Claudia Matei1, Gabriela Kozma1, Dan Bindea3, Calin Pop1,2
1 “Dr. Constantin Opris” Emergency County Hospital, Baia Mare, Romania
2 “Vasile Goldis” West University, Arad, Romania
3 “Niculae Stancioiu” Heart Institute, Cluj-Napoca, Romania
Abstract: Introduction – Atrial fibrillation (AF) accounts for over 50% of strokes, also known as cerebrovascular accidents (CVAs). We report a case of a right atrial (RA) myxoma presenting as paroxysmal AF, syncope and acute chest pain, in a patient with previous CVA. Description of the problem. A 62-year-old Caucasian woman was admitted for an episode of syncope and acute chest pain. Two years earlier she had suffered a CVA. Paroxysmal AF was noted at that time. At current presentation pulmonary thromboembolism (PE) was ruled out by pulmonary CT. TTE combined with TOE showed a large moving mass in the RA, prolapsing through the tricuspid valve into the right ventricle. The coronary arteries were normal. The patient underwent surgical treatment. The histopathological study confi rmed diagnosis of myxoma. Questions, problems. Up to 25% of myxomas are found in RA. Chest pain is infrequent. Syncope is experienced by approximately 20% of patients. Our patient had confirmed TTE obstruction of the tricuspid valve and PE was ruled out by CT pulmonary scan. Conclusions – TTE must be considered at admission to clarify etiology in all AF and stroke patients. Although TOE is more sensitive, TTE is usually adequate for the diagnosis of cardiac myxomas.
Keywords: atrial fibrillation, syncope, myxoma, right atrium
CASE REPORT
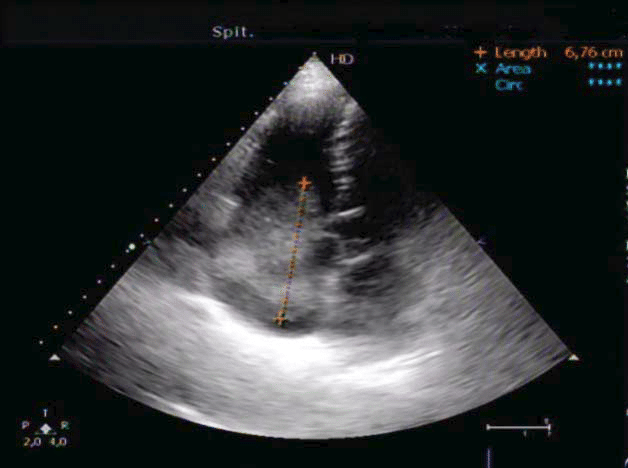
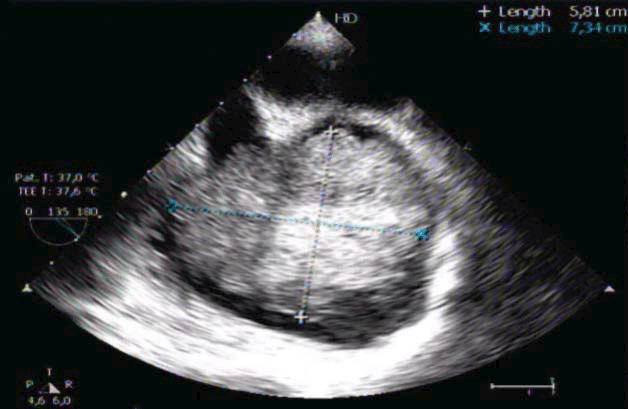
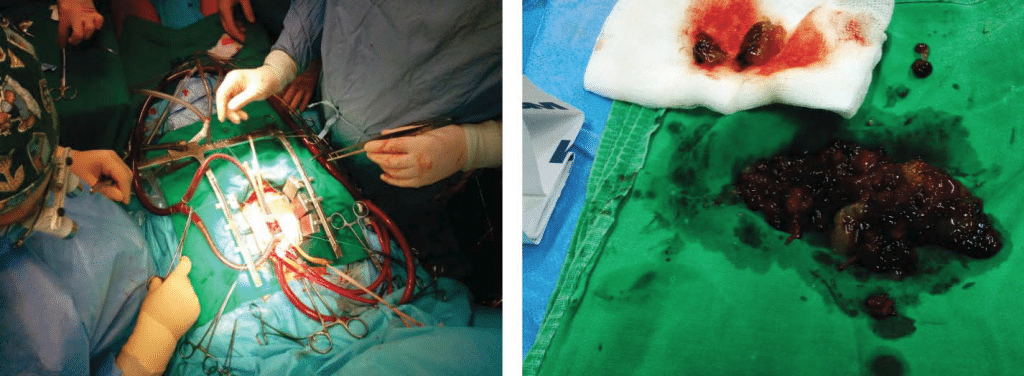
A 62-year-old Caucasian woman was admitted to the Emergency Department (ED) for an episode of syncope and acute chest pain. She had a history of high blood pressure (7-8 years duration), regularly treated with antihypertensive therapy. Two years previously, she had an episode of cerebrovascular accident (CVA), believed to have been embolic in origin. Paroxysmal atrial fibrillation (AF) was noted at that time, no transthoracic echocardiogram (TTE) was performed in the ED, but she was on antivitamin K oral anticoagulants, with no regular control of anticoagulation. The patient also informed us of dyspnea on moderate exertion and discrete weight loss in the last two months. The clinical examination revealed irregular heart rhythm, moderate systolic murmur at the left upper sternal border, and splitting of S1. During the hospitalization we performed several investigations for complete diagnosis: neurological exam, ECG, laboratory examination, CT pulmonary angiography, TTE, transesophageal echocardiography (TOE), as well as coronary angiography. The neurological examination did not find any changes from her previous assessment. A head CT scan confirmed the previous single site CVA. The ECG – showed AF with nonspecific changes. The results of blood tests were within the normal range, except erythrocyte sedimentation rate (104 mm/h), fibrinogen (498 mg/dl) and C-reactive protein (44.5 mg/L), D-dimers >5 pg/ mL DDU. The first suspicion in the ED was pulmonary thrombembolism (PE), ruled out by the CT pulmonary angiography. TTE showed a normal left ventricle size and function (ejection fraction 60%), but also a moving mass in the right atrium (RA), an increased RA, right ventricular volume overload, and a dilated inferior vena cava (Figure 1). The TOE revealed the tumor that was attached to the free wall of the RA, suggesting a myxoma that was prolapsing through the tricuspid valve into the right ventricle during diastole (Figure 2). The coronary artery was normal at angiography (preoperative assesment). After completion of preoperative diagnoses, the patient was transferred to another institution for surgical treatment. Surgical exploration of the RA revealed a 7.0 x 6.3 cm mass, friable and with hemorrhagic areas, attached to the free wall of the RA (Figure 3). The mass was successfully excised. Histological examination of the mass confi rmed the diagnosis of cardiac myxoma. We continued with follow- up of the patient by TTE control right after surgical treatment, as well as 3, 6 and 12 months after, with no signs of tumor recurrence. She feels well and continues to take antihypertensive drugs and antivitamin K oral anticoagulants regularly.
Figure 1. TTE image, apical 5 chambers view – large right atrial mass partially obstructing the tricuspid valve.
Figure 2. TOE image – massive right atrial mass partially obstructing the tricuspid valve.
DISCUSSIONS
Myxomas account for 40-50% of primary cardiac tumors and 75% of sporadic myxomas occur in females. The estimated prevalence results in 75 cases of myxoma per million autopsies1. Early diagnosis may be a challenge because of nonspecific symptoms. These are more pronounced when the myxomas are left-sided, and over 5 cm in diameter2. Up to 25% of myxomas are found in RA. Presenting complaints relate to tumor location, which predicts mechanical interference with cardiac function and influences embolic sites (pulmonary or systemic). Sudden death may occur in 15% of patients, by coronary or systemic embolization or due to the obstruction of blood fl ow at the mitral or tricuspid valve. Chest pain is infrequent and may be due to coronary embolization3.
The presence of an intracardiac shunt may result in a paradoxical embolism4. TOE did not confirm the presence of an intracardiac shunt in our patient. Previous CVA was, in this case, caused by paroxysmal AF. Cardiac arrhythmias (AF and atrial fl utter) reportedly occur in approximately 20% of patients with cardiac myxoma. In one study, 19% of the patients had AF associated with large atrial myxoma. Was the paroxysmal AF also secondary to the interferences with the mechanical function of the atria? Left atrial myxomas become symptomatic when they reach about 70g. RA myxomas grow to approximately twice the size of left atrial myxomas before producing symptoms. The exact rate of growth is not known. Tumors vary widely in size, ranging from 1-15 cm in diameter. In one case report, the RA myxoma had a growth rate of 1.36 X 0.03 cm/month5,6. In this case RA myxoma was certainly present at the first episode of AF (tumor size at diagnosis 7.0 x 6.3 cm). Large atrial myxomas could produce episodic mitral or tricuspid valvular obstruction and the patient can present with intermittent syncope, dizziness, or sudden death2. The Guidelines for the diagnosis and management of syncope (2009) recommend echocardiography including evaluation of structural and functional haemodynamic data in oreder to diagnose the presence of structural cardiac disease. As in our case, echocardiography may identify the cause of syncope, when no more tests are needed (e.g. aortic stenosis, atrial myxoma, tamponade, etc8. The patient had confirmed TTE and TOE obstruction of the tricuspid valve (the tumor was located close to the orifi ce of the inferior vena cava with prolapse in the right ventricle and intermittent obstruction), causing syncope. Right atrial myxomas can also embolize to pulmonary vessels and produce signs of pulmonary hypertension. PE was ruled out by a CT pulmonary scan. In this case, when the patient was admitted for CVA – two years ago – she was not TTE examined. That is why we would like to stress the importance of echocardiography; TOE has been reported as having 100% sensitivity for cardiac myxoma and is preferred over TTE. TOE now permits the location, origin, size, shape, attachment, mobility, valve compromise and hemodynamic consequences to be determined6. In our case, TOE revealed the tumor that was attached to the free wall of the RA. The most common site of attachment is at the border of the fossa ovalis, although myxomas can also originate from the posterior atrial wall, the anterior atrial wall, or the atrial appendage. The mobility of the tumor depends upon the extent of attachment to the interatrial septum and the length of the stalk7. The patient was fortunate not to have suffered from a fatal complication during the last two years. The particularity of the case lies in the fact that, although it is a patient with numerous antecedents, a complete clinical examination combined with laboratory, ECG and TTE examinations would have been enough for a reliable diagnosis of myxoma since she presented with stroke. We consider that TTE is necessary in all patients with syncope and / or stroke. The other tests used to identify the etiology of the syncope – TOE, CT and coronary angiogram were all performed for preoperative assessment.
Figure 3. Intraoperative images – extracorporeal circulation (left image) and large right atrial mass excised (right image).
CONCLUSIONS
• All patients with new onset, apparently isolated AF, should undergo TTE to exclude structural heart diseases.
• All patients with suspected embolic CVA should undergo TTE/TOE to exclude cardio embolic etiology.
• Paroxysmal AF, syncope and stroke is a frequent clinical association requiring several investigations for complete diagnosis.
• Atrial myxoma is the most common primary cardiac tumor, usually presenting with non-specific constitutional, obstructive or embolic symptoms. Myxomas produce symptoms mimicking mitral or tricuspid stenosis or regurgitation, endocarditis, PE, CVA, carcinoid or collagen disease, or atrial thrombus. Atrial arrhythmia is an unusual manifestation.
• With early surgery, the long-term prognosis for atrial myxomas is excellent.
Conflict of interest: none declared.
References
1. Thiene G, Valente M, Lombardi M, Basso C. Tumors of the heart. The ESC Textbook of Cardiovascular Medicine. 2nd ed.; 2009: 735-62.
2. Obrenovic-Kircanski B, Mikic A, Parapid B, et al. A 30-year-single-center experience in atrial myxomas: from presentation to treatment and prognosis. Thorac Cardiovasc Surg 2013; 61(6): 530-6.
3. Karagounis A, Sarasam M. Myxoma of free wall of the right ventricle: a case report. J Card Surg; 2005; 20(1): 73–6.
4. Paraskevaidis IA, Triantafi lou K, Karatzas D, Kremastinos DT. Right ventricular multiple myxomas obstructing right ventricular outfl ow tract. J Thorac Cardiovasc Surg 2003; 126(3): 913.
5. Pergolini A, Zampri G, Sbaraglia F, Musumeci F. Left atrial myxoma: two sides of the coin. J Cardiovasc Med (Hagerstown); 16(2): S74-76.
6. Mary L. Grebenc, Melissa L. Rosado-deChristenson, Curtis E. Green, Allen P. Burke, MD Jeffrey R. Galvin. From the Archives of the AFIP Cardiac Myxoma: Imaging Features in 83 Patients1. RadioGraphics; 2002; 22: 673–689
7. Hasdemir H, Alper AT, Arslan Y, Erdinler I. Left atrial myxoma with severe neovascularization: role of preoperative coronary angiography. Turk Kardiyol Dern Ars 2011; 39(2): 163-5.
8. Moya A et all. Guidelines for the diagnosis and management of syncope (version 2009). European Heart Journal 2009; 30: 2631–2671.
 This work is licensed under a
This work is licensed under a