Frans Van de Verf
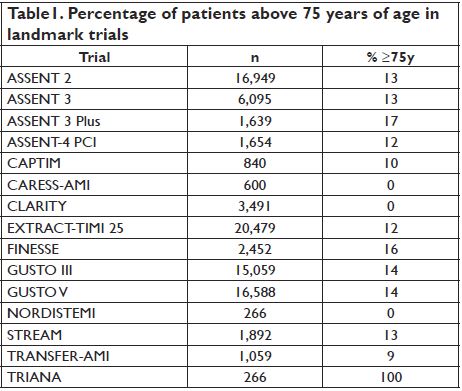
The clinical trial evidence for efficacy of fibrinolysis in the elderly is limited. There are no dedicated adequately sized fibrinolytic trials in the elderly, and patients aged 75 years or higher are under-represented in the landmark trials (Table )1. However, on aggregate, there appeared to be little to no heterogeneity in efficacy relating to age in the large fibrinolytic trials. There are no pathophysiological reasons to doubt the efficacy of fibrinolysis in older patients, and sub-analyses from landmark trials have suggested that the mortality benefit associated with fibrinolytic therapy is preserved in the elderly2. The Fibrinolytic Therapy Trialists’ meta-analysis from 1994 (with a re-analysis in 2000) reported an absolute mortality reduction in patients aged between 65 and 75 years, and over 75 years, that was significantly greater than that in patients aged <55 years (34 and 40 vs. 16 lives saved per 1000 treated, respectively) 3,4. Data from the GISSI-1 study also suggest that the largest absolute benefit occurs in elderly patients, due to their higher baseline risk5. Hence, there is reason for optimism that an appropriately designed trial of adequate size would provide much needed evidence to address this unmet need in elderly STEMI patients not able to undergo timely pPCI.
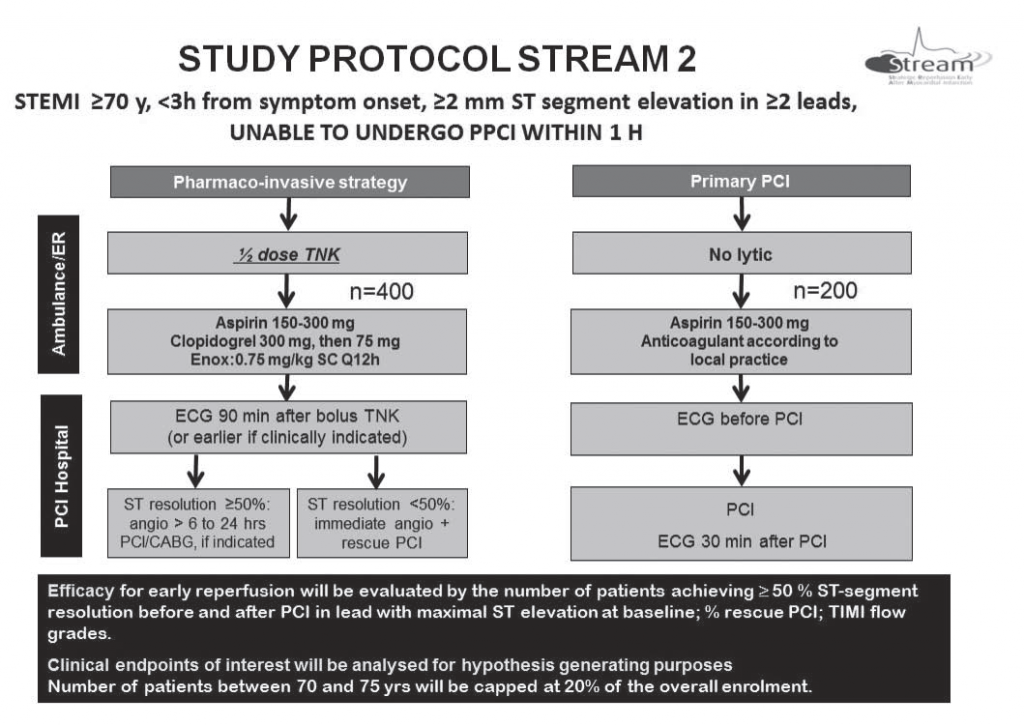
Not well known is that a loading dose of clopidogrel (300 or 600 mg) has not been studied as an adjunct to fibrinolysis in patients above 75 years of age. Also few studies have compared fibrinolysis with pPCI in the elderly. In the unpublished SENIOR PAMI (Primary Angioplasty in Myocardial Infarction) trial conducted over a decade ago, primary PCI was not found to be superior to fibrinolysis in 481 elderly STEMI patients (aged >70 years) randomized up to 12 h after symptom onset6. However, in a small Dutch study in 87 elderly STEMI patients aged 75 years randomized up to 24 h after symptom onset, pPCI was associated with a significantly lower 2-year mortality than the non-fibrin-specific agent streptokinase (7 vs. 13 deaths; p = 0.04)7. More recently, 266 STEMI patients aged 75 years or higher presenting within 6 h of symptom onset were randomized to pPCI or thrombolysis in the Spanish TRIANA (TRatamiento del Infarto Agudo de miocardio eN Ancianos) trial8. All fibrinolytic-treated patients received standard weight-adjusted tenecteplase, unfractionated heparin (UFH) [60 IU/kg bolus (max 4000 IU) followed by a 12-IU/kg/h infusion] and clopidogrel (75 mg once daily without loading dose). Although the trial was underpowered and was prematurely stopped due to slow enrollment, there was no difference in the primary 30-day combined endpoint between the two arms. The TRIANA study group undertook a combined analysis of their trial as well as the two aforementioned trials (n = 834 patients overall); this showed no difference in 30-day mortality but a significant lower risk with pPCI in elderly STEMI patients in the composite endpoint of death, re-infarction, and disabling stroke up to 30 days (odds ratio 0.64, 95% confidence interval 0.45–0.91). However, given the small sample size, somewhat dated conduct of the initial two studies, wide randomization windows, and suboptimal fibrinolytic choices, this result cannot be considered definitive. In STREAM 19 a pharmaco-invasive strategy has been shown to be at least as good as primary PCI in patients presenting <3 hours after symptom onset who could not get the invasive intervention within 1 hour after first medical contact. Physicians, however, are reluctant to offer a pharmaco-invasive strategy to elderly patients because of the risk of intracranial hemorrhage. In the STREAM 1 study high rates intracranial bleeding in the elderly were observed with full dose lytic therapy. After halving
the dose of tenecteplase, no new intracranial bleedings were observed and efficacy for reperfusion was similar to the total population . Only 96 elderly patients were treated with half dose tenecteplase in STREAM 1. In the planned STREAM 2 study 600 patients 70 years of age or older with the same baseline characteristics as in STREAM 1 will be randomized between primary PCI and a pharmaco-invasive approach with half-dose tenecteplase and 300 mg clopidogrel (Figure). Romania with its network of ambulance will be a key partner in this study.
Conflict of interest: none declared.
References
1. Koeth O, Zahn R, Gitt AK, Bauer T, Juenger C, Senges J, Zeymer U. Clinical benefit of early reperfusion therapy in patients with STelevation myocardial infarction usually excluded from randomized clinical trials (results from the Maximal Individual Therapy in Acute Myocardial Infarction Plus [MITRA Plus] registry). Am J Cardiol 2009;104(8):1074-7.
2. White HD, Barbash GI, Califf RM, Simes RJ, Granger CB, Weaver WD, Kleiman NS, Aylward PE, Gore JM, Vahanian A, Lee KL, Ross AM, Topol EJ. Age and outcome with contemporary thrombolytic therapy. Results from the GUSTO-I trial. Global Utilization of Streptokinase and TPA for Occluded coronary arteries trial. Circulation 1996;94(8):1826.
3. White HD. Thrombolytic therapy in the elderly. Lancet 2000; 356(9247):2028.
4. Indications for fi brinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Fibrinolytic Therapy Trialists’ (FTT) Collaborative Group. Lancet 1994;343(8893):311.
5. Sherry S, Marder VJ. Mistaken guidelines for thrombolytic therapy of acute myocardial infarction in the elderly. J Am Coll Cardiol 1991; 17(5):1237.
6. Grines C. SENIOR PAMI: a prospective randomized trial of primary angioplasty and thrombolytic therapy in elderly patients with acute myocardial infarction. Presented at: Transcatheter Cardiovascular Therapeutics 2005; October 19, 2005; Washington, DC. 2005.
7. de Boer MJ, Ottervanger JP, van’t Hof AW, Hoorntje JC, Suryapranata H, Zijlstra F. Reperfusion therapy in elderly patients with acute myocardial infarction: a randomized comparison of primary angioplasty and thrombolytic therapy. J Am Coll Cardiol 2002;39(11):1723.
8. Bueno H, Betriu A, Heras M, Alonso JJ, Cequier A, Garcia EJ, Lopez-Sendon JL, Macaya C, Hernandez-Antolin R. Primary angioplasty vs. fibrinolysis in very old patients with acute myocardial infarction: TRIANA (TRatamiento del Infarto Agudo de miocardio eN Ancianos) randomized trial and pooled analysis with previous studies. Eur Heart J 2011;32(1):51-60.
9. Armstrong PW, Gershlick AH, Goldstein P, Wilcox R, Danays T, Lambert Y, Sulimov V, Rosell Ortiz F, Ostojic M, Welsh RC, Carvalho AC, Nanas J, Arntz HR, Halvorsen S, Huber K, Grajek S, Fresco C, Bluhmki E, Regelin A, Vandenberghe K, Bogaerts K, Van de Werf F; STREAM Investigative Team. Fibrinolysis or primary PCI in ST-segment elevation myocardial infarction. N Engl J Med. 2013;368(15):1379-87.
 This work is licensed under a
This work is licensed under a