Razvan Constantin Serban1,2, Laszlo Hadadi1,2, Ioana Sus1,2, Eva Katalin Lakatos1,2, Zoltan Demjen2, Irina Pintilie2, Alina Scridon1
1 University of Medicine and Pharmacy of Tirgu Mures, Romania
2 Emergency Institute for Cardiovascular Diseases and Transplantation Tirgu Mures, Romania
Abstract: Objectives – The impact of obesity in patients with ST-segment elevation myocardial infarction (STEMI) remains controversial. We sought to investigate the impact of body mass index (BMI) on various key features of STEMI patients. Methods – A total of 322 STEMI patients were retrospectively evaluated. Demographic, clinical, hemodynamic, electrocardiographic, and laboratory data at presentation, angiographic data and percutaneous coronary intervention-related complications, and parameters characterizing the in-hospital evolution of STEMI patients were stratified by BMI values. Results – Over three quarters (76.7%) of STEMI patients were overweight or obese. Obese patients were more often hypertensives and diabetics (both p<0.001), presented more often hypertriglyceridemia (p<0.001), but were less likely to be active smokers (p=0.02). Increased BMI did not influence in-hospital mortality rates or STEMI-related complications. However, obese patients presented significantly lower sum of ST-segment elevation (p<0.01) and maximum ST-segment elevation (p=0.03), and were less likely to present anterior STEMI. Conclusions – Obese patients displayed lower maximum ST-segment elevation and sum of ST-segment elevation, and were less likely to present anterior STEMI. These features may act to compensate the intrinsic obesity-related cardiovascular risk of these patients, explaining the lack of increased mortality in this group. Keywords: ST-segment elevation myocardial infarction; body mass index; obesity paradox.
Rezumat: Obiective – Impactul obezităţii asupra pacienţilor cu infarct miocardic cu supradenivelare de segment ST (STEMI) rămâne controversat. Ne-am propus să evaluăm impactul indicelui de masă corporală (IMC) asupra unor caracteristici cheie ale pacienţilor cu STEMI. Metode – Un total de 322 de pacienţi cu STEMI au fost evaluaţi retrospectiv. Datele demografice, clinice, hemodinamice, electrocardiografice şi de laborator la prezentare, datele angiografice şi cele legate de complicaţiile angioplastiei coronariene şi diferiţi parametri ce caracterizează evoluţia intraspitalicească a pacienţilor cu STEMI au fost stratificaţi pe baza IMC. Rezultate – Peste trei sferturi (76,7%) din pacienţii cu STEMI au fost supraponderali sau obezi. Pacienţii obezi au fost mai frecvent hipertensivi şi diabetici (p<0,001), cu hipertrigliceridemie (p<0,001), dar mai puţin fumători activi (p=0,02). IMC nu a influenţat mortalitatea sau alte complicaţii legate de STEMI. Pacienţii obezi au prezentat însă valori mai mici ale sumei supradenivelării (p<0,01) şi ale supradenivelării maxime de segment ST (p=0,03) şi au prezentat mai rar STEMI anterior. Concluzii – Pacienţii obezi au prezentat supradenivelare maximă şi suma supradenivelării de segment ST mai mici şi s-au prezentat mai rar cu STEMI anterior. Aceste caracteristici ar putea compensa riscul cardiovascular intrinsec legat de obezitate, explicând lipsa unor rate crescute de mortalitate la aceşti pacienţi.
Cuvinte cheie: infarct miocardic cu supradenivelare de segment ST, indice de masă corporală, paradoxul obezităţii.
BACKGROUND
Overweight and obesity have become worldwide public health issues. According to the World Health Organization (WHO) estimates, 30% to 70% of both men and women in Europe are overweight and 10% to 30% are obese1. Large epidemiological studies have linked increased BMI with increased risk of cardiovascular diseases,2 including acute ST-segment elevation myocardial infarction (MI) (STEMI)3. In addition, long-term studies provided evidence that obesity is associated with increased mortality in the general population4. However, a paradoxical trend has been described in patients with already established cardiac disease5, indicating that obese patients with heart failure may actually have improved prognosis6. This feature, known as the obesity paradox, has also been reported in several other settings, including in patients with acute coronary syndromes7,8. Taken together, these data suggest that, whereas obesity is a major risk factor for coronary artery disease (CAD), once CAD is established in these patients, being overweight or obese may actually be protective against cardiovascular mortality. Nevertheless, there is no broad consensus concerning the obesity paradox, as a number of studies were unable to support this hypothesis9-11. Furthermore, in the vast majority of studies that support the obesity paradox, BMI did not remain an independent predictor of survival in multivariate analysis, but the improved outcomes seen in obese patients were related to their younger age or better kidney function12. Thus, the obesity-prognosis relationship in STEMI patients remains controversial. Additionally, while most studies focused on the link between obesity and shortor long-term prognosis in CAD patients, the way in which the BMI influences the presentation and the features of MI in STEMI patients has not been approached extensively. In the present study, we examined the association between BMI and a number of key clinical, hemodynamic, ECG, angiographic, and prognosis data in STEMI patients.
MATERIALS AND METHODS
Study population
 Consecutive patients that beneficiated of primary percutaneous coronary intervention (PCI) for STEMI in our center between January 2011 and December 2013 were included in this analysis. The research protocol complied with the Declaration of Helsinki and was approved by the local Ethics Committee. Eligibility criteria required patients to be aged 18 years or older, have spontaneous (type I) STEMI according to the Third universal definition of myocardial infarction guideline of the European Society of Cardiology (ESC)13, and beneficiate of primary PCI for STEMI within the first 12h after symptoms onset or 12h to 24h after symptoms onset if they presented evidence of ongoing ischemia. Patients were excluded from the study if thrombolytic treatment was administered prior to PCI, if they presented left bundle branch block or paced rhythm, making it difficult to assess STEMIrelated ECG parameters, or if they have had a history of coronary artery by-pass surgery. Medical treatment of all patients included in the present study complied with the ESC guidelines on the management of acute STEMI.
Consecutive patients that beneficiated of primary percutaneous coronary intervention (PCI) for STEMI in our center between January 2011 and December 2013 were included in this analysis. The research protocol complied with the Declaration of Helsinki and was approved by the local Ethics Committee. Eligibility criteria required patients to be aged 18 years or older, have spontaneous (type I) STEMI according to the Third universal definition of myocardial infarction guideline of the European Society of Cardiology (ESC)13, and beneficiate of primary PCI for STEMI within the first 12h after symptoms onset or 12h to 24h after symptoms onset if they presented evidence of ongoing ischemia. Patients were excluded from the study if thrombolytic treatment was administered prior to PCI, if they presented left bundle branch block or paced rhythm, making it difficult to assess STEMIrelated ECG parameters, or if they have had a history of coronary artery by-pass surgery. Medical treatment of all patients included in the present study complied with the ESC guidelines on the management of acute STEMI.
Body mass index
Body mass index values were calculated based on patients’ weight and height at admission, as recorded in the medical files. For the analysis, patients were classified into four groups, according to the WHO recommendations14: underweight (BMI < 18.50 kg/m2), normal weight (BMI: 18.5-24.9 kg/m2), overweight (BMI: 25.0-29.9 kg/m2), and obese (BMI ≥30.0 kg/m2).
Clinical evaluation and outcomes
For every patient included in the study, the age, gender, medical (smoking status, arterial hypertension, diabetes mellitus, heart failure, chronic kidney disease, previous MI) and treatment (beta-blockers, calcium channel blockers, antiarrhythmics, antialdosteronics, angiotensin converting enzyme inhibitors and/or angiotensin II receptor blockers, statins) history were recorded. Clinical (presence of angina and Killip class), hemodynamic (systolic, diastolic, and mean blood pressure, heart rate, and left ventricular ejection fraction), ECG (number of ECG leads with ST-segment elevation, maximum ST-segment elevation, sum of ST-segment elevation, ECG localization of STEMI, presence of rhythm or conduction disorders), and blood parameters (complete blood count, glycaemia, lipid profile, myocardial enzymes, creatinine) at hospital admission were also assessed. Chronic kidney disease was defined as an estimated glomerular filtration rate < 60 ml/ min/1.73 m2 using the Cockroft-Gault equation. Left ventricular ejection fraction was determined by echocardiography at hospital admission. Rhythm disorders included atrial and ventricular extrasystoles, tachycardia and/or fibrillation, and various combinations of these rhythm disorders. Conduction disorders included atrioventricular blocks, right bundle branch block, and various combinations of these cardiac conduction disorders. Angiographic data (preand post-PCI Thrombolysis in Myocardial Infarction (TIMI) flow, number of diseased vessels, left main disease, and chronic total occlusion) and PCI-related complications (iatrogenic coronary artery dissection, coronary perforation, angiographic no-reflow, angiographically visible distal embolization, and acute intra-PCI occlusion) were also recorded. Additionally, traditional clinical (Primary Angioplasty in Myocardial Infarction (PAMI), Global Registry of Acute Coronary Events (GRACE), modified Age, Creatinine, and Ejection Fraction (ACEFm)), angiographic (SYNergy between PCI with TAXUSTM and Cardiac Surgery (SYNTAX)) and combined (clinical SYNTAX) risk scores, previously validated in STEMI patients, were also evaluated. A number of parameters that characterize the in-hospital evolution of STEMI patients were also assessed reinfarction, cardiogenic shock, heart failure, asystole, conduction disorders, emergency cardiac pacing, cardiac arrhythmias, sudden cardiac death, kidney and liver dysfunction, echocardiographic left ventricular ejection fraction at discharge, length of hospital stay, and all-cause mortality.
Statistics
Continuous variables are presented as mean values ± standard deviation or median and range, as appropriate. Categorical data are summarized using frequencies and percentages. The Chi-square test was used for comparison of categorical data and one-way analysis of variance (ANOVA) or Kruskal-Wallis test (non-parametric ANOVA) were applied for comparison of continuous variables between the predefined BMI groups. Correlations between BMI and clinical, hemodynamic, ECG, laboratory, and angiographic data were ascertained using Spearman’s rank correlation test. Stepwise multiple regression analysis was used to identify independent predictors of clinical and angiographic complications. Statistical adjustment included demographic and clinical factors that differed in prevalence between the predefined BMI groups. Receiver operating characteristics (ROC) analysis was used to identify BMI cutoff values and BMI sensitivity and specificity for predicting various complications. All tests were two-sided and a p-value of less than 0.05 was considered statistically significant. All data were computed using MedCalc for Windows, version 12.4.3.0 (MedCalc Software, Ostend, Belgium).
RESULTS
Baseline characteristics
A total of 428 patients were initially screened for inclusion in the study. Patients for whom BMI data (n=102) were not available were excluded from the study. Only 4 patients (1.2% of the cohort study) were underweight. Because of the small number of patients falling in this latter category, which would have led to limited statistical power in this group, all analyses were restricted to normal weight, overweight, and obese patients. This left a total of 322 patients eligible for the analyses (68% males), with a mean age of 62.4 ± 11.5 years.
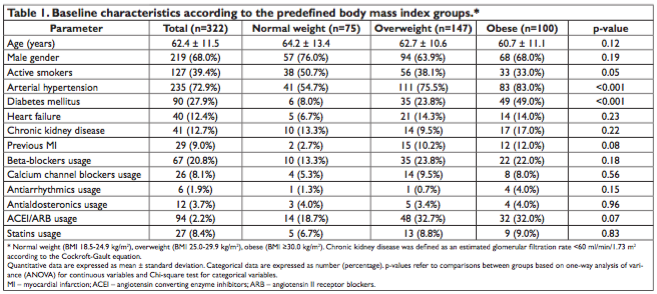
The mean BMI in the total population was 28.5 ± 4.6 kg/m2. According to the predefined BMI categories, 75 (23.3%) patients had normal weight, 147 (45.7%) were overweight, and 100 (31.0%) were obese. The baseline characteristics of the predefined BMI groups are listed in Table 1. Unsurprisingly, obese patients were more often hypertensives and diabetics (both p<0.001). Obese patients also tended to be younger (p=0.05), were less likely to be active smokers (p=0.02), and were more likely to have experienced a previous MI (p=0.03) than normal weight patients. Meanwhile, patients’ gender and medical history, including heart failure and chronic kidney disease, were not significantly different among the three groups (all p>0.05).
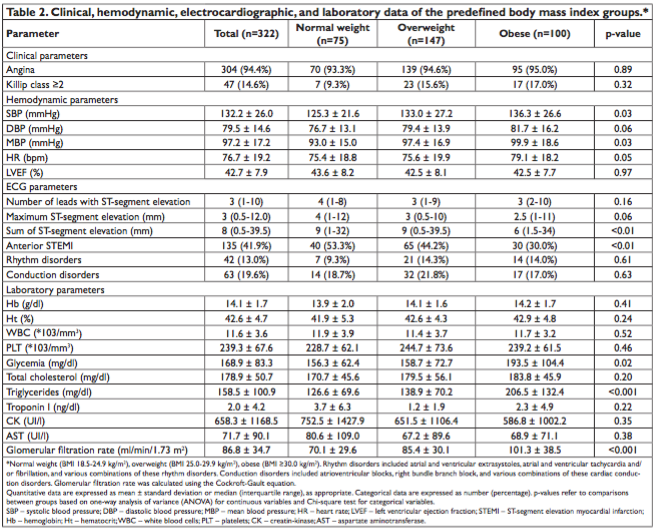
Clinical, hemodynamic, electrocardiographic, and laboratory data at presentation
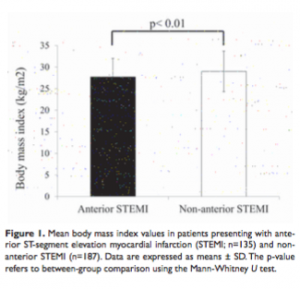
Clinical, hemodynamic, ECG, and laboratory data of the studied groups at presentation to the Emergency Department are listed in Table 2. Unsurprisingly, patients with higher BMI values also presented higher glycemic levels (p=0.02), higher triglycerides (p<0.001), and higher glomerular filtration rate (p<0.001) than patients with lower BMIs. In the same vein, BMI values significantly positively correlated with systolic (r=0.15, p<0.01), diastolic (r=0.16, p<0.01), and mean (r=0.17, p<0.01) blood pressure, and with the heart rate (r=0. 13, p=0. 02), as well as with glycemic (r=0. 18, p<0. 001), total cholesterol (r=0. 18, p<0. 01), triglycerides (r=0.34, p<0.001) levels, and with the glomerular filtration rate (r=0.38, p<0.001). A significant negative correlation was observed between BMI values and the occurrence of anterior STEMI (r=-0.15, p<0.01). Mean BMI was significantly lower (p<0.01) in patients presenting with anterior STEMI (27.7±4.3 kg/m2) than in patients presenting with non-anterior STEMI (29.0±4.7 kg/m2) (Fig. 1). Additionally, the sum of ST-segment elevation was significantly different among the three groups (p<0.01).
Compared to obese patients, normal weight patients presented significantly higher sum of ST-segment elevation (p<0.01) and higher maximum ST-segment elevation (p=0.03). When all patients were considered together, BMI values significantly negatively correlated with maximum ST-segment elevation (r=-0.14, p=0.01), as well as with the sum of ST-segment elevation (r=0.16, p<0.01). However, when maximum ST-segment elevation and the sum of ST-segment elevation were compared between patients with anterior versus non-anterior STEMI, the former group presented significantly higher values for both parameters: 4.0 mm (1.0-12.0 mm) versus 2.5 mm (0.5-8.5 mm) for maximum ST-segment elevation (p<0.001); 8.0 mm (1.539.5 mm) versus 6.25 mm (0.5-34 mm) for the sum of ST-segment elevation (p=0.01). After adjusting for hypertension, diabetes mellitus, blood pressure, glycaemia and triglycerides levels, the association between BMI and ST-segment elevation and the sum of ST-segment elevation was no longer significant. However, in multiple regression analysis, lower BMI remained an independent predictor of anterior STEMI (r=-0.16, p=0.04). ROC analysis identified a BMI ≤26.26 kg/m2 as a strong predictor of anterior STEMI (OR 1.78, 95%CI 1.13-2.79, p=0.01), with a sensitivity of 49.6% and a specificity of 68.2%.
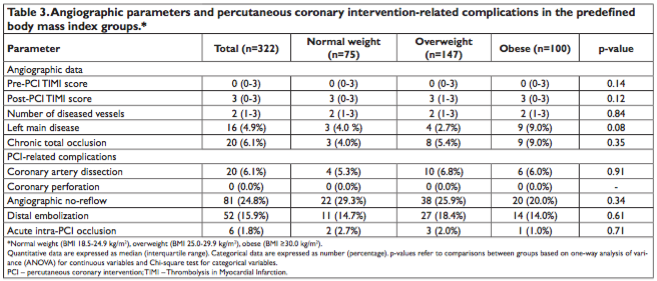
Angiographic data and percutaneous coronary intervention-related complications
As showed in Table 3, there was no significant difference between the three BMI groups for any of the angiographic parameters or PCI-related complications. However, patients presenting chronic total occlusion tended to have higher BMI values compared to those without (30.4±5.5 kg/m2 versus 28.4±4.5 kg/m2, p=0.07).
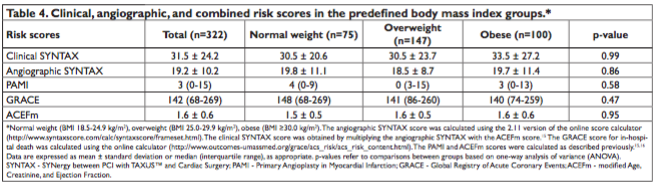
Clinical, angiographic, and combined risk scores
Clinical, angiographic, and combined risk scores in the studied groups are listed in Table 4. There were not significant differences between the three BMI groups concerning any of the studied scores (all p>0.05).
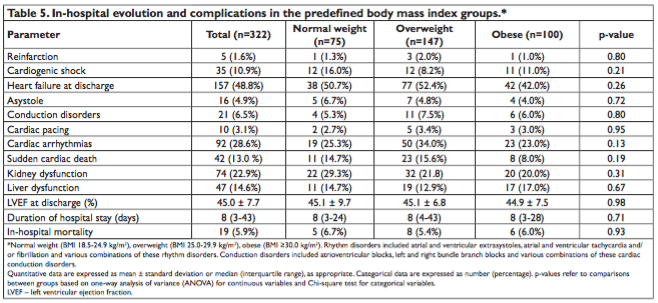
In-hospital evolution and complications
Data regarding the in-hospital evolution and complications in the studied groups are listed in Table 5. None of the studied parameters, including in-hospital mortality rates, were significantly different between the three BMI groups (all p>0.05). Also, there was no significant correlation between BMI values and any of these parameters (all p>0.05).
DISCUSSIONS
The main findings of the present study are that (1) based on the current WHO standards, more than 75% of patients undergoing primary PCI for STEMI were overweight or obese; (2) increased BMI did not influence in-hospital mortality rates, nor acute STEMIrelated complications; (3) patients with higher BMIs presented lower maximum ST-segment elevation and sum of ST-segment elevation; and (4) were less likely to develop anterior STEMI. With their rising prevalence, overweight and obesity have become a worldwide public health issue, affecting more than half of the adult population of the U.S.A.17. The presence of obesity has been associated with hyperinsulinemia, sympathetic overactivity, increased triglycerides, cholesterol, and insulin resistance, explaining the high rates of diabetes mellitus, arterial hypertension, CAD, heart failure or stroke in this population2,18,19. Moreover, plaque rupture and acute coronary syndromes, including STEMI, occur more often in obese patients than in their normal weight peers2,20,21. Thus, it is not surprising that in the present study, patients with weights above the normal range represented more than three quarters of patients beneficiating of primary PCI for STEMI, and that obese patients were more likely to have experienced a previous MI. Also it is not surprising that patients with higher BMIs were more likely to be hypertensives and diabetics, and tended to be younger than their normal weight counterparts. However, contrary to previous studies, complete occlusions were not more common in patients with higher BMIs20, and also there was no significant difference in the burden of coronary atherosclerosis, as quantified by the angiographic SYNTAX score.
Despite the strong association between obesity and cardiovascular risk in the general population, a multitude of studies suggested that, similarly to what has been observed in patients with heart failure or endstage renal disease on maintenance hemodialysis22,23, the clinical outcomes after acute cardiovascular events may actually be more favorable in patients with higher BMIs, including in those presenting with an acute MI24,25. This obesity paradox however, does not seem to be supported by all studies9. Whereas some studies reported better outcomes in patients with increased weight, others did not find any association. In a follow-up study of the Controlled Abciximab and Device Investigation to Lower Late Angioplasty Complications (CADILLAC) trial, although lower in-hospital, 30-days, and 1-year mortality rates were observed in obese patients with acute MI undergoing primary PCI, statistical significance was only reached in male patients12. Lower in-hospital mortality and major adverse cardiac events in obese than in normal weight patients have also been reported in a study based on the New York State Coronary Angioplasty Reporting System26. However, in that study, mortality rates were significantly higher in extremely than in less obese patients26. In other two large population-based studies, although mortality rates were lower in higher weight patients, this was due to lower non-cardiac deaths, whereas higher BMI patients experienced more recurrent coronary events10,27. In fact, even in the studies that did report an inverse relationship between BMI and mortality, after adjusting for age, gender, kidney dysfunction, or N-terminal probrain natriuretic peptide values, BMI was no longer predictive of mortality after STEMI20,28, suggesting that comorbidities may actually play a more important role in these patients’ outcomes. In line with these latter studies, obese patients included in our study did not present either more or less frequently with any adverse cardiac event, such as reinfarction, cardiogenic shock, rhythm or conduction disorders, or in-hospital mortality. Furthermore, there was no significant correlation between BMI values and any of the traditional risk scores validated in patients with STEMI. It is of note, however, that GRACE scores were significantly higher in the present study compared to previous studies29, suggesting that the BMI may be relevant only in patients with less severe clinical presentation. One important observation is that whereas most studies supporting the obesity paradox are large-scale studies, this relationship is not supported by the vast majority of small, single-center studies, suggesting that, even if present, this inverse BMI-survival association is probably modest. Nevertheless, all studies, including the present one, appear to agree on the fact that, contrary to what is accepted for the general population, increased BMI does not translate into increased risk of adverse cardiac events following acute STEMI. Several hypotheses have been set forth to explain this finding. In most studies, including the present one, obese patients presenting with STEMI had younger age and were less likely to be smokers, both of which may impact on their better prognosis30-32. Studies have also suggested that obese patients are more likely to be treated earlier, more aggressively, with guideline-recommended therapies33. However, in the present study, despite the higher incidence of arterial hypertension, diabetes mellitus, and hypertriglyceridemia among patients with higher BMI values, the likelihood of being treated with therapies that may influence prognosis, including beta-blockers, renin-angiotensin-aldosterone system blockers, or statins34, was similar among the different BMI groups. One other potential explanation was that obese patients could present earlier in the evolution of acute MI, due to their increased awareness of cardiovascular risk29. However, in the present study, the symptom onset-to-cardiac catheterization laboratory time intervals were similar between the different BMI groups (5.7±4.4 h in normal weight patients versus 6.6±4.8 h in overweight patients versus 6.6±4.4 h in obese patients, p=0.16). It has also been suggested that obese patients may have less severe left ventricular dysfunction at presentation35. This was again not the case in the present study, as there was no significant difference in left ventricular ejection fraction at presentation between the different BMI groups. From a pathophysiological point of view, it has been suggested that patients with high BMI values may have greater metabolic reserve, and better neurohormonal profile, as demonstrated by the lower B-type natriuretic peptide levels observed in previous studies36. Finally, obese patients appear to be less likely to develop acute complications such as hemorrhagic events and anemia, which may also impact on their better prognosis37. In the present study, despite a greater incidence of arterial hypertension, diabetes mellitus, and hypertriglyceridemia in the obese patients, in-hospital mortality rates were not different between the different BMI groups. However, obese patients displayed lower maximum ST-segment elevation and sum of ST-segment elevation, and were less likely to present anterior STEMI, all features known to affect prognosis in acute MI38. After adjusting for potential confounders, however, BMI no longer predicted the sum of ST-segment elevation values or maximum ST-segment elevation. As indicated by the higher values of these parameters in patients with anterior versus non-anterior STEMI, the decreased values of these parameters in obese patients may have been related to their lower likelihood of presenting anterior STEMI. Additionally, the increased thickness of the subcutaneous tissue in obese patients may also have contributed to this finding, lowering ECG voltage. Contrarily, in multiple regression analysis, lower BMI remained an independent predictor of anterior STEMI. A lower incidence of infarctions involving the left anterior descending coronary artery in obese patients has also been reported in a follow-up study of the CADILLAC trial involving over 2.000 patients12. These features may act to compensate the intrinsic obesity-related cardiovascular risk of these patients, explaining the lack of increased mortality in this pa-tient group. The mechanisms explaining the increased likelihood of obese patients to develop non-anterior STEMI remain to be elucidated. Additional insights into the BMI-mortality relationship in STEMI patients will probably arise from studies that will accurately quantify body composition and fat distribution.
Potential limitations
Several potential limitations apply to this study. First, the relatively low number of patients included in the analysis may have affected the study’s statistical power. Secondly, our analysis has all the limitations of a retrospective analysis and should thus be viewed as hypothesis-generating rather than definitive. Finally, data on waist circumference and waist-to-hip ratio were unavailable and more direct adiposity quantification by computed tomography or dual-energy x-ray absorptiometry was not performed in the present study. Although the BMI is a validated marker of adiposity and the most widely used marker in clinical practice, it may also reflect muscle mass, which makes it an imperfect measure of body adiposity, whereas other markers, such as the waist circumference and/or the waist-to-hip ratio may be better markers of CAD39. However, the vast majority of studies assessing the obesity paradox have used almost exclusively the BMI as an index of obesity.
CONCLUSIONS
In the present study, patients with weights above the normal range represented more than three quarters of patients undergoing primary PCI for STEMI. Although the obesity paradox was not confirmed in the present study, increased BMI did not translate into increased risk following acute STEMI. On the contrary, obese patients were less likely to present anterior STEMI and displayed lower maximum ST-segment elevation and sum of ST-segment elevation. These features may act to compensate the intrinsic obesity-related cardiovascular risk of these patients, explaining the lack of increased mortality in this patient group.
Acknowledgement: This work was supported by the University of Medicine and Pharmacy of Tîrgu Mureş Research Grant number 17800/1/22.12.2015. Conflict of interes: none declared.
References
1. http: //www. euro. who. int/en/health-topics/noncommunicable-diseases/obesity/data-and-statistics; accessed on April, 9th, 2016.
2. Wilson PW, D’Agostino RB, Sullivan L, Parise H, Kannel WB. Overweight and obesity as determinants of cardiovascular risk: the Framingham experience. Arch Intern Med 2002;162: 1867-72.
3. Borgeraas H, Hertel JK, Svingen GF, Seifert R, Pedersen EK, SchartumHansen H, Hjelmesæth J, Nygård O. Association of body mass index with risk of acute myocardial infarction and mortality in Norwegian male and female patients with suspected stable angina pectoris: a prospective cohort study. BMC Cardiovasc Disord 2014;14: 68.
4. Peeters A, Barendregt JJ, Willekens F, Mackenbach JP, Al Mamun A, Bonneux L. Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann Intern Med 2003;138: 24-32.
5. Iancu M, Şerban M, Copăescu C, Ginghină C. Structural and functional ventriculo-arterial changes in obesity: mechanisms, implications and reversibility after weight loss. Romanian Journal of Cardiology 2013;23(1): 37-43.
6. Morse SA, Gulati R, Reisin E. The obesity paradox and cardiovascular disease. Curr Hypertens Rep 2010;12(2): 120-6.
7. Dhoot J, Tariq S, Erande A, Amin A, Patel P, Malik S. Effect of morbid obesity on in-hospital mortality and coronary revascularization outcomes after acute myocardial infarction in the United States. Am J Cardiol 2013;111: 1104-10.
8. Buettner HJ, Mueller C, Gick M, Ferenc M, Allgeier J, Comberg T, Werner KD, Schindler C, Neumann FJ. The impact of obesity on mortality in UA/non-ST-segment elevation myocardial infarction. Eur Heart J 2007;28: 1694-701.
9. Chrysant SG, Chrysant GS. New insights into the true nature of the obesity paradox and the lower cardiovascular risk. J Am Soc Hypertens 2013;7(1): 85-94.
10. Kaplan RC, Heckbert SR, Furberg CD, Psaty BM. Predictors of subsequent coronary events, stroke, and death among survivors of first hospitalized myocardial infarction. J Clin Epidemiol 2002;55: 654-64.
11. Călin C, Pătru C, Deleanu D, Ulmeanu V, Ginghină C. Clinical and angiographic correlates of left ventricular aneurysm formation in patients with myocardial infarction. Romanian Journal of Cardiology 2012;22(4): 279-84.
12. Nikolsky E, Stone GW, Grines CL, Cox DA, Garcia E, Tcheng JE, Griffin JJ, Guagliumi G, Stuckey T, Turco M, Negoita M, Lansky AJ, Mehran R. Impact of body mass index on outcomes after primary angioplasty in acute myocardial infarction. Am Heart J 2006;151(1): 168-75.
13. Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD: the Writing Group on behalf of the Joint ESC/ACCF/AHA/WHF Task Force for the Universal Definition of Myocardial Infarction. Third universal definition of myocardial infarction. Eur Heart J 2012;33: 255167.
14. Ferro-Luzzi A, Garza C, Haas J, Habicht JP, Himes J, Pradilla A, Raman L, Ransome-Kuti O, Seidell JC, Victoria C, Wahlqvist ML, Yip R. Physical status: the use interpretation of anthropometry: report of a WHO Expert Committee. WHO Tech Rep Ser 1995;854: 1-452.
15. Garg S, Sarno G, Garcia-Garcia HM, Girasis C, Wykrzykowska J, Dawkins KD, Serruys PW; ARTS-II Investigators. A new tool for the risk stratification of patients with complex coronary artery disease: the Clinical SYNTAX Score. Circ Cardiovasc Interv 2010;3: 317-26.
16. Addala S, Grines CL, Dixon SR, Stone GW, Boura JA, Ochoa AB, Pellizzon G, O’Neill WW, Kahn JK. Predicting mortality in patients with ST-elevation myocardial infarction treated with primary percutaneous coronary intervention (PAMI risk score). Am J Cardiol 2004;93: 629-32.
17. Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999-2000. JAMA 2002;288: 1723-7.
18. Klein S, Burke LE, Bray GA, Blair S, Allison DB, Pi-Sunyer X, Hong Y, Eckel RH. Clinical implications of obesity with specific focus on cardiovascular disease. A statement for professionals from the American Heart Association Council on nutrition, physical activity, and metabolism. Circulation 2004;110: 2952-67.
19. Wolk R, Berger P, Lennon RJ, Brilakis ES, Somers VK. Body mass index: a risk factor for unstable angina and myocardial infarction in patients with angiographically confirmed coronary artery disease. Circulation 2003;108: 2206-11.
20. Herrmann J, Gersh BJ, Goldfinger JZ, Witzenbichler B, Guagliumi G, Dudek D, Kornowski R, Brener SJ, Parise H, Fahy M, McAndrew TC, Stone GW, Mehran R. Body mass index and acute and long-term outcomes after acute myocardial infarction (from the Harmonizing Outcomes With Revascularization and Stents in Acute Myocardial Infarction Trial). Am J Cardiol 2014;114(1): 9-16.
21. Eckel RH, York DA, Roessner S, Hubbard V, Caterson I, StJeor ST,
Hayman LL, Mullis RM, Blair SN. Prevention conference VII. Obesity, a worldwide epidemic related to heart disease and stroke. Executive summary. Circulation 2004;110: 2968-75.
22. Kalantar-Zadeh K, Block G, Horwich T, Fonarow GC. Reverse epidemiology of conventional cardiovascular risk factors in patients with chronic heart failure. J Am Coll Cardiol 2004;43: 1439-44.
23. Horwich TB, Fonarow GC. Reverse epidemiology beyond dialysis patients: chronic heart failure, geriatrics, rheumatoid arthritis, COPD, and AIDS. Semin Dial 2007;20: 549-53.
24. Romero-Corral A, Montori VM, Somers VK, Korinek J, Thomas RJ, Allison TG, Mookadam F, Lopez-Jimenez F. Association of body weight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet 2006;368: 666-78.
25. Oreopoulos A, Padwal R, Norris CM, Mullen JC, Pretorius V, KalantarZadeh K. Effect of obesity on shortand long-term mortality postcoronary revascularization: a meta-analysis. Obesity (Silver Spring) 2008;16: 442-50.
26. Minutello RM, Chou ET, Hong MK, Bergman G, Parikh M, Iacovone F, Wong SC. Impact of body mass index on in-hospital outcomes following percutaneous coronary intervention (report from the New York State Angioplasty Registry). Am J Cardiol 2004;93: 122932.
27. Rea TD, Heckbert SR, Kaplan RC, Psaty BM, Smith NL, Lemaitre RN, Lin D. Body mass index and the risk of recurrent coronary events following acute myocardial infarction. Am J Cardiol 2001;88: 467-72.
28. Zeller M, Steg PG, Ravisy J, Lorgis L, Laurent Y, Sicard P, Janin-Manificat L, Beer J-C, Makki H, Lagrost A-C, Rochette L, Cottin Y; RICO Survey Working Group. Relation between body mass index, waist circumference, and death after acute myocardial infarction. Circulation 2008;118: 482-90.
29. Bucholz EM, Rathore SS, Reid KJ, Jones PG, Chan PS, Rich MW, Spertus JA, Krumholz HM. Body mass index and mortality in acute myocardial infarction patients. Am J Med 2012;125(8): 796-803.
30. Kang WY, Jeong MH, Ahn YK, Kim JH, Chae SC, Kim YJ, Hur SH, Seong IW, Hong TJ, Choi DH, Cho MC, Kim CJ, Seung KB, Chung WS, Jang YS, Rha SW, Bae JH, Cho JG, Park SJ. Obesity paradox in Korean patients undergoing primary percutaneous coronary intervention in ST-segment elevation myocardial infarction. J Cardiol 2010;55: 84-91.
31. Das SR, Alexander KP, Chen AY, Powell-Wiley TM, Diercks DB, Peterson ED, Roe MT, de Lemos JA. Impact of body weight and extreme obesity on the presentation, treatment, and in-hospital outcomes of 50,149 patients with ST-Segment elevation myocardial infarction results from the NCDR (National Cardiovascular Data Registry). J Am Coll Cardiol 2011;58: 2642-50.
32. Madala MC, Franklin BA, Chen AY, Berman AD, Roe MT, Peterson ED, Ohman EM, Smith SC Jr, Gibler WB, McCullough PA. Obesity and age of first non-ST-segment elevation myocardial infarction. J Am Coll Cardiol 2008;52: 979-85.
33. Steinberg BA, Cannon CP, Hernandez AF, Pan W, Peterson ED, Fonarow GC. Medical therapies and invasive treatments for coronary artery disease by body mass: the “obesity paradox” in the Get With the Guidelines Database. Am J Cardiol 2007;100: 1331-5.
34. Fox KA, Poole-Wilson P, Clayton TC, Henderson RA, Shaw TR, Wheatley DJ, Knight R, Pocock SJ. 5-year outcome of an interventional strategy in non-ST-elevation acute coronary syndrome: the British Heart Foundation RITA 3 randomised trial. Lancet 2005;366: 914-20.
35. Lundergan CF, Ross AM, McCarthy WF, Reiner JS, Boyle D, Fink C, Califf RM, Topol EJ, Simoons ML, Van Den Brand M, Van de Werf F, Coyne KS; GUSTO-I Angiographic Investigators. Predictors of left ventricular function after acute myocardial infarction: effects of time to treatment, patency, and body mass index. Am Heart J 2001;142(1): 43-50.
36. Horwich TB, Fonarow GC. Measures of obesity and outcomes after myocardial infarction. Circulation 2008;118: 469-71.
37. Suh JW, Mehran R, Claessen BE, Xu K, Baber U, Dangas G, Parise H, Lansky AJ, Witzenbichler B, Grines CL, Guagliumi G, Kornowski R, Wohrle J, Dudek D, Weisz G, Stone GW. Impact of in-hospital major bleeding on late clinical outcomes after primary percutaneous coronary intervention in acute myocardial infarction the HORIZONSAMI (Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction) trial. J Am Coll Cardiol 2011;58: 1750-6.
38. Lee KL, Woodlief LH, Topol EJ, Weaver WD, Betriu A, Col J, Simoons M, Aylward P, Van de Werf F, Califf RM. Predictors of 30-day mortality in the era of reperfusion for acute myocardial infarction. Results from an international trial of 41,021 patients. GUSTO-I Investigators. Circulation 1995;91: 1659-68.
39. Sonmez K, Akcakoyun M, Akcay A, Demir D, Duran NE, Gençbay M, Degertekin M, Turan F. Which method should be used to determine the obesity, in patients with coronary artery disease? (body mass index, waist circumference or waist-hip ratio). Int J Obes Relat Metab Disord 2003;27: 341-6.
 This work is licensed under a
This work is licensed under a