Radu Stavaru1, Diana Grapa2, Gabriel Stanica1, Andreea Cuculici1, Razvan Radu1, Marin Postu1
1 Emergency Institute of Cardiovascular Diseases “Prof. Dr. C. C. Iliescu”, Bucharest, Romania
2 Sanador Hospital, Bucharest, Romania
Abstract: World-wide, the most frequent cause of death is coronary artery disease (CAD), responsible, every year, for the death of seven million people, accounting for 12.8% of all deaths.1 Nevertheless, the incidence of acute myocardial infarction (AMI) and death rates after AMI are declining in most countries, especially in the developed ones.2-4 The survivors of AMI are at high risk of developing a recurrent myocardial infarction or other manifestations of cardiovascular disease, such as stroke5- 8. We present the case of a male patient, 80 years old, with a history of inferior myocardial infarction and angioplasty with two barre metal stents on the right coronary artery (2012), who presented an episode of loss of consciousness, followed by motor deficit of the lower limbs and dysarthria. The head CT did not show any acute hemorrhagic lesions, but the patient had elevated myocardial necrosis biomarkers and the ST segment elevation in the inferior leads on the electrocardiography (EKG). He was diagnosed with inferior ST-segment elevation myocardial infarction (STEMI) and transferred to our clinic for further investigations and treatment.
Keywords: myocardial infarction, ST-segment elevation myocardial infarction, thromboaspiration
INTRODUCTION
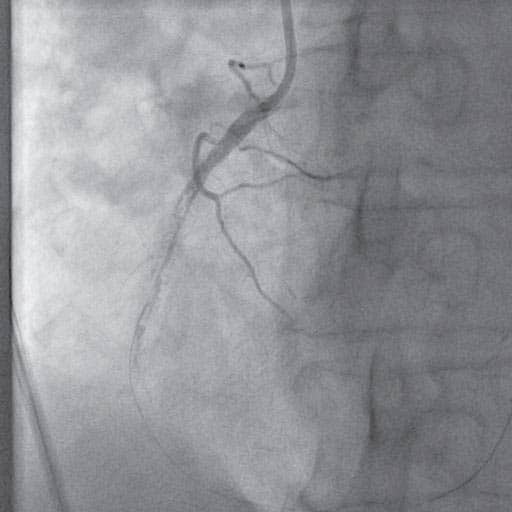
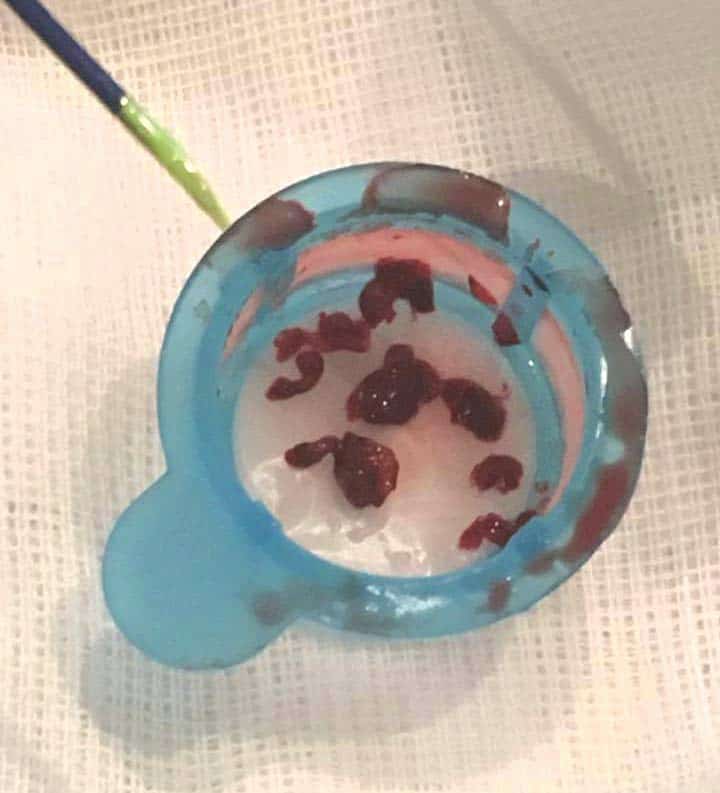
Case report: We present the case of a male patient, 80 years old, hypertensive, dyslipidaemic, with a history of inferior myocardial infarction and angioplasty with 2 BMS on the right coronary artery (2012), who presented an episode of loss of consciousness, followed by motor deficit of the lower limbs and dysarthria. He was admitted to neurology and a head CT scan was performed, this showed no acute hemorrhagic lesions. The myocardial biomarkers were raised and the electrocardiography (EKG) showed ST segment elevation in the inferior leads. The patient was diagnosed with inferior ST-segment elevation myocardial infarction (STEMI) and was referred to our clinic for further investigations and treatment. At admission, the patient accused no angina or dyspnea, but was somnolent and had crural motor defi cit. The myocardial necrosis markers were elevated and the EKG showed persistent ST segment elevation in DII, DIII, aVF with negative T waves and Q waves and ST segment depression in the reciprocal leads. Echocardiography showed a moderately depressed ejection fraction (EF=35%) with akinesia of the inferior wall and apical half of the interventicular septum and a moderate aortic stenosis. The patient underwent urgent coronarography, which revealed right coronary artery (RCA) proximal occlusion and 70% calcified stenosis of the left anterior coronary artery. We decided for emergency percutaneos coronary intervention (PCI) on the right coronary artery. After the occlusion was passed with a hydrophilic guidewire, we predilatated with a semicompliant balloon,but no fl ow was obtained due to the high amount of thrombotic material. We performed multiple thromboaspiration passages, with the extraction of numerous thrombi and vessel repermeabilization was obtained. A long drug eluting stent was implanted with a very good angiographic result, TIMI 3 fl ow to distal RCA. During the hospitalization, the patient’s evolution was unfavorable. He started having episodes of atrial fibrillation and non sustained ventricular tachycardia which were successfully treated with amiodarone. On the third day after admission, the patient became agitated and disoriented; the neurological motor deficit was accentuated. A second CT scan was performed which revealed subacute ischemic stroke in the right posterior junctional territory and a chronic subdural hematoma with a minimal shift of the midline structures contralateral. The patient was transferred to a
stroke unit for specific treatment where he died 48h later.
Figure 1A. Proximal occlusion of RCA.
Figure 1B. RCA – high amount of thrombotic material.
Figure 1C. Final PCI result on RCA.
DISCUSSIONS
World-wide, the most frequent cause of death is coronary artery disease (CAD), responsible, every year, for the death of seven million people, accounting for 12.8% of all deaths1. Twentysix million people worldwide experience a stroke each year, making it the second leading cause of mortality and leading cause of long-term disability. One third of strokes represent intracerebral or subarachnoid hemorrhage, whereas two thirds represent cerebral ischemia9. Acute ischemic stroke in patients with acute coronary syndrome is uncommon, but devastating, it occurs in 1-2% of patients and it is the single, strongest risk factor for inhospital mortality10. Acute MI is a long-established risk factor for ischemic stroke. The association seems causal because overlying areas of akinesia there are often seen trombi9. This could be an explanation for the ischemic stroke our patient developed: he has a moderate depressed left ventricle ejection fraction with area of akinesia. Another explanation could be atrial fibrillation that was documented during his hospitalization. However, there is little information available, on the type of optimal reperfusion therapy and the antithtombotic adjuvant therapy to be applied to patients with STEMI and acute ischemic stroke10. TASTE and TOTAL studies compared routine manual thrombectomy vs PCI alone to STEMI patients who were undergoing primary PC. The results revealed that routine thrombectomy did not reduce the risk of cardiovascular death, recurrent myocardial infraction, cadiogenic shock, but was associated with an increased rate of stroke within 30 days11,12. On the other hand, TAPAS study showed thrombus aspiration is applicable in a large majority of STEMI patients with better results regarding reperfusion and clinic outcomes than conventional PCI13. In our case, we decided to use manual thrombus aspiration, due the high quantity of thombotic material with a good result.
Figure 2. Thrombi removed with aspiration catheter.
Figure 3. Subacute ischemic stroke in the right posterior junctional territory.
CONCLUSION
Manual thromboaspiration with multiple passages is a simple, cheap and high accessibility method to obtain better results regarding the reduction of distal embolization in selected STEMI patients.
Conflict of interest: none declared.
References
1. Steg G, James S, Atar D et. al – ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. European Heart Journal. 2012; (33): 2569-2619.
2. Moran AE, Forouzanfar MH, Roth GA, Mensah GA, Ezzati M, Flaxman A, Murray CJ, Naghavi M. The global burden of ischemic heart disease in 1990 and 2010: the Global Burden of Disease 2010 study. Circulation.2014;129(14):1493–501
3. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, et al. Heart disease and stroke statistics – 2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322.
4. Nichols M, Townsend N, Scarborough P, Rayner M. Cardiovascular disease in Europe 2014: epidemiological update. Eur Heart J. 2014; 35(42):2929.
5. Smolina K, Wright FL, Rayner M, Goldacre MJ. Long-term survival and recurrence after acute myocardial infarction in England, 2004 to 2010. Circ Cardiovasc Qual Outcomes. 2012;5(4):532–40.
6. Witt BJ, Brown Jr RD, Jacobsen SJ, Weston SA, Yawn BP, Roger VL. A community-based study of stroke incidence after myocardial infarction. Ann Intern Med. 2005;143(11):785–92.
7. Campo G, Saia F, Guastaroba P, Marchesini J, Varani E, Manari A, Ottani F, Tondi S, De Palma R, Marzocchi A. Prognostic impact of hospital readmissions after primary percutaneous coronary intervention. Arch Intern Med. 2011;171(21):1948–9
8. Johansson S, Rosengren A, Young K, Jennings E – Mortality and morbidity trends after the first year in survivors of acute myocardial infarction: a systematic review, BMC Cardiovascular Disorders. 2017; 17(1):53.
9. Kamel H, Healey JS – Cardioembolic Stroke. Circulation Research. 2017;120:514-526
10. González-Pacheco H, Méndez-Domínguez A, Vieyra-Herrera G, Azar- Manzur F, Meave-González A, Rodríguez-Zanella H, Martínez-Sánchez C – Reperfusion strategy for simultaneous ST-segment elevation myocardial infarction and acute ischemic stroke within a time window.
11. Sanjit S. Jolly, M.D., John A. et al – The Trial of Routine Aspiration Thrombectomy with PCI versus PCI Alone in Patients with STEMI (TOTAL). The New England Journal Of Medicine 2015; 372:1389-1398.
12. Ole Fröbert, Bo Lagerqvist, Göran K. Olivecrona et al – The Thrombus Aspiration in ST-Elevation Myocardial Infarction in Scandinavia Trial. N Engl J Med 2013; 369:1587-1597.
13. Tone Svilaas, M.D., Pieter J. Vlaar, M.Sc., Iwan C. van der Horst,et al – The Thrombus Aspiration during Percutaneous Coronary Intervention in Acute Myocardial Infarction Study (TAPAS). N Engl J Med 2008; 358:557-567.



 This work is licensed under a
This work is licensed under a