C. Matei1,2, Ioana Pop3, Mihaela Badea4, Adriana Saraolu1, I. M. Coman1,2, E. Apetrei1,2
Article received on May 21st 2012. Article accepted on May 31st 2012.
1 ”Prof. Dr. C.C. Iliescu” Emergency Institute for Cardiovascular Diseases, Bucharest
2 “Carol Davila” University of Medicine and Pharmacy, Bucharest
3 CLINICCO, Braşov
4 HUMANITAS Clinic, Bucharest
Dr. Costel Matei, ”Prof. Dr. C.C. Iliescu” Emergency Institute for Cardiovascular Diseases, Bucharest, Cardiology Department, 258 Fundeni Street, 022328, Bucharest, Romania
E-mail: cmatei2002@yahoo.co.uk
Abstract: Supraventricular arrhythmias are common in patients with dilated cardiomyopathy. Among them, atrial fibrillation (AF) plays an important role, especially in terms of negative hemodynamic consequences and embolic risk. Aim – To identify predictive factors of AF presence in patients with dilated cardiomyopathy and to quantify their predictive power. Secondary, these factors have been pursued with the overall risk of death and how the presence of AF influences the long term evolution of these patients. Materials and methods – The retrospective study included 348 patients diagnosed with dilated cardiomyopathy, in sinus rhythm, divided according to etiology in subgroup A – non-ischemic etiology – and subgroup B – ischemic etiology –. Patients were followed clinically, ECG, echocardiography for a mean of 60.1 months (4-126 months). Statistical analysis was performed using EpiInfo 6.0, EpiInfo 3.5.1 (CDC Atlanta, USA) and MedCalc 12.2.1.0 (Medcalc Software BVBA, Belgium). Results – During follow-up, AF was identified in subgroup A and subgroup B as paroxystic AF in 7% and 5% respectively, and permanent AF in 12% and 10% respectively of patients. Univariate and multivariate analysis (Cox) showed a good prediction of paroxysmal AF for 2 parameters in univariate analysis: left ventricular end diastolic diameter (HR = 2.7, p <0.05) and presence of mitral regurgitation (HR = 2.7, p <0.05); predictive power was better for grade 3 mitral regurgitation (HR = 3.78, p <0.05). In multivariate analysis, only the presence of grade 3 mitral regurgitation maintains its prediction power. Best predictors of permanent AF were NYHA functional class at baseline (HR = 1.74, p <0.05), LA diameter (HR = 7.96, p <0.005), presence of mitral regurgitation (HR = 2.14, p <0.05), also the predictive power was better for grade 3 mitral regurgitation (HR = 2.47, p <0.05). None of these parameters reach statistical significance in multivariate analysis. NYHA functional class >3, LV ejection fraction >35%, presence of mitral regurgitation greater than grade 2 or systolic pulmonary artery pressure >60mmHg had high specificity (70%, statistically significant only for the presence of any type of fibrillation), while QRS duration ≤110ms, LV end-diastolic diameter >63mm, LV end-systolic diameter >47mm, LA diameter >41mm had high sensitivity (over 70%, statistically significant only for LA diameter in relation to installation of permanent AF). Conclusions – This study identified as predictive factors of paroxysmal AF ventricular end diastolic diameter >63mm and presence of mitral regurgitation, while permanent AF was associated with heart failure NYHA class, LA diameter and presence of mitral regurgitation. With a high enough prevalence, AF is a condition that can contribute to lower quality of life and heart failure worsening. Overall mortality, on the other hand, was not significantly influenced by the presence of AF.
Keywords: atrial fibrillation, dilated cardiomyopathy, heart failure
Rezumat: Tulburările de ritm supraventriculare sunt frecvent întâlnite la pacienţii cu cardiomiopatie dilatativă. Între acestea, fibrilaţia atrială (AF) joacă un rol important, mai ales prin prisma consecinţelor hemodinamice negative şi a riscului embolic. Scopul lucrării – Identificarea factorilor de predicţie privind apariţia AF la pacienţii cu cardiomiopatie dilatativă şi cuantificarea puterii de predicţie a acestora. Secundar au fost urmărite corelarea acestor factori cu riscul global de mortalitate şi modul în care prezenţa AF influenţează evoluţia pe termen lung a acestor pacienţi. Material şi metodă – Studiul retrospectiv a inclus 348 de pacienţi diagnosticaţi cu cardiomiopatie dilatativă, în ritm sinusal, împărţiţi în funcţie de etiologie în lotul A – etiologie non-ischemică – şi lotul B – etiologie ischemică –. Pacienţii au fost urmăriţi clinic, ECG, ecocardiografic pe o perioadă medie de 60,1 luni (4–126 luni). Analiza statistică s-a făcut cu EpiInfo 6.0 şi EpiInfo 3.5.1 (CDC Atlanta, SUA) şi MedCalc 12.2.1.0 (Medcalc Software BVBA, Belgia). Rezultate – Pe perioada urmăririi, AF a fost identificată în lotul A şi în lotul B sub formă de AF paroxistică la 7%, respectiv 5%, iar ca AF permanentă la 12%, respectiv 10%, din pacienţi. Analiza univariată şi multivariată (Cox) a arătat o predicţie bună pentru apariţia AF paroxistice a 2 parametri în analiza univariată: diametrul telediastolic al ventriculului stâng (HR= 2,7, p<0,05) şi prezenţa regurgitării mitrale (HR= 2,7, p<0,05); puterea de predicţie a fost mai bună în cazul regurgitării grad 3 (HR= 3,78, p<0,05). În analiza multivariată, numai prezenţa regurgitării mitrale grad 3 îşi menţine puterea de predicţie. Pentru apariţia AF permanente predictori buni s-au dovedit clasa funcţională NYHA la includere (HR= 1,74, p<0,05), diametrul AS (HR= 7,96, p<0,005), dar şi prezenţa regurgitării mitrale (HR= 2,14, p<0,05); de asemenea, puterea de predicţie a fost mai bună în cazul regurgitării grad 3 (HR= 2,47, p<0,05). Nici unul dintre aceşti parametri nu au atins semnificaţia statistică în analiză multivariată. Clasa funcţională NYHA>3, fracţia de ejecţie VS >35%, prezenţa regurgitării mitrale mai mare de gradul 2 sau presiunea sistolică în artera pulmonară >60mmHg au avut specificitate mare (peste 70%, semnificativ statistic doar pentru prezenţa oricărui tip de AF), în timp ce durata QRS ≤110ms, diametrul telediastolic VS> 63mm, diametrul telesistolic VS> 47mm, diametrul AS> 41 mm au avut sensibilitate crescută (peste 70%, semnificativă statistic doar pentru diametrul AS în relaţie cu instalareaA F permanente). Concluzii – Studiul a identificat ca factori de predicţie în apariţia AF paroxistice un diametru telediastolic VS >63mm şi prezenţa regurgitării mitrale, în timp ce apariţia AF permanente s-a corelat cu clasa de insuficienţă cardiacă, diametrul AS şi prezenţa regurgitării mitrale. AF reprezintă una din condiţiile ce pot contribui la scăderea calităţii vieţii prin agravarea fenomenelor de insuficienţă cardiacă. Mortalitatea globală, pe de altă parte, nu a fost semnificativ influenţată de prezenţa AF.
Cuvinte-cheie: fibrilaţie atrială, cardiomiopatie dilatativă, insuficienţă cardiacă
Introduction
Idiopathic dilated cardiomyopathy (DCM) is a myocardial disease characterized by the dilatation of the left ventricle or biventricular dilatation, combined with the decrease of myocardial contractility in the absence of abnormal filling conditions (valve diseases, systemic arterial hypertension) or coronary heart disease to cause decrease of the global systolic function. In the past few years more evidences have been presented supporting the implication of an autoimmune process (both humoral and cellular) in the pathogenesis of dilated cardiomyopathy1. Most of the patients are diagnosed between the ages of 20 and 50 years, but the disease can also manifest in children and elders.
The most common first clinical manifestation of idiopathic dilated cardiomyopathy is heart failure (HF), which develops in 75-85% of the patients. Just certain categories of patients present arrhythmias with a high prevalence. They mark a negative prognostic, thus evoking the special importance of determining some prediction factors for the onset of such arrhythmias. The literature gives special attention to ventricular arrhythmias, which can lead to one of the two death mechanisms in DCM, sudden death. Less studied, supraventricular arrhythmias contribute to hemodynamic deterioration, frequently modifying the functional status and the patient quality of life.
Among supraventricular arrhythmias, atrial fibrillation (AF) is the most common in dilated cardiomyopathy associated with heart failure. Loss of the atrial contraction contribution to ventricular filling, rapid ventricular rate and the increased risk of embolism are just some of the negative effects of atrial fibrillation onset in patients with DCM.
The prevalence of atrial fibrillation in DCM increases proportionally with heart failure class as defined by the New York Heart Association (NYHA). The risk of AF increases as the global ejection fraction (EF) decreases. Thus, the presence of congestive heart failure is one of the most important independent predictive factors for AF, with a 6-fold increase of the relative risk. On the other hand, atrial fibrillation can significantly aggravate congestive heart failure symptoms in patients who were in a compensated stage of the disease when AF occurred, being one of the most important causes for decompensated heart failure.
It is also known that patients having AF with high ventricular rate can develop ventricular dilatation and decrease of the systolic function (the so-called tachyarrhythmic cardiomyopathy), so it is sometimes difficult to establish whether the atrial fibrillation occurred in the evolution of the DCM, or it is one of its causes. Even patients with recurrent AF episodes can develop in time such tachy-cardiomyopathies, which can disappear once the arrhythmia has been eliminated. R-to-R interval irregularity can also participate in the development of ventricular dysfunction2.
Finding some prediction factors for the onset of AF in patients diagnosed with DCM can be useful to improve the prognosis, generally reserved, of these patients.
Objectives
The main objective of the study was to identify some predictors for the onset of AF in patients with DCM and quantify their predictive power. As secondary objectives we correlate these factors with the overall risk mortality and the relationship between presence of AF and the long term evolution of these patients.
Materials and methods
The patients included in our study were selected from the electronic database of the “Prof. Dr. C.C. Iliescu” Emergency Institute for Cardiovascular Diseases, Bucharest between January 2003 and December 2007 using search criteria “dilated cardiomyopathy” as discharge diagnosis. From the 562 patients found, only patients in sinus rhythm and without pacemaker implantation at the time of the diagnosis, or at the first evaluation, were selected for our study. Three hundred forty-eight patients (85.6% men, 14.4% women) with ages between 18 and 83 (mean age 54.9±12.8) were identified in the database and formed the study group. Considering the etiology of DCM the patients were divided in subgroup A – 186 patients with non-ischemic DCM and subgroup B – 162 patients with ischemic DCM. The ischemic etiology was accepted based on the myocardial infarction history or on objective evidence of coronary artery disease (CAD) at angiography in patients with LV systolic dysfunction3,4. It is important to mention that in subgroup A the most frequent etiology was idiopathic cardiomyopathy (58%), followed by alcoholic cardiomyopathy (26%), whilst the remaining 16% were determined by other etiologies.
Data regarding clinical parameters (NYHA class, 6 minutes walking test), the presence of cardiovascular risk factors (arterial hypertension, diabetes, smoking, dyslipidemia), ECG parameters (QRS duration, presence of conduction abnormalities), 24h ambulatory ECG readings (the number, frequency and systematization degree of supraventricular events), echocardiography data (LV ejection fraction, LV and LA dimensions, presence of mitral and/or aortic regurgitation, the presence and degree of the LV diastolic dysfunction), as well as the treatment used (drugs classes) were recorded for the study group patients at inclusion.
The patients were followed for a mean period of 60.1 months (4-126 months). Their final status and follow-up duration were decided by two factors: 1) hospital/ambulatory visit for clinical check-up or admission or 2) interrogation of the Romanian National Health Insurance House Integrated Information System (SIUI) available online at http://siui.casan.ro:82/Asigurati/ (for those who were not registered in the Institute electronic database for more than 12 months). For the last category of patients, it was decided that in case of death the date would be approximated at 3 months after their last presence in the Institute (thus obtaining information in 139 of the total 158 deaths). In case the patient was not dead, the follow-up period would be considered up to December 2011 (date of the last reported data before the SIUI interrogation). Data collection and the statistic analysis were made taking into account the confidentiality rules.
When available, the same data recorded at inclusion were captured at follow-up. The atrial fibrillation history (clinically documented and confirmed by a 12 leads ECG) was also noted. The patients were divided according to the European Society of Cardiology recommendations for the management of atrial fibrillation in two categories (paroxistical / permanent). “Persistent” atrial fibrillation could not be identified in the studied patients due to the lack of information about the length of the paroxistical episodes not converted to sinus rhythm during admission.
Statistical analysis was done using EpiInfo 6.0 and EpiInfo 3.5.1 (CDC, Atlanta, 2008) and MedCalc 12.2.1.0 (Medcalc Software BVBA, Belgium). Continuous variables are presented as mean +/- standard deviation and categorical variables are expressed in percentiles. The continuous variables were assessed with the Kolmogorov-Smirnov test for normal distribution. The non-paired t-test was used for the continuous variables between patients with and without atrial fibrillation. Squared Chi-test was used to compare the same patient’s categorical values. Univariate and multivariate analysis were performed using Cox proportional hazard regression. Receiver operator characteristics (ROC) curves were used to determine the predictive power of the studied parameters for the development of atrial fibrillation – sensitivity (St), specificity – (Sp), positive predictive value – (PPV) and negative predictive value – (NPV). The differences in survival in the selected categories were presented through the Kaplan – Meyer survival curves. A p value less then < 0.05 was considered statistically significant.
Results
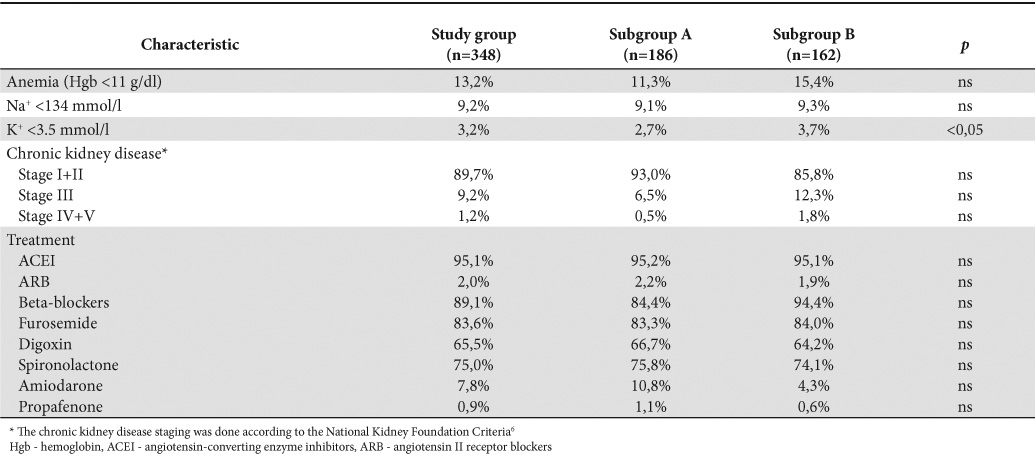
The main characteristics of study patients are presented in Table 1 (clinical data) and Table 2 (biological and treatment parameters). As expected, statistically significant differences of prevalence were registered for the CAD risk factors in the two subgroups, linked to the fact that patients having ischemic cardiomyopathy frequently have associated co-morbidities such as diabetes, arterial hypertension and dyslipidemia. We have noticed, in both subgroups of patients, high values for beta-blockers (95%), ACE inhibitors (90%) and spironolactone (75%) use. More surprising was the high number of patients receiving digitalis treatment (65%) as the study patients were in sinus rhythm at inclusion. A small number of patients were taking amiodarone with antiarrhythmic purposes, most frequently introduced for ventricular arrhythmias prophylaxis.
Table 1. Clinical characteristics of the patients
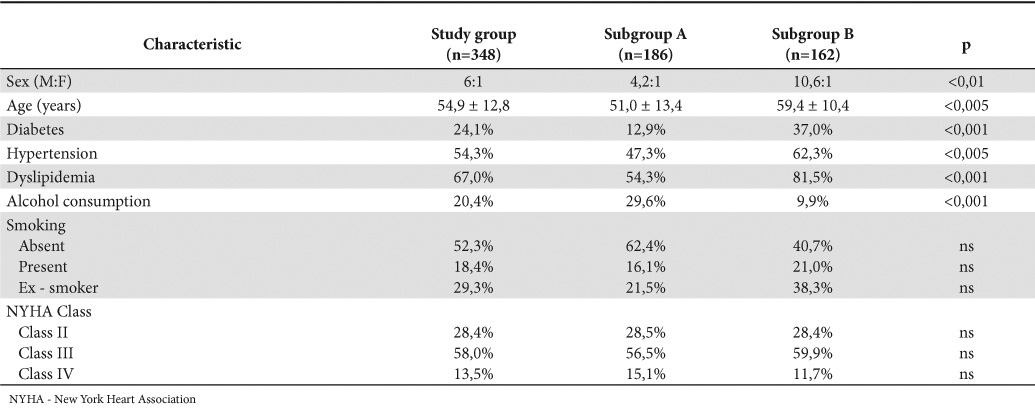
Table 2. Laboratory parameters and therapeutic classes used for treatment
The echocardiographic parameters significant to our study were synthesized in Table 3 (expressed in percentiles in the study group) and Table 4 (mean values and standard deviation).
Clinically documented AF episodes, confirmed by 12 leads ECG, occurred during the follow-up period in 59 patients (16.9%), 35 from subgroup A (18.8%) and 24 from subgroup B (14.8%). Atrial fibrillation episodes were categorized according to the current guides5, as it can be observed in Figure 1, without noticing any significant statistical differences between the two types of DCM (ischemic and non-ischemic). It is important to mention that “persistent” atrial fibrillation could not be clearly identified in our patients because of the absence of information regarding the duration of the paroxistical episodes when sinus node rhythm restoration was not achieved during hospitalization. Twenty-one patients (6%) needed permanent pacemaker implantation, three of them having permanent atrial fibrillation (they were not pacemaker dependent).
Table 3. Echocardiographic characteristics (frequencies) in the study group
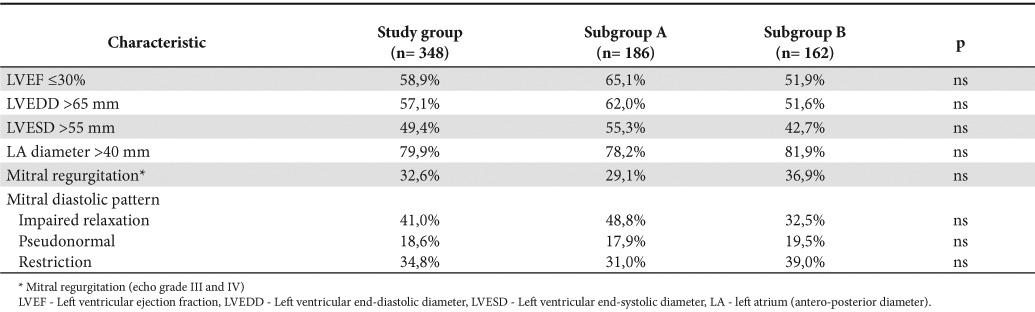
Table 4. Echocardiographic characteristics (mean +/-SD)
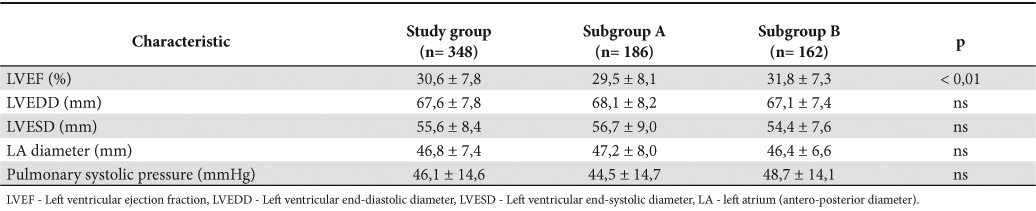
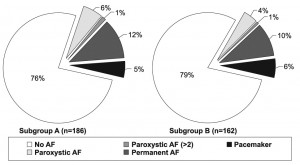
Figure 1. The prevalence of atrial fibrillation, in different forms, in the patients taken into the study
For the study of the predictive power for the onset of AF (paroxistical, permanent, or both) we choose a series of clinical, ECG and echocardiographic parameters, which we have tested in order to determine their prediction capacity by measuring the sensitivity (St), specificity (Sp), positive predictive value (PPV) and negative predictive value (NPV) of each parameter (Table 5). As a general observation, we note that the NPV were very good for all the parameters taken into consideration, whereas the PPV were low. The best value (PPV= 33%) – statistically significant (p<0.005) – was obtained for the NYHA functional class greater than 3 as a predictor for the onset of any type of AF, no matter the DCM group taken into study (39% in subgroup A, 27% in subgroup B).
Table 5. Predictive values, sensitivity and specificity of the studied parameters for presence of atrial fibrillation
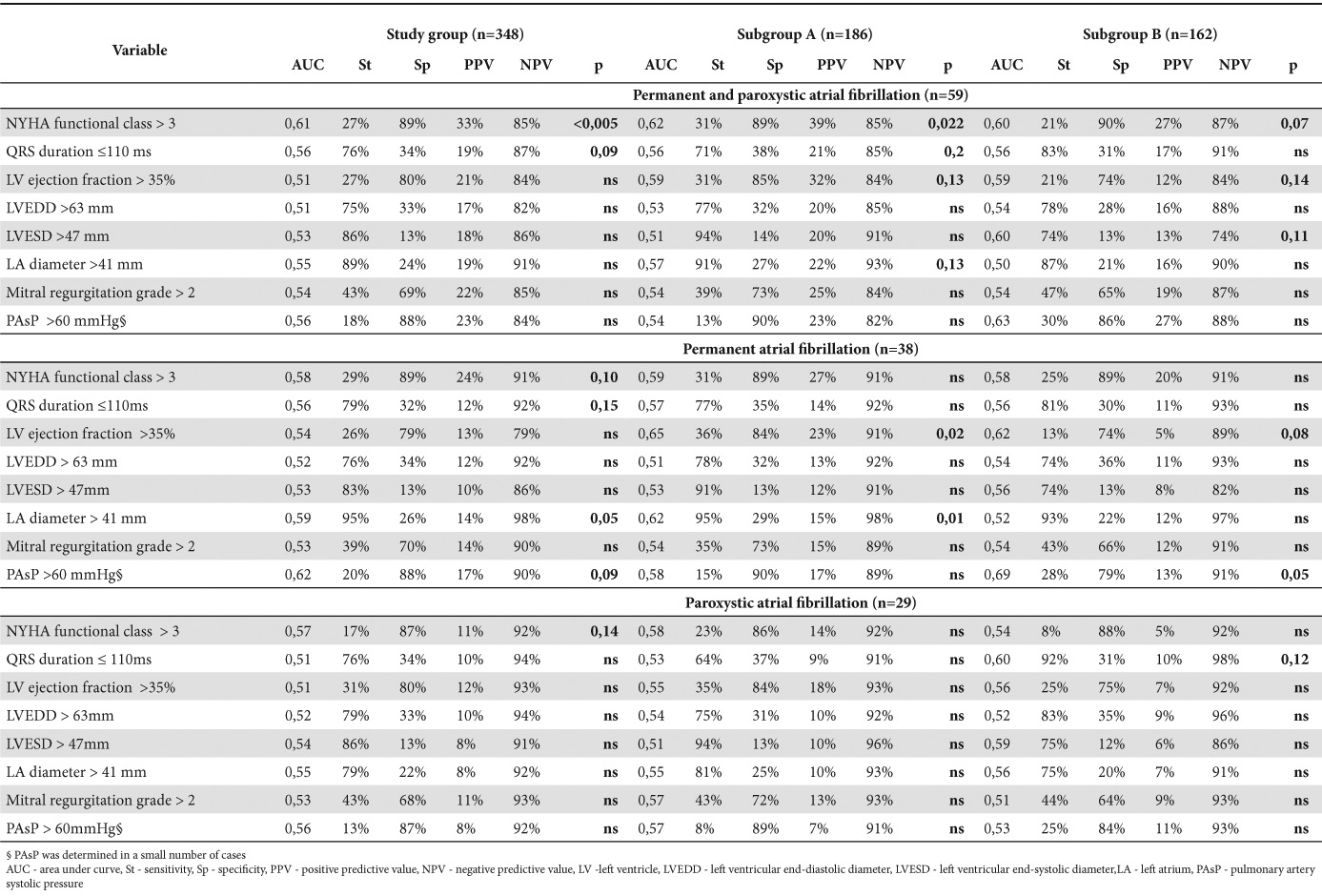
NYHA functional class greater than 3, LV ejection fraction >35%, the presence of a more than moderate mitral regurgitation or pulmonary artery systolic pressure (PAsP) > 60mmHg had a high specificity (over 70%, statistically significant only for the presence of any type of fibrillation), whereas QRS duration <110ms, LVEDD > 63 mm, LVESD > 47 mm or LA diameter > 41 mm had high sensitivity (statistically significant only for the LA diameter, in relation to the presence of permanent AF).
The univariate and multivariate analysis (Table 6) revealed a good prediction for paroxystic AF onset, realized by 2 parameters in the univariate analysis: LVEDD (HR= 2.7, 95% CI 1.02–7.11, p< 0.05) and the presence of mitral regurgitation (HR= 2.7, 95% CI= 1.02–7.11, p< 0.05); the predictive power was better in case of presence of grade 3 mitral regurgitation (HR= 3.78, 95% CI= 1.27–11.28, p <0.05). Only the grade 3 mitral regurgitation maintains its predictive power in the multivariate analysis. On the other hand, the NYHA functional class at inclusion (HR= 1.74, 95% CI=1.07–2.81, p <0.05), LA diameter (HR= 7.96, 95% CI=1.91–33.07, p <0.005) and the presence of mitral regurgitation (HR= 2.14, 95% CI= 1.04–4.42, p <0.05) proved to be good predictive factors for the presence of permanent atrial fibrillation; also, the predictive power was better for presence of grade 3 mitral regurgitation (HR= 2.47, 95% CI= 1.04–5.88, p <0.05). None of these parameters reached statistical significance in multivariate analysis. The PAsP seems to be also statistically significant, but with low HR value (1.03). We may notice that small number of determinations in the study group (only the abnormal values were recorded) can influence the statistical analysis for this parameter.
Table 6. Univariate and multivariate Cox proportional-hazards regression analysis for AF prediction
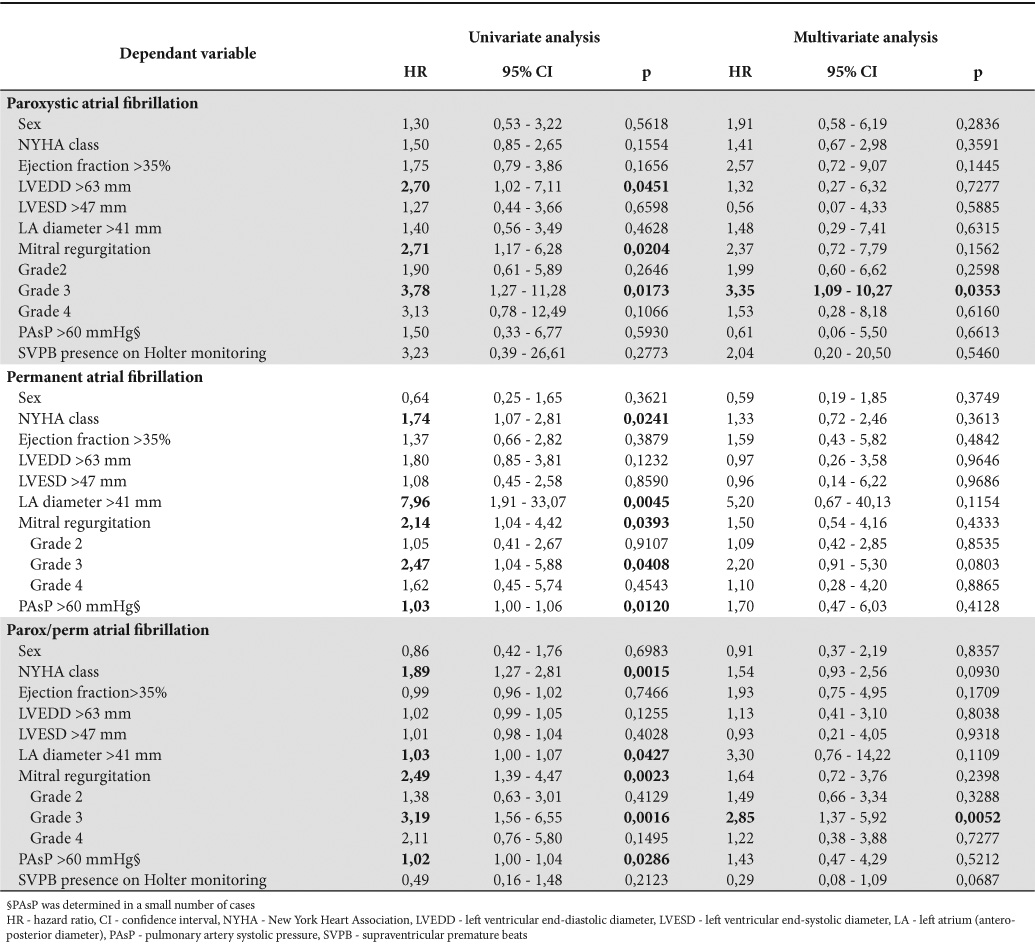
The presence of supraventricular premature beats on Holter monitoring, their number (total, maximum/hour, mean/hour), as well as therapeutic drug classes used were also studied in the uni- and multivariate analysis but none of them showed statistically significant values, so they were not mentioned.
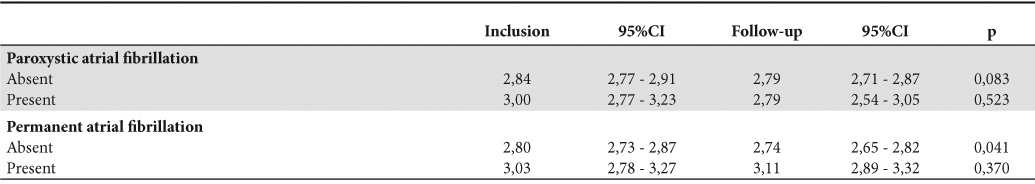
The analysis of NYHA class changes between inclusion and end of the follow-up showed no significant differences both in patients with, or without, paroxystic atrial fibrillation; in contrast, the evolution of patients with permanent atrial fibrillation shows a slight increase in the functional class, compared to those without permanent AF which maintains almost the same value (Table 7).
Table 7. The mean of the NYHA functional class for patients with, or without permanent, or paroxystic atrial fibrillation
The survival of patients with or without paroxystic AF episodes was similar (Figure 2A). Looking at patients with permanent AF, as it is shown in Figure 2B, the survival curves diverges after a period of 45 months, but without reaching statistically significance (p= 0.13). The analysis of survival curves in patients with permanent AF (Figure 2C, D) shows that patients with ischemic DCM (subgroup B), although initially seem to have a better prognosis despite the presence of AF, have a lower long term survival probability than those in non-ischemic DCM group (subgroup A). We must also consider the potential biases in the appreciation of mortality of DCM patients, as death can be the consequence of both the pump dysfunction, as well as of presence of malignant ventricular arrhythmias. One of the limitations of this study is the absence information regarding the mechanisms of death.
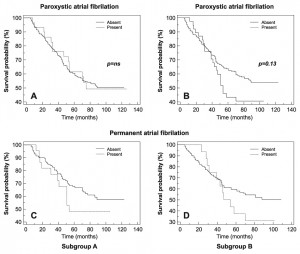
Figure 2. Kaplan – Meyer survival curves in DCM patients, with or without AF
Twenty-one patients received permanent pacemakers during the follow-up period, in three, already having AF at the time of cardiac stimulation, only biventricular re-synchronization was performed.
Discussions
Interaction and inter-relationship between AF and heart failure, as well as information on their prevalence were outlined starting from the Framingham study, estimating that it is important to consider the temporal sequence between AF and heart failure when observing relative risk for mortality associated with AF or heart failure patients, the second condition having a detrimental impact on survival7,8. With a reported prevalence between 13% and 27% in different studies, atrial fibrillation is one of important co-morbidities the patient with heart failure may face during disease evolution8-11.
Trying to determine potential predictor factors for the risk of patients with DCM and heart failure to develop atrial fibrillation during disease progression, either paroxysmal or permanent, can be difficult, as well as with malignant ventricular arrhythmias associated with this disease. Many factors, some permanent, others just with temporary appearance during disease progression (precipitating factors) may lead to an episode of AF. The presence of a systolic ventricular dysfunction (often accompanied by diastolic dysfunction) can in its turn influence the evolution of such an episode (AF) towards becoming permanent, thorough the hemodynamic modifications it induces. It is a well-known fact that the success rate of conversion to sinus rhythm and relapse prevention is when compared to the situation the above mentioned factors are absent.
Recent investigations of structural and physiological changes of atrial myocardium (both structural and electrical remodeling!) revealed that the presence of neurohormonal activation, fibrosis and apoptosis in the evolution of idiopathic DCM are important triggers for atrial fibrillation. In our study we found a relatively low prevalence of permanent atrial fibrillation (12% in the patients with idiopathic DCM and 9% in patients with ischemic etiology), somewhat at the lower compared with existing literature on patients with heart failure without take account of the etiology. Thus, when the DCM patient becomes symptomatic with heart failure symptoms, the risk of developing atrial fibrillation increases 6 times12. In our study we found a relatively low prevalence of permanent atrial fibrillation (12% in the idiopathic DCM group and 9% in patients with ischemic etiology), somewhat at the lower limit of the data existing in literature on patients with heart failure without take account of the etiology11,13,14.
At the same time, the well known implication of the renin-angiotensin-aldosterone system in the pathogenesis of heart failure contributes to the onset and maintaining of the atrial fibrillation. The increase in the production of angiotensin II contributes to the stimulation of atrial interstitial fibrosis, promoting the structural atrial remodeling. Neurohormonal modulation and adrenergic receptors blockage with angiotensin conversion enzyme inhibitors15 and beta-blockers, respectively, could explain the effectiveness of these drugs in AF prevention in patients with heart failure and DCM. However, in our study, the presence of these drug classes in the therapeutic scheme did not represent a significant risk factor or protection factor against AF. It is noticeable as a possible explanation for this fact the high prevalence (over 90%) of patients treated with both ACE-I and beta-blockers even from the inclusion in the study.
DCM patients with a low ejection fraction and increased LV end-diastolic pressure have an increased risk of LA dilatation, an important predictive factor for the onset and development of AF17. It is yet unclear whether the prognostic significance of the left atrium dilation (quantified by diameter, area or volume – it was recently showed that LA dimension increase is best quantified by volume) is the result of the diastolic dysfunction of the left ventricle, of the mitral regurgitation, or even that of the AF itself. All of these pathological conditions contribute to the dilation of the LA, having a negative influence on the prognostic of patients suffering from DCM and low ejection fraction. It is also possible that the LA dilation in patients with DCM can be caused by the myopathic atrial affliction, caused by the extension of the primary pathological process to the atrial myocardium. Pathological anatomy studies could bring further information on this subject.
Atrial fibrillation also represents one of the independent factors influencing mortality in patients with heart failure. As Macarie and colab.14 have shown, AF is a negative prognostic factor, being responsible for a 14% increase in the death risk (univariate analysis), together with the ejection fraction. Its improvement by even one unit determines a significant 3% decrease of the risk. In our study, the survival curves show the same tendency for a less favorable evolution for patients with DCM who in the course of their evolution enter permanent atrial fibrillation, without reaching statistical significance parameters; we also note that the same phenomenon is independent of the non-ischemic etiology of dilated cardiomyopathy.
The limitations of the study are mostly connected to the retrospective nature of the selected patient’s group analyses. Thus, regarding the echocardiography data, we did not have more sensitive parameters for the quantification of the LA dimensions and function, because the routine examinations performed on patients’ admission do not have a systematic record of such parameters, which generally require a large amount of time to measure. Another important limit was the absence of details concerning the causes of death, this leading to the impossibility to separate deaths caused by cardiovascular events from those caused by other factors.
Conclusions
Our study identified factors that can predict atrial fibrillation appearance in patients with dilated cardiomyopathy, regardless of its etiology (ischemic or non-ischemic). The left ventricular end-diastolic diameter >63 mm and the presence of mitral regurgitation proved to be significantly correlated to the onset of paroxystic atrial fibrillation, whereas permanent atrial fibrillation proved to be correlated to the heart failure NYHA class, the LA diameter and the presence of mitral regurgitation.
With a fairly high prevalence (7%, respectively 5% for the paroxystic atrial fibrillation and 12%, respectively 9% for the permanent atrial fibrillation in the 2 subgroups) atrial fibrillation represents one of the conditions that can contribute to the deterioration of the quality of life, by aggravating the heart failure symptoms. On the other hand, global mortality was not significantly influenced by the presence of atrial fibrillation, other factors, such as the presence of malignant ventricular arrhythmias, being to be also quantified.
List of abbreviations
ACE-I angiotensin II converting enzyme inhibitors
AF atrial fibrillation
ARB angiotensin II receptors blockers
AUC area under curve
CAD coronary artery disease
CI confidence interval
DCM dilated cardiomyopathy
EF ejection fraction
Hgb hemoglobin
HF heart failure
HR hazard ratio
LA left atrium
LV left ventricle
LVEDD left ventricular end-diastolic diameter
LVEF left ventricular ejection fraction
LVESD left ventricular end-systolic diameter
NPV negative predictive value
NYHA New York Heart Association
PAsP pulmonary artery systolic pressure
PPV positive predictive value
ROC receiver operator characteristic
SD standard deviation
SIUI Unique Computerized Integrated System
Sp specificity
St Sensitivity
SVPB supraventricular premature beats
Conflict of interest: none declared
Bibliography
1. Elliott P, Andersson B, Arbustini E et al. Classification of the cardiomyopathies: a position statement from the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J 2008;29:270-6.
2. Steinhoff JP, Sheahan RG. Tachycardia-Induced Cardiomyopathy: Atrial Fibrillation and Congestive Heart Failure. Am J Med Sci 2005;329:18-21.
3. Gheorghiade M, Bonow RO. Chronic Heart Failure in the United States: A Manifestation of Coronary Artery Disease. Circulation 1998;97:282-9.
4. Felker GM, Shaw LK, O’Connor CM. A standardized definition of ischemic cardiomyopathy for use in clinical research. J Am Coll Cardiol 2002;39:210-8.
5. Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association (EHRA). Endorsed by the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2010;31:2369-429.
6. K/DOQI Clinical Practice Guidelines on Chronic Kidney Disease. Evaluation, classification, and stratification. Kidney Disease Outcomes Quality Initiative. Am J Kidney Dis 2002;39:S1-S266.
7. Wang TJ, Larson MG, Levy D et al. Temporal Relations of Atrial Fibrillation and Congestive Heart Failure and Their Joint Influence on Mortality. Circulation 2003;107:2920-5.
8. Middlekauff HR, Stevenson WG, Stevenson LW. Prognostic significance of atrial fibrillation in advanced heart failure. A study of 390 patients. Circulation 1991;84:40-8.
9. Carson PE, Johnson GR, Dunkman WB, Fletcher RD, Farrell L, Cohn JN. The influence of atrial fibrillation on prognosis in mild to moderate heart failure. The V-HeFT Studies. The V-HeFT VA Cooperative Studies Group. Circulation 1993;86:VI102-VI110.
10. Senni M, Tribouilloy CM, Rodeheffer R et al. Congestive Heart Failure in the Community : A Study of All Incident Cases in Olmsted County, Minnesota, in 1991. Circulation 1998;98:2282-9.
11. Swedberg K, Olsson LG, Charlesworth A et al. Prognostic relevance of atrial fibrillation in patients with chronic heart failure on long-term treatment with beta-blockers: results from COMET. Eur Heart J 2005;26:1303-8.
12. Kanoupakis EM, Kallergis EM, Mavrakis HE et al. Electrophysiological and electroanatomical mapping of the right atrium in patients with dilated cardiomyopathy: relation to the collagen turnover and to increased propensity for AF. Europace 2009;11 (suppl 2):Abstract 287.
13. Apetrei E. Fibrilatia atriala si insuficienta cardiaca. Rom Journal of Cardiol 2012;1:1-3.
14. Macarie Tepes Piser I, Macarie C. Atrial fibrilation and survival in patients with heart failure and low ejection fraction. Rom Journal of Cardiol 2012;1:4-13.
15. Healey JS, Baranchuk A, Crystal E et al. Prevention of Atrial Fibrillation With Angiotensin-Converting Enzyme Inhibitors and Angiotensin Receptor Blockers: A Meta-Analysis. J Am Coll Cardiol 2005;45:1832-9.
16. Abi Nasr I, Bouzamondo A, Hulot JS, Dubourg O, Le Heuzey JY, Lechat P. Prevention of atrial fibrillation onset by beta-blocker treatment in heart failure: a meta-analysis. Eur Heart J 2007;28:457-62.
17. Abhayaratna WP, Seward JB, Appleton CP et al. Left Atrial Size: Physiologic Determinants and Clinical Applications. J Am Coll Cardiol 2006;47:2357-63.
 This work is licensed under a
This work is licensed under a