: the Framingham Study. Arch Intern Med 1991; 151:1365–1368.
18. Aro AL, Anttonen O, Tikkanen JT, Junttila MJ, Kerola T, Rissanen HA, Reunanen A, Huikuri HV. Intraventricular conduction delay in a standard 12-lead electrocardiogram as a predictor of mortality in the general population. Circ Arrhythm Electrophysiol 2011; 4:704-710.
19. Strauss DG. Importance of defi ning left bundle branch block. J Electrocardiol 2012; 45: 505-507.
20. Kumar V, Venkataraman R, Aljaroudi W, Osorio J, Heo J, Iskandrian AE, Hage FG. Implications of left bundle branch block in patient treatment. Am J Cardiol 2013; 111:291-300.
21. Uebleis C, Hoyer X, Van Kriekinge SD, Schuessler F, Laubender RP, Becker A, Lehner S, Todica A, Haug A, Bartenstein P, Cumming P, Germano G, Hacker M. Association between left ventricular mechanical dyssynchrony with myocardial perfusion and functional parameters in patients with left bundle branch block. J Nucl Cardiol 2013;
20:253–261.
22. Zaręba W. Comparison of clinical trials evaluating cardiac resynchronization therapy in mild to moderate heart failure. Cardiol J 2010; 17:543–548.
23. Gregg RE, Helfenbein ED, Babaeizadeh S. New ST-segment elevation myocardial infarction criteria for left bundle branch block based on QRS area. J Electrocardiol 2013; 46: 528-534.
 This work is licensed under a
This work is licensed under a