Daniel Gherasim1, Maria Jalbă1, Marina Lupu2, Dan Deleanu1, Carmen Ginghină1,3, Eduard Apetrei1,3
1 “Prof.Dr. C.C. Iliescu” Emergency Institute for Cardiovascular Disease, Bucharest
2 “Panduri” Medical Center, Bucharest
3 “Carol Davila” University of Medicine and Pharmacy, Cardiology Department, Bucharest
Contact address:
Dr. Daniel Gherasim, Clinical Cardiology, “Prof. Dr. C. C. Iliescu” Emergency Institute for Cardiovascular Disease, Bucharest, Sos.Fundeni 258, Sector 2, Bucharest, Zip code 022328
E-mail: gherasimdanro@yahoo.com
Abstract: Purpose – Exercise stress testing (ET) is a valuable screening test for the detection of obstructive coronary artery disease (CAD). Previous studies from the literature show an overall sensitivity of 68% and specificity of 77% with variable predictive values depending on pretest probability. The purpose of the current study was to evaluate the diagnostic value of ET in the modern era of cardiology. Aims – This is a retrospective study on 404 patients with chest pain suggestive for angina and with no history of ischaemic heart disease, which have performed a treadmill exercise stress testing and than after and a selective coronary angiography, from October 2008 to January 2013. The coronary angiography was performed between 2 – 60 days after the test. A positive test was defined as horizontal or downsloping ST segment depression or elevation of 0.1 mV (1mm) or slowly upsloping of 1.5 mm (the slowly upsloping was defined as <1 mv/s). Coronary arteries stenoses were quantitatively evaluated and considered significant if the coronary diameter was reduced by ≥70%. Results – From 404 patients, 254 were men (63%) and the average age was 59.3 years ± 9 years. Hypertension was found in 80.7% (326 patients), diabetes in 23.2% (94 patients), 48.5% were smokers (196 patients), 82.1% had dyslipidemia (332 patients) and 30.7% were overweight (124 patients). A positive stress test was found in 285 patients and 186 had significant stenosis on coronarography. The rest of 119 patients had either a negative stress test, an equivocal one or inconclusive (the inability to reach 85% of the target heart rate, and without any ST segment alterations). At the coronary angiography we found significant lesions in 32 patients (26.9%) from the group with negative, equivocal or inconclusive stress testing. The sensitivity of the test was 85.3% and the specificity 46.8%.The positive predictive value was 65.3% and the negative predictive value was 73.1%. The amplitude of ST segment changes showed a correlation with the degree of stenosis. No correlation was found between the ECG teritory were ST depression appeared and the affected coronary artery, but ST elevation in lead aVR is an important indicator of significant left main coronary artery (LMCA) stenosis.The time of exercise (the exercise capacity) is correlated with the age of the patient. Conclusions – In modern era where imagistic stress testing seems to have a better sensitivity, the old fashioned electrocardiographic stress test continues to have a good sensitivity and remains, due to the larger accessibility and lower cost compared with other techniques (stress echography, stress SPECT, myocardial perfusion imaging) the first option in the diagnostic algorithm of coronary artery disease.
Keywords: exercise testing, risk factors, predictive value, significant coronary artery stenosis, exercise capacity.
Rezumat: Scopul – Testul ECG de efort reprezintă o metodă valoroasă şi larg folosită pentru diagnosticul bolii obstructive coronariene. Studiile anterioare din literatura de specialitate arătau o sensibilitate de 68% şi o specificitate de 77% pentru testul de efort, valoarea predictivă depinzând de probabilitatea pretest pentru boală coronariană. Scopul studiului este de a evalua valoarea diagnostică a testului de efort în epoca cardiologiei moderne. Metoda – Am efectuat un studiu retrospectiv pe 404 pacienţi care prezentau durere toracică sugestivă pentru angină, fără boală coronariană ischemică cunoscută, care au efectuat un test de efort pe covor rulant în laboratorul nostru şi apoi control coronarografic, în perioada octombrie 2008-ianuarie 2013. Coronarografia a fost realizată într-un interval cuprins între 2 şi 60 de zile după test. Testul a fost interpretat ca pozitiv dacă a apărut subdenivelare de segment ST de minim 0,1 mV (1 mm) de tip orizontal sau descendent sau subdenivelare de tip lent ascendent ≥1,5 mm sau supradenivelare de segment ST de minim 0,1 mm. Stenoza coronariană a fost interpretată ca semnificativă la o reducere a lumenului ≥70%. Rezultate – Între cei 404 pacienţi, 254 erau bărbaţi (63%), iar vârsta medie a grupului a fost de 59,3 ani ± 9 ani. Ca factori de risc, 80,7% (326 de pacienţi) aveau hipertensiune, 23,2% (94 pacienţi) erau diabetici, 48,5% (196 de pacienţi) erau fumători, 82,1% (332 pacienţi) aveau valori mari ale colesterolului seric, iar 30,7% erau supraponderali. Testul a fost pozitiv la 285 de pacienţi iar o stenoză semnificativă a apărut în 186 de cazuri. Restul de 119 pacienţi au avut fie un test negativ, fie un test interpretat ca echivoc (modificări ale segmentului ST sub limita pragului ischemic stabilit) sau neconcludent (nu a realizat un test submaximal, adică 85% din valoarea maximă predictivă pentru vârstă). Sensibilitatea testului a fost de 85,3%, iar specificitatea de 46,8%. Valoarea predictivă pozitivă a fost de 65,3%, iar cea negativă de 73,1%. Amplitudinea modificarilor ST s-a corelat cu gradul stenozei. Nu a putut fi stabilită o corelaţie între teritoriul în care au apărut modificările pe ECG şi artera coronară implicată, exceptând supradenivelarea segmentului ST în aVR care reprezintă un indicator pentru stenoza de trunchi comun. Timpul de efort (capacitatea de efort) este corelat cu vârsta. Concluzii – În epoca cardiologiei moderne, când sunt disponibile alte investigaţii noninvazive cu sensibilitate superioară (ecografia de efort, perfuzia miocardică de stress), testul de efort continuă să arate o bună sensibilitate şi rămâne, datorită costului redus şi accesibilităţii, prima opţiune în algoritmul de diagnostic al bolii coronariene.
Cuvinte cheie: test de efort, factori de risc, valoare predictivă, stenoză coronariană semnificativă, capacitate de efort.
Introduction
Cardiovascular disease (CVD) remains the global main cause of death, accounting for 17.3 million deaths per year and continues to cause a much greater mortality burden among Europeans than any other disease: 51% of deaths among women and 42% among men in the last year of reported data1. Coronary heart disease only, accounts for almost 1.8 milion deaths, or 20% of all deaths in Europe annualy, but the patterns vary widely in individual countries2. In our country, age-standardized mortality is still high, despite a decrease of mortality rate in the last 10 years with 16% in men and 22% in women2.
Chest pain is the most common presenting complaint indicating CAD and is seen frequently by primary care physicians or cardiologists.
The exercise treadmill test is used in the evaluation of symptomatic patients to predict the presence and extent of coronary artery disease (CAD). A large number of noninvasive stress testing are currently available, but the exercise ECG is still used as a standard for comparison with other clinical and testing risk markers. It is also the least costly of all provocative noninvasive tests, do not always require a cardiologist, and are convenient for the patient because are often an office-based investigation. The ECG exercise test (ET) for the diagnosis of obstructive CAD has a class I indication (class I: conditions for which there is evidence and/or general agreement that a given procedure or treatment is useful and efective) in the subgroup of adults with an intermediate pretest probability of CAD on the basis of gender, age, and symptoms3.
The studies evaluating the diagnostic accuracy of the ET have proved a mean sensitivity of 68% and a mean test specificity of 77%, with sensitivities ranging from 23% to 100% and specificities ranging from 17% to 100%, but the large proportions of studies and meta-analysis was published about 20 or 30 years ago4. The prevalence of CAD was changing and also, over the past two decades the frecquency and severity of abnormal stress testing have progressively decreased5. In the modern era of cardiology, to analyse the sensitivity and specificity of ECG exercise testing could be a challenge.
In our knowledge, there are no available data regardind the sensitivity or specificity of ET nowdays in our country.
Study group
This is a retrospective study of 404 patients, which were referred for exercise testing in our Institute between October 2008 to January 2013, according to the following inclusion criteria: 1) chest pain suggestive for angina; 2) no history or electrocardiographic evidence of previous myocardial infarction; 3) no left bundle branch block, WPW syndrome, ECG criteria for left ventricular hypertrophy (LVH) or valvular disease which can influence the interpretation of ST segment deviation or left ventricular function; 4) absence of clinical indication for urgent coronary revascularization.
Clinical informations and risk factors evaluation were obtained before testing. Exercise testing was performed in the morning and after withdrawal, where was the case, of antianginal therapy for at least 72 hours, on the treadmill (Burdick, USA) using the classical Bruce protocol under supervision of the in charge cardiologist; recording of the ECG was done with the Mason-Likar torso-mounted limb system, ankle and wrist electrodes being replaced by electrodes mounted on the torso at the base of the limbs. The patients were encouraged not to tighly grasp the front or side rails of the treadmill and to exercise to their maximum. The test was symptom limited and was terminated when any of the following occurred: severe angina, dyspnoea, fatigue, hypotension, complex ventricular arrhythmia and >1 mm ST segment depression. Sub-maximal predicted heart rate was calculated as 75% of maximal predicted heart rate (ie 220-age). The ECG was recorded with a Siemens Megacart electrocardiograph on each stage, prior peak exercise and in the recovery period, at each minute. A paper spead of 25 mm/s was used an 1 vertical mm equals 0,1 mV. The ECG was read by measuring the ST segment deviation from the PQ (PR) segment at 0,08 sec. from the J point. A positive test was defined as horizontal or downsloping ST segment depression or elevation of 0,1 mV (1 mm) or slowly upsloping of 1.5 mm, slowly being defined as <1 mv/sec. Equivocal test was defined as not meeting the positive test criteria but showing concerning change (eg, minimal ST depression not reached 0,1 mV, symptoms of chest pain without ECG changes). Inconclusive tests, the inability to achieve 85% of the maximal predictive heart rate, were assimilated with the equivocal tests. ST deviation was interpreted by the treadmill computer system, with confirmation or regulation by the supervising physician (cardiologist with great experience in ET). All the ET data were abstracted from the standard ET template routinely used in our system.
Systolic blood pressure was measured with a mercury sphygmomanometer in the final minut of each stage, at peak exercise and immediately after stoping exercise and every minut in the recovery phase. Exercise capacity was estimated from the time of exercise.
Selective coronary angiography was performed between 2 days and 60 days after the test, the decision to referre the patient for invasive evaluation had belonged to the attending cardiologist. Coronary artery stenoses were quantitatively evaluated and considered significant if the coronary diameter was reduced by ≥70%. Data collected on each patient included age; sex; risk factors for CAD; exercise time; the maximum amplitude of ST segment deviation (mm); the ECG leads with ST deviation which were grouped in five teritories: I, aVL, V4-V6; V3-V5; II, III, aVF; aVR, V1; V4-V6; the degree of stenoses for left anterior descending artery and the septal and diagonal branches (LAD), left circumflex artery and his marginal branches (Cx), right coronary artery (RCA) and left main coronary artery (LM).
Statistical analysis
Descriptive statistics were used to characterize the study population with respect to demographics, cardiac risk factors and ET results. We then evaluated the relationship between ET results and documented extend of CAD in coronary angiography by calculating sensitivity, specificity, predictive positive value (PPV), negative predictive value (NPV) using standard formulas from 2×2 table. The analysis was performed using SPSS 21.0 (Statistical Package for Social Science version 21, SPSS, Inc, USA). The Spearman correlation coefficient was used to determine bivariate non-parametrics correlations. A probability error of 5% was established for every analysis, the value of p<0.05 being considered statistically significant.
Results
Patient demographics of the 404 patients are presented in Table 1. Sixty-three percent were men and 37% were women. The age range from 28 to 83 years with a mean age of 60 years ± 9 (mean ± standard deviation), the same mean value for men, as for the women. The study population has a significant number of cardiac risk factors, as noted in Table 1. Hypertension was present in 326 patients (80.7%),and dyslipidemia in 82.2% (332 patients); 196 patients had declared to be active smokers (48.5%), 124 patients (30.7%) were overweight persons, and the diabetes was found in 94 cases (23.3%). 37,6% of patients had 2 risc factors and 36.6% presented the association of three risk factors.
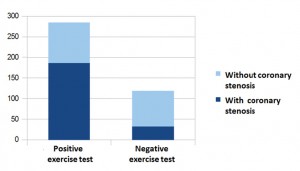
There were a total of 285 positive tests and 119 negative tests, which includes also the equivocal tests. A significant coronary artery stenosis was present in 186 patients with positive stress testing and in 32 patients with negative stress testing, as shown in Figure 1. The ST segment depression was recorded simultaneously in leads I, aVL, V4-V6 in 50 patients, in leads V3-V5 in 136 patients, in inferior leads II, III and aVF in 201 patients (50% of total patients), in V4-V6 in 185 patients. ST segment elevation in aVR and V1 was recorded in 65 patients. The ST deviation was recorded in two ECG territories in 122 patients (30.2%).
Table 1. Characteristic of the Exercise Stress
| Testing Study Population | |
| Age (years) | |
| Mean | 59.3 |
| SD | +/- 9 |
| Sex (%) | |
| Men | 63 |
| Women | 37 |
| Risk Factors (%[n]) | |
| Hypertension | 80.7 (326) |
| Hypercholesterolemia | 82.1 (332) |
| Diabetes Mellitus | 23.2 (94) |
| Current smoker | 48.5 (196) |
| Obesity | 30.7 (124) |
| Association of Risk Factors (%[n]) | |
| No risk factors | 1.5 (6) |
| One risk factor | 6.7 (27) |
| Two risk factors | 37.6 (152) |
| Three risk factor | 36.6 (148) |
| Four risk factors | 14.6 (59) |
| All five risk factors | 3 (12) |
The sensitivity of the test was 85.3%, the specificity 46,8 %, the positive predictive value was 65.3%, and the negative predictive value was 73.1%. Both sensitivity and specificity were similar in men and women (0.87 and 0.46 for men, respectively 0.78 and 0.47 for women). The PPV was greater for the men (0.75 vs 0.44 in women), but NPV was greater for the women (0.8 vs 0.66 for men), which corresponding with the higher prevalence of CAD in men compared with women in the same aging group. Most patients (29%) had only one coronary artery with stenosis; the sensitivity of the ET for the one-vessel disease was 74.5%, and specificity was 50%. If the equivocal test would be included in the positive tests, the sensitivity of the test would be 94.5%, with a decrease in specificity (31.2%); PPV would be 61.7%, and NPV 82.9%. We found, also, a high sensitivity (91.5%) and a low specificity (37%) when we made the calculation without take into account the equivocal tests, comparing only positive with pure negative tests.
For a better comparison between the results of ET and coronary arteries involvement, we have divided the study population in four groups: 1) patients with positive ET and significant coronary lesions – true positive tests (186 patients); 2) patients with positive ET and without significant coronary artery stenosis – false positive tests (99 patients); 3) patients with negative or equivocal ET and without coronary stenoses – true negative tests (87 patients); 4) patients with negative ET and significant coronary stenosis – false negative tests (32 pacients). The characteristics of the four groups are presented in Table 3.
A pure negative ET (equivocal test not included) was recorded in 65.5% (57 patients) with no coronary artery stenoses and only in 13 patients (40%) in whom the CAD was present. In 32 patients with significant stenosis the ET was not positive. In these patients, the majority (25 patients) had one vessel disease (any coronary artery), one patient had three vessels disease and one patient had significant stenosis of left main artery, but also of LAD and Cx.
The ECG teritory with ST deviations (anterior, inferior, antero-septal, lateral) is not specific for one or other of the coronary artery, except the ST depression in V3-V5 or ST elevation in aVR, V1 where odds ratio (OD) for the LM is statistically significant, as shown in Table 2.
Table 2. The distribution on ECG territories compared with the involved coronary artery
| No (%) | OR | 95% Confidence Interval | |||
| I, aVL,V4-V6 | LAD | 33 (66%) | 3.556 | 1.905 | 6.640 |
| Cx | 27 (54%) | 3.603 | 1.964 | 6.607 | |
| RC | 26 (52%) | 2.676 | 1.468 | 4.880 | |
| LM | 7 (14%) | 2.343 | 0.949 | 5.784 | |
| V3-V5 | LAD | 54 (39.7%) | 1.038 | .681 | 1.584 |
| Cx | 38 (27.9%) | 0.980 | .619 | 1.550 | |
| RC | 42 (30.9%) | 0.946 | .606 | 1.476 | |
| LM | 12 (8,8% | 1.344 | .628 | 2.878 | |
| II, III, aVF | LAD | 98 (48.8%) | 2.268 | 1.506 | 3.414 |
| Cx | 79 (39.3%) | 3.108 | 1.960 | 4.930 | |
| RC | 95 (47.3%) | 4.617 | 2.902 | 7.346 | |
| LM | 21 (10.4%) | 2.515 | 1.122 | 5.635 | |
| aVR, V1 | LAD | 41 (63.1%) | 3.241 | 1.868 | 5.625 |
| Cx | 36 (55.4%) | 4.154 | 2.395 | 7.204 | |
| RC | 34 (52.3%) | 2.859 | 1.663 | 4.914 | |
| LM | 18 (27.7%) | 10.436 | 4.728 | 23.037 | |
| V4-V6 | LAD | 89 (48.1%) | 2.015 | 1.344 | 3.023 |
| Cx | 74 (40%) | 2.983 | 1.899 | 4.687 | |
| RC | 83 (44.9%) | 3.146 | 2.032 | 4.873 | |
| LM | 16 (8.6%) | 1.386 | .658 | 2.922 | |
| No=number of cases with coronary arteries stenoses; OR = odds ratio | |||||
Table 3. Characteristics of The Exercise Testing Groups According with the Positivity of the Test and Presence of Significant Coronary Arteries Stenoses
| Positive test, signifiant stenoses | Positive test, no signifiant stenoses | Negative test, no signifiant stenoses | Negative test, signifiant stenoses | ||
| No. of patients | 186 | 99 | 87 | 32 | |
| Mean age (years) | 60.2 | 59.8 | 56.3 | 61 | |
| Women (no, [%]) | 41 (22%) | 52 (52%) | 46 (53) | 11 (34%) | |
| Risk factors | 1 | 15 (17%) | |||
| 2 | 64 (33.4%) | 44 (44.4%) | 30 (34.5%) | 14 (43.7%) | |
| 3 | 78 (41.9%) | 34 (34.3%) | 28 (32%) | 8 (25%) | |
| 4 | 32 (17.2%) | 11 (11.1%) | 7 (8%) | 8 (25%) | |
| Mean exercise time (min) | 6.2 | 6.68 | 7.15 | 6.24 | |
| Mean ST segment deviation (mm) | 1.65 | 1.28 | – | – | |
The most significant stenoses were found in patients in whom the ST segment alteration in lateral leads V4-V6 or aVR and V1 have been revealed. In Figure 2 we have presented the exercise electrocardiogram of a patient with severe stenosis located at the ostium of LAD, with ST depression in multiple leads, but also with ST elevation in aVR.
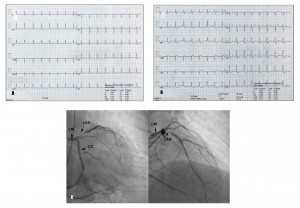
Figure 2. A. Rest Electrocardiogram(ECG) – normal; B. The positive exercise test: ST depression in leads II, III, aVF, V3-V6 and ST segment elevation in aVR; C. The coronary arteriography: suboclusion located at the ostium of LAD. ( LM – left main coronary artery, LAD – left anterior descending, CX – left circumflex artery).
When we analysed the correlation between the number of risk factors for CAD and the number of involved coronary arteries, an correlation Spearman coefficient of 0.210 was positive, indicating a positive relation, but the power of this indicator is weak. More risk factors we have, more coronary artery with stenosis will be found (p<0.05). For each unit increase in number of risk factors, the number of affected coronary arteries will increase with 0.245; eg, the predictor number of stenotic coronary arteries will be 1.8 in a patient with all five risk factors.
The exercise capacity, expressed as exercise time on treadmill is not correlated with the number or the degree of coronary artery stenosis. The age of the patient was the only factor which we could find to significant influence the exercise capacity.
The amplitude of ST modification was correlated with the severity of coronary artery stenosis.
Hypertension was the risk factor we have found in 325 patients. In this subgroup of patients, the ST segment alterations was recorded predominantely in the lateral precordial leads V4-V6. The exercise time was almost one minut better (52 sec) in hypertensive patients with a stenosis <70% or without stenosis, compared with the hypertensive patients with significant stenosis, which is statistically significant (p<0.0001). The same correlation was found when we analised the exercise capacity and the results of ET. The hypertensive patients with positive ET had a lower exercise capacity (difference of 54 sec) when the stenosis is <70% compared with hypertensive patients with positive ET and stenosis >70% (346 sec vs 400 sec), as shown in Table 5.
Discussion
Exercise testing remains the most widely accessible and relatively inexpensive method for initial evaluation of suspected coronary artery disease6. Prediction of the disease is one of the primary functions of stress testing and any clinician would like to be able to predict in each patient the anatomic and functional coronary disease severity, which influence the ultimate outcome of the patient7. Bayes’s theorem states that the predictive value of a positive test is directly related to the prevalence of disease in the population being studied3,7. There are a number of ways to estimate disease prevalence, and therefor is a disagreement in this field. Also, there are diferences between prevalence of CAD in diferent areas of cardiology practice; would be a larger percentage of patients with CAD in a tertiary center with experts in the field than in the office of GP, for example. The sensitivity of the ET is not very good compared with other noninvasive methods such as the various exercise imaging studies which provide greater diagnostic accuracy than electrocardiograhic test alone.
ECG for the detection of CAD revealed a mean test sensitivity of 68% and a mean test specificity of 77%8, but the data were recorded almost three decades ago, even they are mentioned in recent papers and scientific statements for clinical practice4.
We found a high sensitivity (85.3%), a specificity of 46,7% and NPV of 73,1% in our study, which is comparable with much expensive tests used to diagnose the presence of coronary artery disease. For example, the exercise stress echocardiography has a sensitivity of 80-85%, and a specificity of 80-88%; the exercise stress SPECT (single photon emission computed tomography) has a sensitivity of 73-92%, and a specificity of 63-87%9. We didn’t have collected data about pretest probability and usually, the pretest probability is formally estimated, based on symptomatology, age and sex, as noted in the ACC/AHA Guideline for stess testing3 (Table 4). We can presume that a large number of patients has an intermediate to high pretest probability, being selected by general practician (GP) and attending cardiologist, but was the same ET laboratory status as shown in previous studies. Certainly, the study has a referral bias (RB) which occurs when patients with an abnormal stress test result are referred to cardiac catheterization at a higher rate than those with a normal stress result, but usually RB is not accounted for when analysing the sensitivity and specificity of stress test.
Table 4. Pretest Probability of Coronary Artery Disease by Age, Gender, and Symptoms
| Age (years) | Gender | Typical Angina | Atypical Angina | Nonanginal chest pain | Asymptomatic |
| 30-39 | Men | Intermediate | Intermediate | Low | Very low |
| Women | Intermediate | Very low | Very low | Very low | |
| 40-49 | Men | High | Intermediate | Intermediate | Low |
| Women | Intermediate | Low | Very low | Very low | |
| 50-59 | Men | High | Intermediate | Intermediate | Low |
| Women | Intermediate | Intermediate | Low | Very low | |
| 60-69 | Men | High | Intermediate | Intermediate | Low |
| Women | High | Intermediate | Intermediate | Low | |
| Modified from refs.3 High indicates > 90%; intermediate, 10% – 90%; low, <10%; very low, <5%. Intermediate pretest probability is an ACC/AHA Class I indication for exercise testing. |
|||||
Table 5. Exercise Capacity and the Severity of Stenosis in Hypertensive Patients
| Group Statistics | |||||
| Coronary stenosis | No | Mean | Std. Deviation | Std. Error Mean | |
|
Exercise Time (sec) |
>70 % | 118 | 348.3136 | 109.17708 | 10.05057 |
| <70% | 102 | 400.4216 | 79.60029 | 7.88160 | |
Despite the fact known from old studies that ST depression is less likely to be associated with CAD in women10,11, we found a high sensitivity for ET in women too (0.78%). The PPV was 0.44% (compared with 0.75 in men), but the NPV is superior in women (0.8 vs 0.66 in men). The difference could be explained by the diferences in the prevalence of CAD in women vs men12.
As we expected, we didn’t find a correlation between the ECG leads with ST changes and the coronary artery involved. When LAD disease was found, in 66% of cases the ST depression had occurred in anterior leads I, aVl, V4-V6, but for the same disease we found ECG changes also in V3-V5 in 40% of cases, only in V4-V6 in 48%, and the same prevalence in inferior leads (48% of cases). In many cases we had concomitant ST changes in more then one territory. The ecg changes was occurred in one territory in 23% of cases. But the amplitude of ST depression was correlated with the degree of stenosis: more tight stenosis we had, more depth ST modification.
A challenging issue in the literature was the predictive value of ST elevation in lead aVR in the setting of exercise testing. Prior studies have demonstrated the value of ST changing in aVR in acute coronary syndromes where the ST elevation may indicate severe stenosis or occlusion of the left main coronary artery13-15. In the setting of ET only few studies16-18 raised the importance of ST elevation in aVR as an important indicator for significant LM stenosis or ostial LAD stenosis. In our study, the ST changes in aVR and V1 were statistically significant marker for the LM stenosis.
We found hypertension in 80.7% of cases, which is the double of the prevalence found in the SEPHAR II study, where the prevalence of hypertension was 40.1%19. Exercise responses regarding exercise BP, exercise capacity, ST changes in hypertensive patients are correlated with the risk of CV disease and CV death20,21.
In our study, the hypertensive patients developed ST segment depression predominantely in the lateral precordial leads V4-V6, a fact which was revealed also in other ET studies22, and had a lower exercise capacity (they didn’t reach the stage III of the Bruce protocol) if a significant coronary artery stenosis occurred.
We note also that the exercise testing is a safe procedure. There were no serious complications in this study, even in the patients with severe CAD.
Conclusions. In the modern era with dynamic changes in the prevalence, impact and treatment of cardiovascular risk factors and changes in the prevalence of CAD and CVD mortality, the predictive value of ECG stress testing is not very well established. We have demonstrated that in a specialised cardiological center, with a high expertise in ET, the sensitivity of the exercise testing for CAD is also high, both in men and women, comparable or even superior with other imaging exercise techniques; exercise testing continue to be first option in the diagnostic algorithm of coronary artery disease and with a good price/quality ratio.
Conflic of interest: The authors declare that they don’t have any conflict of interest.
Author’s contributions: All authors have contributed to the manuscript and approved the final version.
References
1. Smith SC, Collins A, Ferrari R, Holmes DR, Logstrup S, Vaca D, Ralston J, Sacco R, Stam H, Taubert K, Wood D, Zoghbi W.Our time:a call to save preventable death from cardiovascular disease. J Am Coll Cardiol.2012;60:2343-2348.
2. Nichols M, Townsend N, Scarborough P, Rayner M. Cardiovascular disease in Europe 2014:epidemiological update. Eur Heart J. 2014;35: 2950-2959
3. Gibbons RJ, Balady G, Bricker JT, Chaitman BR, Fletcher GF, Froelicher VF, Mark DB, McCallister BD, Mooss AN, O’Reilly MG, Winters WL. ACC/AHA 2002 Guideline Update for Exercise Testing.A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Exercise Testing). 2002. American College of Cardiology Web site. Available at :www.acc.org/clinical/guidelines/exercise/dirIndex.htm
4. Fletcher G, Ades P, Kligfield P, Arena R, Balady GJ, Bittner VA, Coke LA, Jerome FL, Forman DE, Gerber TC, Gulati M, Madan K, Rhodes J, Thompson PD, Williams MA. Exercise standards for testing and training:a scientific statement from the American Heart Association. Circulation. 2013;128:873-934
5. Rozanski A, Gransar H, Hayes S, Min J, Friedman JD, Thomson LEJ, Berman DS. Temporal trends in the frequency of inducible myocardial ischemia during cardiac stress testing.1991 to 2009. J Am Coll Cardiol. 2013;61:1054-65
6. Kligfield P, Lauer M. Exercise electrocardiogram testing.Beyond the ST segment. Circulation 2006; 114:2070-2082.
7. Ellestad, M.H.Predictive implications. In Stress testing. Principles and Practice. Fifth Edition. Eds: Ellestad MH. Oxford University Press, 2003, p271-309.
8. Gianrossi R, Detrano R, Mulyhill D, LehmannK, Dubach P, Colombo A, McArthur D, Froelicher V. Exercise-induced ST depression in the diagnosis of coronary artery disease. A meta-analysis.Circulation.1989;80:87-98
9. Montalescot G, Sechtem U, Achenbach S, Andreotti F,Arden C, Budaj A, Bugiardini R, Crea F, Cuisset T, Di Mario C, Ferreira JR, Gersh BJ, Gitt AK, Hulot JS, Marx N, Opie LH, Pfisterer M, Prescott E, Ruschitzka F, Sabaté M, Senior R, Taggart DP, Van der Wall EE, Vrints CJM. 2013 ESC guidelines on the management of stable coronary artery disease. The Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. 2013;83:660-666.
10. Kwok Y,Kim C, Grady D, Segal M, Redberg R.Meta-analysis of exercise testing to detect coronary artery disease in women. Am J Cardiol. 1999;36:169-173
11. Wong YK, Dawkins S, Grimes R, Smith F, Dawkins KD, Simpson IA. Improving the positive predictive value of exercise testing in women. Heart 2003; 89: 1416-1421.
12. Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Hei JA, Howard VJ, Huffman MD, S Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Magid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler III ER, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NP, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS,. Wong ND, Woo D, Turner MB. Heart disease and stroke statistics-2014 update: a report from American Heart Association. Circulation 2014; 129: e28-e292
13. Barrabes JA, Figueras J, Moure C, Cortadellas J, Soler-Soler J. Prognostic value of lead aVR in patients with a first non-ST-segment elevation acute myocardial infarction. Circulation. 2003; 108:814-819.
14. Chioncel O, Carp A, Şelaru A, Deleanu D, Zarma L, Macarie C. Valoarea predictivă pozitivă a modificărilor ECG pentru anatomia coronariană: corelaţie factori de risc, clinică, ECG, leziuni coronariene (in Romanian). Revista Română de Cardiologie 1999;2:56-63
15. Szymanski FM, Grabowski M, Filipiak KJ, Karpinski G, Opolski G. Admission ST-segment elevation in lead aVR as the factor improving complex risk stratification in acute coronary syndromes. Am J Emerg Med. 2008;26:408-412
16. Uthamalingam S, Zheng H, Leavitt BA, Pomerantsev E,Ahmado I, Gurm G, Gewirtz H. Exercise-induced ST-segment elevation in Ecg lead aVR is a usefull indicator of significant left main or ostial LAD coronary artery stenosis. J Am Coll Cardiol Img. 2011; 4:176-86)
17. Egher L, GherasimD, C.Cosmin, Ginghină C. ECG stress test in… left main stenosis. Rom J Cardiol. 2012: 22(4):324-325.
18. Rugină M, Molfea V, Deleanu D, Iliescu VA, Bubenek-Turconi S, Gherasim D, Predescu L, Dorobanţu L, Ştiru O, Făţoi D, Coman IM. Chronic proximal coronary occlusion in an oligosymptomatic diabetic patient-medical and surgical therapy. Rom J Cardiol. 2011;21(3): 261-265
19. Dorobanţu M, Bartoş D, Apetrei E, Arsenescu-Georgescu C, Pop D, Ghiorghe S, Tănăsescu R, Craiu E, maniţiu I, Tăutu O. Hypertension in Romania: where we are and what can be done ? Results from SEPHAR II study. Rom J Cardiol. 2012;22(4):177-184)
20. Mundal R, Kjeldsen SE, Sandvik L, Erikssen G, Thaulow E, Erikssen J. Exercise blood pressure predicts cardiovascular mortality in middle-aged men.Hypertension1994:24:56-62
21. Kokkinos P, Manolis A, Pittaras A, Doumas M, Giannelou A, Panagiotakos DB, Faselis C, NarayanP, Singh S, Myers J. Exercise capacity and mortality in hypertensive men with and without additional risk factors. Hypertension 2009; 53:494-499.
22. Michaelides AP, Liakos CI, Raftopoulos LG, Antoniades C, Vyssoulis G, Andrikopoulos G, Ioakeimides N, Tsioufis C, Soulis D, Stefanadis C. Electrocardiographic criteria for detecting coronary artery disease in hypertensive patients with ST-segment changes during exercise testing. J Electrocardiol. 2009;42:405-409.
 This work is licensed under a
This work is licensed under a