Smaranda Radu1, Mariana Floria1,2, Ovidiu Mitu1,3, Florin Mitu1,4
1 „Gr. T. Popa” University of Medicine and Pharmacy, Iasi, Romania
2 III Medical Clinic of „Sf. Spiridon” Emergency Hospital, Iasi, Romania
3 Cardiology Clinic of Cardiovascular Diseases Institute
4 Cardiology Clinic of Rehabilitation Hospital, Romania
Abstract: This paper presents the case of an asymptomatic persistent left superior vena cava unmasked by a simple noninvasive cardiac imaging, namely microbubble test by transthoracic echocardiography.
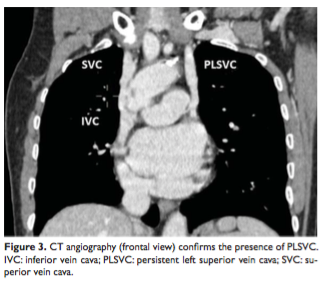
A 25 years old man complaining of atypical chest pain at exertion was examined by the cardiologist. The clinical exam was normal. Twelve leads ECG showed sinus rhythm of 55 beats/min, QRS axis of 70 degree and minor right bundle branch block. Transthoracic echocardiography has shown a large coronary sinus of 32 mm, without right cavities dilatation and without any sign of pulmonary hypertension. Transthoracic echocardiogram was repeated during injection of agitated saline solution into the left basilica vein and micro-bubbles unexpectedly filled firstly coronary sinus and then passed through the right atrium. Contrast enhanced computer tomography angiography confirmed the presence of persistent left superior vein cava and the site of drainage into a large coronary sinus. Right superior vein cava was also identified.
It is mandatory to consider persistent left superior vena cava draining into the coronary sinus in the diagnosis of patients presenting with dilated coronary sinus shown by transthoracic echocardiography. Even if persistent left superior vena cava could be diagnosed by a simple, non-invasive imaging test, an associated heart disease must always be excluded in these patients by another imaging method like computer tomography. This case underlines also the importance of multimodality imaging in the evaluation of these abnormalities.
Keywords: coronary sinus, transthoracic echocardiogram, agitated saline, micro-bubbles.
Rezumat: Lucrarea prezintă cazul unui pacient cu persistenţă de venă cavă superioară stângă asimptomatică demascată printr-o simplă metodă imagistică cardiacă, non-invazivă, şi anume testul cu microbule ecocardiografie transtoracică.
Un bărbat în vârstă de 25 de ani s-a adresat pentru un consult cu acuze de dureri toracice atipice de mai mulţi ani. Examenul clinic a fost normal. Electrocardiograma de suprafaţă a arătat bradicardie sinusală cu 55 bătăi/minut (cu unde P negative în DIII, aVF), axa electrică QRS la 70 de grade şi bloc minor de ramură dreaptă. Ecocardiografia transtoracică a fost în limite normale, cu excepţia unui sinus coronarian dilatat de 32 mm, fără cavităţi drepte mărite şi fără niciun semn de hipertensiune pulmonară. Ecocardiografia transtoracică cu injectare de soluţie salină agitată în vena bazilică stângă a evidenţiat opacifierea atriului drept prin sinusul coronarian şi nu prin vena cava superioară. Examenul computer-tomografic cu substanţă de contrast a confirmat prezenţa unei vene cavă superioară stângă cu drenaj in sinusul coronarian, care era foarte dilatat. Vena cavă superioară dreaptă era prezentă şi nu s-au identificat alte anomalii anomalii anatomice.
În cazul unui sinus coronarian dilatat la ecocardiografia transtoracică este obligatoriu să se ia în considerare persistenţa de vena cavă superioară stângă. Această anomalie poate fi confirmată printr-un test imagistic simplu, non-invaziv, precum testul cu microbule. Întotdeauna trebuie căutată o eventuală anomalie asociată printr-o altă metodă imagistică precum tomografia computerizată cu contrast. Acest caz subliniază importanţa utilizării unui test simplu dar şi a mai multor metode imagistice în evaluarea acestei anomalii.
Cuvinte cheie: sinus coronarian, ecocardiografie transtoracică, soluţie salină agitată, microbule.
BACKGROUND
Persistence of left superior vena cava (PLSVC) is the most common venous anomaly. While affecting 0.5% of the general population, it influences procedures re-quiring vascular intervention or device implantation and may predispose to atrial fibrillation. Despite being mostly asymptomatic, it can be identified through simple cardiac imaging.
CASE REPORT
We present you the case of a 25-year old male referred to the clinic for atypical chest pain at exertion. Taking into account the unremarkable medical history and negative family history, we proceeded into investigating the case.
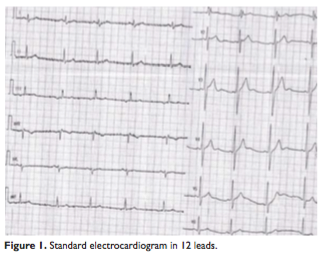
The clinical exam was normal. After performing the ECG, we noted that while being in sinus rhythm with a heart rate of 55 bpm and an AQRS at 60-70 degrees, the patient had a minor right bundle branch block (Figure 1). We also remarked the negative P waves in DIII, aVF.
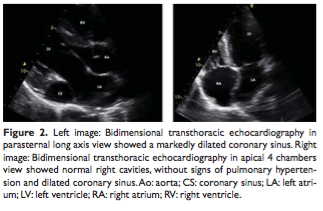
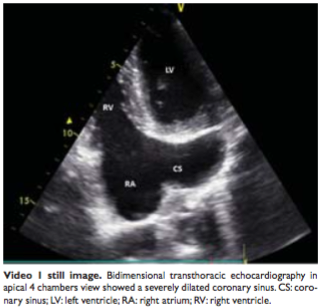
Twenty four hour ECG monitoring was unremarkable. The fact that the patient’s chest pain continued prompted us to perform a transthoracic echocardiography, which showed normal dimensions and functions of the left cavities (Figure 2), and a markedly dilated coronary sinus (CS) of 32 mm in the absence of right cavities dilatation or any signs of pulmonary hypertension (Video 1 still image). The dilated coronary sinus gave rise to the suspicion of a case of PLSVC.The patient refused transoesophageal echocardiography.
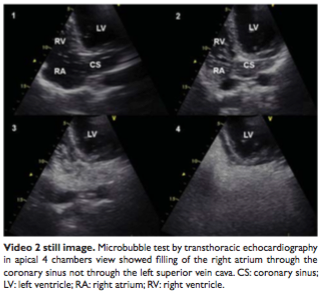
We decided to perform an agitated saline study, injecting the solution in the left arm. Filling of the right atrium with microbubbles not via the superior vein cava, but through the coronary sinus testified for the presence of the aforementioned anomaly (Video 2 still image).
Contrast enhanced computer tomography (CT) angiography confirmed the anomaly, showing the PLSVC draining into the coronary sinus in the presence of normal superior and inferior vein cava (Figure 3).
DISCUSSION
PLSVC is the most common congenital anomaly involving thoracic central venous return1.While ~0.5% of the general population is affected, the percentage rises up
to 10% in those suffering from congenital heart diseases1,2. A PLSVC is an embryological remnant representing persistence of the left anterior cardinal vein that fails to obliterate during embryologic development of right atrium1,3. The right and left anterior cardinal veins drain the cranial regions into the respective ducts of Cuvier, which in turn drain into the sinus venosus. The right cardinal vein and right duct of Cuvier form the superior vein cava. Bridging connection between the anterior cardinal veins forms the left innominate vein. The sinus venosus could be absorbed into the structure of the right atrium.
It has multiple possible draining sites including inferior vein cava, hepatic vein or left atrium, the most common being right atrium via the CS (about 90% of cases)1. Another possibility is drainage into the left atrium through an unroofed CS, thus giving rise to a right-to-left shunt. Most of the times it remains an incidental finding, as this anomaly is clinically silent in its most common form. In rare cases, PLSVC can determine severe right heart dilatation by draining into left atrium in association with an unroofed CS and CS atrial septal defect4. However PLSVC typically drains into the coronary sinus via the vein of Marshall.
Usually the LSVC descends vertically, anterior, and to the left of the aortic arch and main pulmonary artery and enters the left atrium between the pulmonary veins and the atrial appendage, draining, most frequently into the CS. In patients with suspected PLSVC while left arm injection during microbubble test determines fills CS first, followed by right atrium, right arm injection will determines fills right atrium first. Bilateral arm contrast injections should be performed if suspecting a PLSVC, such as an enlarged CS, but do not expand on the reasoning. Bilateral injections can determine rightand left-sided anomalous drainage.
Though drainage into the right atrium via the CS holds no hemodynamic consequences, it could translate into a difficulty when undergoing device implantation or other procedures requiring vascular access. Another risk cited in literature is developing cardiac arrhythmias, particularly atrial fibrillation due to the ligament of Marshall. Given the right-to-left shunt that drainage into the left atrium creates, patients most typically present with cyanosis at this point. Other cardiovascular anomalies have been associated with PLSVC, such as atrial or ventricular septum defects, tetralogy of Fallot, and CS ostium atresia1.
The differential diagnosis of a dilated CS includes partial anomalous hepatic venous drainage and continuity of the inferior vein cava with an LSVC via the hemiazygos vein. Various shunts may result in CS dilatation, either low pressure in the case of unroofed CS and anomalous pulmonary venous drainage, or high pressure in the form of a coronary artery to CS fistula5. Finally, any cause of raised right atrial pressure may cause dilatation.
Despite being mostly asymptomatic, the fact that this anomaly is easily detected through cardiac imaging such CT, magnetic resonance imaging and transthoracic echocardiography should prompt clinicians for a throughout set of investigations when suspecting such an anomaly. We also emphasize the importance of the microbubble test that, while being easily reproduced with a minimum set of risks for the patient, it enables early detection of abnormal intracardiac blood flow. Even if PLSVC could be diagnosed by a simple, non-invasive imaging test, an associated heart disease must always be excluded in these patients by another imaging method like CT. However multimodality imaging in the evaluation of these abnormalities is very important.
The authors presented the case of a young asymptomatic patient with a benign congenital anomaly unmasked by a simple non-invasive cardiac imaging, namely microbubble test (verz useful but perhaps underused in clinical practice) and confirmed by another cardiac imaging technique like CT angiography.
Conflict of interest: none declared.
Funding: none.
References
1. Irwin RB, Greaves M, Schmitt M. Left superior vena cava: revisited. Eur Heart J – Cardiovascular Imaging 2012; 13: 284–291.
2. Altschul E, Shah AB, Skipitaris N, Bhasin K, Kronzon I. Persistent anomaly complicating pacemaker placement. Eur Heart J Cardiovasc Imaging 2016 Apr 29. pii: jew059. [Epub ahead of print]
3. Campbell M, Deuchar DC. The left-sided superior vena cava. Br Heart J 1954;16: 423–39.
4. Speiser U, Quick S, Sandfort V, Strasser RH, Kolschmann S. Persistent left superior vena cava draining into left atrium, unroofed coronary sinus, and coronary sinus atrial septal defect as rare cause for severe right heart dilatation: diagnostic steps and therapy. Eur Heart J Cardiovasc Imaging 2014;15(6):711.
5. Mantini E, Grondin CM, Lillehei W, Edwards JE. Congenital anomalies involving the coronary sinus. Circulation 1966;33:317–27.
Video legends
Video 1: Bidimensional transthoracic echocardiography in apical 4 chambers view show markedly dilated coronary sinus in the absence of right cavities dilatation or any signs of pulmonary hypertension.
Video 2: Bidimensional transthoracic echocardiography in apical 4 chambers and agitated saline study: filling of the right atrium with microbubbles not via the superior vein cava, but through the coronary sinus.
 This work is licensed under a
This work is licensed under a