Dan Mihai Alexandrescu1, Liviu Macovei2, Cristina Ciobanu1, Larisa Anghel1, Amin Bazyani1, Ana Tanasa, Catalina Arsenescu Georgescu2
1 „Prof. Dr. George I.M.Georgescu” Institute of Cardiovascular Diseases, Iasi, Romania
2 „Grigore T. Popa” University of Medicine and Pharmacy, „Prof. Dr. George I.M.Georgescu” Institute of Cardiovascular Diseases, Iasi, Romania
3 „Grigore T. Popa” University of Medicine and Pharmacy, „Prof. Dr. George I.M.Georgescu” Institute of Cardiovascular Diseases, Iasi, Romania
Abstract: Introduction – Despite proper antiplatelet treatment, some patients show resistance to aspirin or clopidogrel, with important consequences in terms of morbidity or mortality. The factors which induce a high risk of in-stent thrombosis are: diabetes, obesity, dyslipidemia, severe left ventricular dysfunction or complex coronary lesions. Material and Method – We present a 65 years patient with high blood pressure and metabolic syndrome, with important vascular impairment, who had initially underwent angioplasty with pharmacologically active stent on the left anterior descending coronary artery for unstable angina pectoris, but later, under a proper dual antiplatelet therapy, developed subacute in-stent thrombosis with important implications on the clinical course (extensive anterior acute myocardial infarction). Results – Following the coronarographic confirmation of the instent thrombosis, thromboaspiration was performed obtaining a TIMI III flow. The clopidrogel sensitivity testing confirmed the resistance to this drug that required its replacement with ticagrelor. The subsequent evolution was favourable, but a significant myocardial contractile reserve was lost. Conclusions – In stent thrombosis represents a current problem in the interventional treatment of the coronary lesions with severe clinical and prognostic implications. A closer analysis of the associated prothrombotic conditions, as well as the preliminary testing of the clopidogrel resistance, could significantly decrease the risk of in-stent thrombosis.
Keywords: in stent thrombosis, antiplatelet therapy resistance, acute myocardial infarction.
Abstract: Introducere – În ciuda tratamentului antiagregant corect administrat, unii bolnavi prezintă rezistenţă la aspirină sau clopidogrel, cu importante consecinţe în termeni de morbiditate sau mortalitate. Factorii care induc un risc crescut de tromboză intrastent sunt reprezentaţi de: diabetul zaharat, obezitatea, dislipidemia, disfuncţia severă a ventriculului stâng precum şi leziunile coronariene complexe. Material şi metodă – Prezentăm cazul unui pacient de 65 ani, hipertensiv, cu sindrom metabolic şi afectare vasculară importantă, care iniţial a beneficiat de angioplastie cu stent activ farmacologic pe artera coronară descendentă anterioară pentru angină pectorală instabilă. Ulterior, în condiţiile unei terapii duble antiagregante corecte pacientul prezintă tromboză subacută intrastent cu importante implicaţii clinico-evolutive (infarct miocardic acut anteroextensiv). Rezultate – După confirmarea coronarografică a trombozei intrastent s-a reintervenit şi s-a practicat tromboaspiraţie cu obţinerea unui flux TIMI III. Testarea sensibilităţii la clopidogrel a confirmat existenţa rezistenţei la acest drog, ceea ce a impus înlocuirea cu ticagrelor. Ulterior, evoluţia a fost favorabilă, dar cu pierderea unei importante rezerve miocardice contractile. Concluzii – Tromboza intrastent reprezintă o problemă de actualitate în tratamentul intervenţional al leziunilor coronariene, cu implicaţii clinico-prognostice severe. O analiză atentă, a condiţiilor asociate protrombotice, precum şi testarea prealabilă a rezistenţei la clopidogrel, ar putea scădea semnificativ riscul de tromboză intrastent.
Cuvinte cheie: tromboza intrastent, rezistenţă la terapia antiplachetară, infarct miocardic acut.
INTRODUCTION
In stent thrombosis is one of the major complications of the coronary angioplasty that requires emergency treatment. Depending on the elapsed time since stent implantation, thrombosis can be acute (in the first 24 hours), subacute (in the first 30 days), late (in the first year) or very late (after one year). The risk of developing in stent thrombosis is 1,5%, simple stents are commonly involved especially in the moment when the dual antiplatelet theraphy is stopped1,2.
MATERIAL AND METHOD
We present the case of a 65 years old patient, with high blood pressure, diabetes, obesity, dyslipidemia with important vascular impairment (obstructive artheriopathy of the lower limbs stage II A Leriche Fontaine and inferior myocardial infarction at 50 years old) who is admitted to hospital for angina pains on exertion.
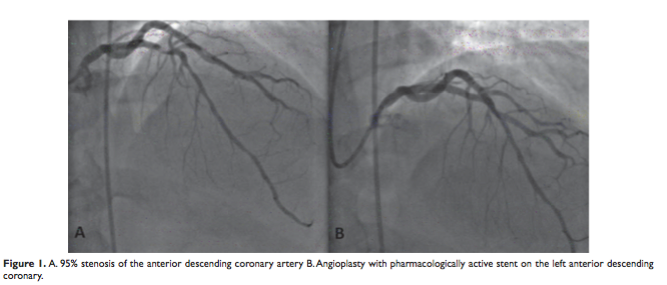
The coronarography revealed bicoronary lesions: old occlusion of the right coronary artery and 95% lesion of the anterior descending coronary artery on which there was performed a transluminal angioplasty with the insertion of the pharmacologically active stent. After selective intubation of the left anterior descending coronary artery with a VODA 3.5 guide catheter, we cross the stenosis area with 0.014 guide wire. We directly implant a drug eluting 3.0/19 mm stent at 20 atm, yielding the regression of the lesion from 95% to 0%. (Figure 1) The patient received 300 mg loading dose of clopidogrel, followed by 75 mg/day.
Three days after the angioplasty, the patient is again admitted to the hospital for a big crisis of angina of 7 hours. The electrocardiogram reveals the presence of the sinus rythm with 80/min frequency with newly appeared changes suggestive for acute anterior myocardial infarction with ST elevation segment. The biochemical tests confirm the infarction hypothesis (CKMB 256 UI, AST 94 UI, LDH 500 UI). A nonspecific inflammatory syndrome is also confirmed (fibrinogen 718 mg/dl, CRP 20 mg /dl, WBC 15000/mm with neutrophilia (69%)).
The transthoracic echocardiogram shows a non-dilated left ventricle with moderate systolic dysfunction (35% ejection fraction), with significant kinetic disorders in the anterior region (apex, medioapical septum and anterior wall dyskinesia).
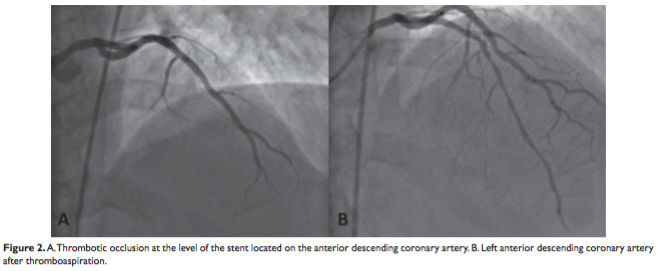
A new coronography was carried out and it confirmed the acute thrombotic occlusion at the level of the stent located on the anterior descending coronary artery. Thromboaspiration was carried out, leading to the repermeabilisation of the vessel (TIMI III flow) (Figure 2).
Treatment with the glycoprotein IIb/IIIa inhibitor (Eptifibatide) and unfractionated heparin was initiated. The clopidogrel sensitivity testing confirmed the resistance to this drug, which required its replacement with ticagrelor 180 mg/day.
DISCUSSIONS
In stent thrombosis is a major problem with current prognostic implications. The main causes of stent thrombosis, whether we are talking about bare metal stents (BMS) or drug-eluting stents (DES), are: stent under expansion; strut fracture, stent deformation or other mechanical complications and drug resistance3.
Uren NG et al in a study in 2002 have reported that stent malapposition is a predictor of early or very late stent thrombosis4.
Another important mechanism is the resistance to antiplatelet therapy. Despite proper antiplatelet treatment, some patients show resistance to aspirin or clopidogrel. The resistance to the antiplatelet agent could be defined as an inhibiting deficiency of the platelets function, followed by the inefficiency of the prevention of the atherothrombotic ischemic events5.
Clopidogrel inhibits the ADP mediated platelet aggregation in a percentage of 30-50% by blocking the ADP-P2Y12 receptor in the platelet membrane. If there is an increased release of ADP or an alternative way of platelet activation is stimulated, then its antipletelet action is insufficient, increasing the risk of coronary events. CREST study mentions that an incomplete inhibition of the P2Y12 receptors represents a risk factor for the subacute stent thrombosis6,7.
RECLOSE 1 study carried out by Buonamici et al. in 2007 mentions a number of comorbidities associated with a weak response to clopidogrel, such as diabetes, insulin resistance, obesity, hypercholesterolemia, left ventricular systolic dysfunction and congestive heart failure8-10. Of all these, the high body mass index has been identified as an important predictor of body resistance to clopidogrel11. Another study carried out on patients with coronary angioplasty who initially underwent intravascular ultrasound and later received dual antiplatelet treatment associates the weak response to clopidogrel with long coronary stenosis, highly calcified, bifurcation stenosis or stenosis on small caliber vessels, with slow flow or accompanied by coronary dissection12.
Under these circumstances, the new antiplatelet agents offer a good alternative, decreasing significantly the risk of stent thrombosis. Prasugrel or ticagrelor are new treatment options, clinical studies showing their superiority compared to clopidogrel in inhibiting the platelet aggregation13,14.
The presented case of subacute thrombosis in pharmacologically active stent meets many conditions that can cause the resistance to clopidogrel. The patient has diabetes, is overweight and dyslipidemic. At the same time, the performed treatment with atorvastatine and omeprazol could have interfered with the clopidogrel metabolization process, limiting the prodrug turning into its active component. After the acute coronary event, clopidogrel was replaced with ticagrelor. The subsequent evolution of the patient was good, without other ischemic events, but with the loss of a significant myocardial contractile reserve.
CONCLUSIONS
In the patient with coronary angioplasty with stent, the antiplatelet dual therapy should be chosen depending on the individual risk of in-stent thrombosis that can be assessed based on the clopidogrel sensitivity testing and on the presence or absence of certain associated prothrombotic conditions (comorbidities such as diabetes, obesity, insulin resistance, dyslipidemia, as well as the presence of severe ventricular dysfunction or complex coronary lesions). It seems that the use of the new platelet antiagregants (ticagrelor, prasugrel) could significantly reduce the risk of in-stent thrombosis.
Conflict de interest: none declared.
References
1. Stoicescu C, Vintila V, Udroiu C, et al. Outcome and Predictors of Stent Thrombosis in the First Romanian Registry of Drug Eluting Stent (RODESINO EXTENSION). Maedica (Buchar) 2013;8(2):15363.
2. L. Vasiluta, T. Ciocarlie, L. Petrescu, et al. Prognostic factors in patients with myocardial infarction with ST elevation at 12 hours after the acute event. Journal of Experimental Medical & Surgical Research Cercetãri Experimentale & Medico-Chirurgicale 2013;4:131–135.
3. Alfonso F, Byrne RA, Rivero F, et al. Current treatment of in-stent restenosis. J Am Coll Cardiol. 2014;63:2659–73.
4. Uren NG, Schwarzacher SP, Metz JA, et al. Predictors and outcomes of stent thrombosis: an intravascular ultrasound registry. EurHeart J 2002; 23: 124-132.
5. Bonello L, Tantry US, Marcucci R, et al. Consensus and future directions on the definition of high on-treatment platelet reactivity to adenosine diphosphate. J Am Coll Cardiol 2010;56:919-33.
6. Gurbel PA, Bliden KP, Samara W, et al. Clopidogrel effect on platelet reactivity in patients with stent thrombosis: results of the CREST Study. J Am Coll Cardiol 2005;46:1827-32.
7. Nicoleta Alexandru, Doina Popov, Adriana Georgescu. Platelet dysfunction in vascular pathologies and how can it be treated Thrombosis Research 2012 Feb;129(2):116-26.
8. Angiolillo DJ, Fernández-Ortiz A, Bernardo E, et al. Platelet aggregation according to body mass index in patients undergoing coronary stenting: should clopidogrel loading-dose be weight adjusted? J Invasive Cardiol 2004;16:169-74
9. Bernlochner I, Byrne RA, Kastrati A, et al. The future of platelet function testing to guide therapy in clopidogrel low and enhanced responders. Expert Rev Cardiovasc Ther 2011;9:999-1014.
10. Buonamici P, Marcucci R, Migliorini A, et al. Impact of platelet reactivity after clopidogrel administration on drug-eluting stent thrombosis. J Am Coll Cardiol 2007;49:2312-7.
11. Bonello-Palot N, Armero S, Paganelli F, et al. Relation of body mass index to high on-treatment platelet reactivity and of failed clopidogrel dose adjustment according to platelet reactivity monitoring in pati-ents undergoing percutaneous coronary intervention. Am J Cardiol
2009;104:1511-5.
12. Chirumamilla AP, Maehara A, Mintz GS, et al. High platelet reactivity on clopidogrel therapy correlates with increased coronary atherosclerosis and calcification: a volumetric intravascular ultrasound study. JACC Cardiovasc Imaging 2012;5:540-9.
13. Wiviott SD, Trenk D, Frelinger AL, et al. Prasugrel compared with high loadingand maintenance-dose clopidogrel in patients with planned percutaneous coronary intervention: the Prasugrel in Comparison to Clopidogrel for Inhibition of Platelet Activation and Aggregation-Thrombolysis in Myocardial Infarction 44 trial. Circulation 2007;116:2923-32.
14. Cannon CP, Husted S, Harrington RA, et al. Safety, tolerability, and initial efficacy of AZD6140, the first reversible oral adenosine diphosphate receptor antagonist, compared with clopidogrel, in patients with non-ST-segment elevation acute coronary syndrome: primary results of the DISPERSE-2 trial. J Am Coll Cardiol 2007;50:1844-51.
 This work is licensed under a
This work is licensed under a