Cristina Bucşa¹, A. Bucşa², L. Zarma², M. Croitoru², P. Platon², M. Postu², Diana Tacu¹, Eminee Kerezsy¹, I. Sinescu¹, D. Deleanu²
1 Fundeni Clinical Institute, Renal Transplantation Department, Bucharest
2 “Prof. Dr. C. C. Iliescu” Emergency Institute for Cardiovascular Diseases, Bucharest
Contact address:
Cristina Bucşa, MD, Fundeni Clinical Institute, Bucharest.
E-mail: cristinabucsa@yahoo.com
Abstract: Aim of the study – To evaluate the feasibility and the results of percutaneous coronary interventions for acute coronary syndromes in renal transplant recipients. Material and method – Retrospective analysis of ten cases of renal transplant patients who experienced an acute coronary syndrome between January 1st 2005 and December 31st 2011. Those patients underwent invasive coronary angiography followed, in most cases, by coronary angioplasty with stenting. The mean age of the patients was 45 years, with a M/F proportion of 6/4. All patients had severe dyslipidemia, probably due to the immunosuppressive treatment, but the percentage of diabetic patients was only 20%. Results – Most patients, seven out of ten, suffered an ST elevation myocardial infarction and the treatment was primary coronary angioplasty. Procedural success was declared in all cases but with the number of stents implanted per patients was higher than in other cases of primary angioplasty (1.57 stents per procedure). The clinical outcome, both immediate and at one year, was good and the function of the renal graft was not affected in none of the cases. Regarding the other three cases: one had an acute coronary syndrome without ST-segment elevation and it was treated by implantation of two stents; another one had a three-vessel disease and subsequently underwent coronary bypass surgery; the last case was very severe and died due to a cardiac wall rupture. Conclusions – Recent developments in the fields of interventional cardiology and of renal transplantation are responsible for the encounter of a pathology that was rather rare until recently, namely the acute coronary syndromes in renal transplant recipients. The modern treatment in this situation is the coronary angiography, followed, in most cases, by the implantation of one of more coronary stents. The outcome of these procedures is good and the prevention of renal graft failure can be done easily, in collaboration with the transplant nephrologist.
Keywords: renal transplant, acute coronary syndrome
Rezumat: Obiectivele studiului – Evaluarea fezabilității și rezultatului intervențiilor coronariene percutane în cazul sindroamelor coronariene acute apărute la pacienții transplantați renal. Material și metodă – Au fost analizate retrospectiv un număr de zece cazuri de pacienți purtători de transplant renal care, între 1 ianuarie 2005 și 31 decembrie 2011 au suferit un sindrom coronarian acut. La acești pacienți s-a efectuat angiografie coronariană care, în general, a fost urmată de o angioplastie coronariană cu implantare de stent. Media de vârstă a pacienților a fost de 45 de ani, cu un raport M/F de 6/4. Toți pacienții prezentau dislipidemie importantă, posibil și din cauza medicației imunosupresoare, dar proporția de pacienți cu diabet zaharat a fost doar de 20%. Rezultate – Majoritatea pacienților, șapte la număr, au avut un infarct miocardic cu supradenivelare de segment ST care a fost tratat prin angioplastie coronariană primară. Succesul procedural a fost înregistrat în toate cele șapte cazuri, deși numărul mediu de stenturi implantate la un pacient a fost mai mare decât în rândul populației generale de pacienți cu angioplastie primară (1.57 stenturi/procedură). Evoluția clinică imediată și la un an a fost bună, iar funcția grefei renale nu a înregistrat deteriorare în niciunul dintre cazuri. În ceea ce privește restul de trei cazuri, s-au înregistrat un sindrom coronarian acut fără supradenivelare de segment ST care a beneficiat de o angioplastie cu două stenturi, un pacient multicoronarian la care s-a practicat o operație de bypass aortocoronarian și un caz care a decedat din cauza unei rupturi de cord. Concluzii – Dezvoltarea recentă a unor domenii cum sunt cardiologia intervențională sau transplantul renal a dus la apariția unor cazuri mai rar întâlnite până acum, și anume sindroamele coronariene acute la pacienții care au un rinichi transplantat. Tratamentul modern în aceste situații este explorarea coronarografică, urmată, de cele mai multe ori, de implantarea unuia sau mai multor stenturi coronariene. Rezultatul acestor proceduri, imediat și la distanță, este bun, iar prevenirea afectării grefei renale necesită minime precauții dar și colaborarea cu medicul nefrolog.
Cuvinte cheie: transplant renal, sindrom coronarian acut
INTRODUCTION
Many studies show that the renal transplantation is now seen as the best treatment for patients with end-stage renal disease (ESRD) because the renal transplant recipients have a better quality of life and a longer survival compared to patients on dialysis1. Still, the cardiovascular disease is by far more common in the renal transplant patients than in the general population, representing the leading cause of death in this group5. Some interesting figures show that nearly 50% of the patients die with a functional renal graft and, from these deaths, 50% are of cardio- or cerebrovascular origin6-8.
The large prevalence of atherosclerosis in renal transplanted patients has several causes (Table 117). First of all, we should mention the traditional risk factors for the atherosclerotic disease: high blood pressure, smoking, dyslipidemia, diabetes mellitus, age, etc. We should remark here the high prevalence of diabetes as a cause of renal failure, especially in the developed countries, and also the increasing age of the patients undergoing renal transplantation. Beside the traditional risk factors there are some elements specific to the renal disease or to the post-transplant status: the graft function after transplantation and the number of acute rejection; hyperhomocysteinemia and elevation of some inflammatory markers; development of diabetes mellitus after transplant; secondary effects of the immunosuppressive medication1.
Table 1. Risk factors for coronary artery disease after kidney transplantation
| Study | Nr. pts. | %CAD | Risk factor | Relative risk |
| Kasiske BL et al, 2000 | 1124 | 10.9% | Age Cholesterol Blood pressure Diabetes Smoking |
Men 1.05/women 1.40 Men 2.13/women 2.24 Men 1.47/women 0.31 Men 2.78/women 5.4 Men 1.95/women 1.82 |
| Kasiske BL et al, 1996 | 706 | 26% | Age Male gender LDL Blood pressure Diabetes Acute rejection Splenectomy |
1.88 2.68 No effect No effect 3.25 1.40 2.07 |
| Aakhus S et al, 1999 | 406 | 14% | Age Male gender Cholesterol |
NA NA NA |
| Lindholm A et al, 1995 | 1347 | 40% | Age Diabetes Acute rejection |
1.06 3.94 2.02 |
The number of acute rejection episodes seems to be directly related to the cardiovascular risk9-10 and the return to dialysis leads to an important increase in mortality. Graft dysfunction can produce, among other effects, hyperhomocysteinemia, a known risk factor for atherosclerosis, both in general population and in the transplant patients12,13. The relation between the fasting levels of homocysteinemia was observed during a study on 207 patients with renal transplant monitored during an average time of 21.2 months; the results showed that the risk of having such an event rises with 6% by every increase in serum homocysteinemia of 1 µmol/l13.
In regards to the toxic effects of the immunosuppressive medication, we enumerate here some of the adverse reactions of the main categories of drugs. The calcineurin inhibitors (tacrolimus) decrease the renal flow and are associated with increase in the systemic vascular resistances and in the blood pressure. Tacrolimus increases the oxidation of the LDL-cholesterol particles but can also lead to the development of the diabetes after transplant by inhibiting the insulin production in the ß-pancreatic cells. Corticosteroids and cyclosporine increase the incidence of the high blood pressure, diabetes and dyslipidemia. Rapamycin (sirolimus), a macrolid antibiotic used as immunosuppressive agent, is associated with important hypertriglyceridemia and hypercholesterolemia, especially when it’s used in combination with cyclosporine.
Concerning the clinical forms of coronary artery disease, a research on almost one thousand patients with renal transplant17 shows a relative high proportion of asymptomatic patients but in which the coronary angiography demonstrated significant lesions, with indication for revascularisation. The same study suggests a better survival at 5 years for those patients treated with coronary bypass surgery or percutaneous coronary interventions, compared with the conservative treatment. Acute coronary syndromes incidence in renal transplant recipients with diabetes was 0.79% per patient-year, compared to 1.69% per patient-year in the patients on dialysis, before the renal transplantation.
METHODS – THE STUDY GROUP
The purpose of this study is to assess the particularities of the percutaneous coronary interventions (PCI) in patients with a renal transplant who suffered an acute coronary syndrome, analysing both clinical and angiographic parameters. The study group included ten patients with renal transplants of different ages, which were performed at the Fundeni Clinical Institute. These ten patients suffered an acute coronary syndrome (ACS) between January 1st 2005 and December 31st 2011 and subsequently underwent coronary angiography in the Department of Invasive Cardiology at the Prof. Dr. C. C. Iliescu Emergency Institute for Cardiovascular Diseases. Although the number of patients seems low, especially when compared with the impressive series of hundreds of patients reported in large transplant centres from around the world, we should notice that both the interventional cardiology and the renal transplantation experienced important increases in experience especially in the last ten to fifteen years and the cases situated at the intersection of these two subspecialties are still rather few.
From the study group of ten patients, seven had an ST elevation myocardial infarction (STEMI) and were treated by primary percutaneous coronary intervention (PPCI). Two cases had a non ST elevation ACS, one being treated by implantation of two drug eluting stents (DES) and the other one by coronary artery bypass surgery. Finally, the last case presented at 72 hours from the onset of an ACS with a terrible complication, meaning rupture of the interventricular septum, possibly associated with a free ventricular wall rupture (transthoracic echocardiography data); the patient deceased soon after, before a surgery could be performed. This high proportion (7 out of 10) of the PPCI in the cases of renal transplant recipients who supported a coronary angiography for an ACS suggests that there is still some reticence to indicate this invasive approach to a larger number of patients, in situations that are less severe than a STEMI.
We will start by presenting the general characteristics of the whole group of ten patients; after that, we will pay a special attention to the subgroup of 7 patients who underwent PPCI (Table 2). The demographic data of the whole study group show the next findings: the mean age was 45 years, with limits between 31 and 62 years, and the sex ratio was M/F=6/4. The prevalence of the traditional risk factors was as follows: dyslipidaemia 100%, hypertension 80%, smoking 20%, diabetes 20%. One should notice that dyslipidaemia was found in every patient, probably due to the immunosuppressive medication prescribed after renal transplantation. Instead, the percentage of diabetic patients looks small (20%), considering the fact that in the general PCI population this proportion is around 25%. Regarding the clinical presentation, this was not different from the symptoms encountered in other patients with ACS: prolonged chest pain, accompanied or not by dyspnea, was the cardinal symptom that was found in all patients.
Table 2. Demographic data and risk factors in the study group
| General group (n=10 pts.) |
STEMI subgroup (n=7 pts.) |
|
| Age (mean/limits) | 45/31-62 | 42/31-62 |
| Sex (M/F) | 6/4 | 4/3 |
| Dyslipidemia (%) | 100 | 100 |
| Hypertension (%) | 80 | 85.7 |
| Smoking (%) | 20 | 14.2 |
| Diabetes (%) | 20 | 14.2 |
Here are some of the findings that are specific to the post-transplant status. Seven patients had a renal graft transplanted from living donor and in the rest of three the transplant was from a dead heart-beating donor. The mean duration of dialysis before transplantation was 28 months and the mean time from transplantation was 50.4 months. The immunosuppressive therapy consisted in an association of corticosteroids and other drugs in 7 cases, and in 3 cases the regimen was corticosteroid-free.
In the analysis of the subgroup of 7 cases with PPCI we will first present the general demographic data and subsequently we will present some specific features of the interventional procedure and of the postprocedural outcome (Table 3). The patients’ age varied between 31 and 62 years, with a mean value of 42 years, slowly younger than in the whole group; the gender ratio was M/F=4/3. The risk factors prevalence was: dyslipidaemia 7/7; hypertension 6/7; smoking 1/7; diabetes 1/7. Five patients received a renal graft from a living donor and two from cadaver. The mean duration of pre-transplantation dialysis was 24 months and the mean time from transplantation was 44 months. The immunosuppressive maintenance medication was a combination of steroids, cyclosporine and mycophenolate mofetil in 5 cases and a free-steroid regimen with tacrolimus and rapamycin in 2 cases.
Table 3. Procedural data for the coronary angioplasty in STEMI cases
| General group (n=10 pts.) |
|
| Mean time from onset to reperfusion | 4.7 hours |
| Infarct-related artery | LAD : 3 RCA : 4 |
| TIMI flow pre-intervention | TIMI 0 : 5 TIMI III: 2 |
| Nr. of stents per procedure | 1.57 |
| TIMI flow post-intervention | TIMI 3: 6 TIMI 2 : 1 |
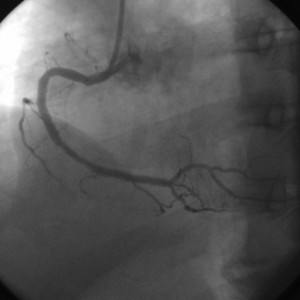
The mean time from the symptom onset to the interventional opening of the culprit vessel was 4.7 hours, which is a very acceptable value in our practice. The arterial approach was femoral in all seven cases; we preferred the left femoral artery as arterial approach because the transplanted kidney is placed generally in the right iliac fossa and its artery is anastomosed with the right internal iliac artery of the recipient. The infarct-related artery was the right coronary artery (RCA) in 4 cases and the left anterior descending (LAD) in 3 cases. The TIMI flow on arrival was 0 in 5 cases (total occlusion) and III in 2 cases (spontaneous reperfusion). The mean number of stents implanted per procedure was 1.57, significantly higher than in the general population of PPCI patients, where the number of stents used for a patient is around 1.1. All the stents were bare metal stents (BMS). The results of the interventions were good, with TIMI III flow at the end of the procedures in 6 cases and TIMI II in one case. These angiographic results, combined with the relatively short time until presentation, lead to a very good postprocedural outcome, all the patients being discharged in NYHA I functional class (4 cases) or NYHA II (3 cases). According to the transthoracic echocardiograms performed before discharge, the mean ejection fraction of the left ventricle was 47% (limits 40% to 55%). The prevention of the contrast-induced deterioration of the renal graft function was done by intravenous administration of saline solution during and after the procedure. The serum creatinine values were obtained daily a few days after the intervention; the renal function was unchanged in all seven cases, the mean serum creatinine value being almost the same before procedure and at discharge.
The medication prescribed at discharge included dual antiplatelet therapy (aspirin and clopidogrel), statin and beta-blocker in all patients, angiotensin converting enzyme inhibitor in 5 cases and diuretic in 2 cases.
Follow up was done at 1, 3, 6 and 12 months after the procedure and it included only non-invasive tests. The stress electrocardiography testing was avoided in asymptomatic patients. The outcome was in general favourable, with only one case in which the repeat of the angioplasty was needed, due to a clinical significant restenosis.
DISCUSSION
The introduction of the coronary angioplasty as the standard treatment in the setting of an acute ST elevation myocardial infarction was done in our country only in the last three years, which is a very important step through the normalisation of the cardiac patients care. On the other side, the growing number of patients receiving a renal transplant (530 between 2006 and 2010 versus 436 between 2001 and 2005 in our centre, more than 20% increase) leads to a higher number of such patients presenting with an acute coronary syndrome. As we demonstrated, the invasive coronary angiography, the percutaneous coronary interventions and even the cardiac surgery can be performed in this patient population with good results and minimal precautions. Although, technically, the PPCI can be a little bit more challenging than in the general population, the outcomes regarding the cardiac function, but also the renal graft function, are good, and the medical management is not very different from standard patients. In the years to come we will see how much the renal transplant population undergoing coronary interventions, for both acute or chronic situations, will increase. Of note is also the role of the drug eluting stents in this category of patients, knowing that the substance eluted by the stent is sometimes similar in structure with some of the immunosuppressive medication taken orally by the transplant recipients.
CONCLUSIONS
The significant progress registered in some subspecialties like interventional cardiology or transplant nephrology in our country in the last ten years led to the development of a pathology rather rarely encountered until now, which is the acute coronary syndromes in patients with a transplanted kidney. The cornerstone of the therapeutic decision is the diagnostic using the invasive coronary angiography. In many cases, including major emergencies like STEMI or NSTEMI, the interventional therapy with implantation of one or more coronary stents, BMS or DES, leads to very good clinical results on the short and mid-term. In some cases coronary surgery can be performed but these situations are still scarce. Prevention of contrast-induced nephropathy is made by standard methods applied in the general population; the medical treatment and the follow-up after intervention are made in cooperation with the nephrologist. These good results achieved in emergency situations suggest that the coronary angiography should be indicated more frequently by the cardiologist or the nephrologist for a renal transplanted patient suspected of coronary artery disease, because the risks related to this investigation are few while the benefits can be very important.
Acknowledgement: This paper is supported by the Sectoral Operational Programme Human Resources Development (SOP HRD) 2007-2013, financed from the European Social Fund and by the Romanian Government under the contract number POSDRU/107/1.5/S/82839
References
1. Kiberd BA, Cardiovascular disease in kidney transplant recipients. Johns Hopkins Advanced Study in Medicine, volume 7 (6).
2. Pita-Fernández et al.: Incidence of cardiovascular events after kidney transplantation and cardiovascular risk scores: study protocol. BMC Cardiovascular Disorders 2011, 11:2.
3. Wolfe RA, Ashby VB, Milford EL, et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med. 1999;341:1725-1730.
4. Bucsa C, Tacu D, Ceck C, Kerezsy E, Domnisor L, Daia D, Sinescu I. The impact of renal transplantationon the evolution of severe confgestive heart failurein patients with end stage reanal disease. In Annals of Fundeni Hospital, vol. 13, no. 3-4, 2008.
5. U.S. Renal Data System, USRDS 2009 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2009.
6. Ojo AO, Hanson JA, Wolfe RA, et al. Long-term survival in renal transplant recipients with graft function. Kidney Int. 2000;57:307-313.
7. Fellström B. Risk factors for and management of post-transplantation cardiovascular disease. BioDrugs. 2001;15:261-278.
8. Lindholm A, Albrechtsen D, Frodin L, et al. Ischemic heart disease – major cause of death and graft loss after renal transplantation in Scandinavia. Transplantation. 1995;60:451-457.
9. Wong BM, Huang M, Zaltzman JS, et al. Mycophenolate mofetil and C-reactive protein in renal transplant recipients. Transplantation. 2007;
83:48-53.
10. Kasiske BL, Guijarro C, Massy ZA, et al. Cardiovascular disease after renal transplantation. J Am Soc Nephrol. 1996; 7: 158-165.
11. Kasiske BL. Risk factors for accelerated atherosclerosis in renal transplant recipients. Am J Med. 1988;84:985-992
12. Arnadottir M, Hultberg B, Vladov V, et al. Hyperhomocysteinemia in cyclosporine-treated renal transplant recipients. Transplantation. 1996;61:509-512.
13. Ducloux D, Motte G, Challier B, et al. Serum total homocysteine and cardiovascular disease occurrence in chronic, stable renal transplant recipients: a prospective study. J Am Soc Nephrol. 2000;11:134-137.
14. Vanrenterghem Y, Claes K, Montagnino G, Fieuws S, Maes B, Villa M, Ponticelli C: Risk factors for cardiovascular events after successful renal transplantation. Transplantation 2008, 85(2):209-216.
15. Boden WE, O’Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, et al. COURAGE Trial Research Group. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007; 356:1503-1516.
16. Enkiri SA et al. Coronary angiography is a better predictor of mortality than noninvasive testing in patients evaluated for renal transplantation. Catheterization and Cardiovascular Interventions 76:795-801 (2010).
17. Hypolite IO et al. Acute Coronary Syndromes after Renal Transplantation in Patients with End-Stage Renal Disease Resulting from Diabetes. American Journal of Transplantation 2002; 2: 274±281.
18. Koushik R, Kasiske BL. The prevention and treatment of coronary artery disease in kidney transplant recipients. In Weir RM, Medical management of kidney transplantation, Ed. Lippincott Williams& Wilkins, 2005.
19. Gang S, Dabhi M, Rajapurkar MM. Ischaemia imaging in type 2 diabetic kidney transplant candidates-is coronary angiography essential? Nephrol Dial Transplant 2007;22:2334-2338.
20. De Lima JJ, Sabbaga E, Vieira MLC, de Paula FJ, Ianhez LE, Krieger EM, Ramires JAF. Coronary angiography is the best predictor of events in renal transplant candidates compared with noninvasive testing. Hypertension 2003;42:263-268.
21. Jones DG, Taylor AM, Enkiri SA, Lobo P, Brayman KL, Keeley EC, Lipson LC, Gimple LW, Ragosta M. Extent and severity of coronary disease and mortality in patients with end stage renal failure evaluated for renal transplantation. Am J Transplant 2009;9:1-7.



 This work is licensed under a
This work is licensed under a