Daniel Gherasim1, Mircea Iurciuc2, Cristina Voiculet3, Alina Giuca4, Virgil Petrescu5, Florin Maghiar6, Alexandra Gherghina7, Adrian Tase8, Carmen Ginghina1,9
1 “Prof.Dr.C.C.Iliescu” Emergency Institute for Cardiovascular Diseases, Bucharest
2 “Victor Babes” University of Medicine Timisoara
3 Clinical Emergency Hospital Constanta
4 Emergency County Clinical Hospital, Cardiology Center, Craiova
5 Colentina Universitary Hospital, Bucharest
6 University of Medicine Oradea
7 Clinical Emergency Hospital Brasov
8 University of Pitesti, Faculty of Nursing, Emergency County Hospital Pitesti
9 “Carol Davila” University of Medicine and Pharmacy, Cardiology Department, Bucharest
Contact address:
Daniel Gherasim, Clinic of Cardiology, Emergency Institute for Cardiovascular Diseases, 258 Fundeni Avenue, 2nd District, Bucharest, Zip code 022328. E-mail: gherasimdanro@yahoo.com
Abstract: The aim of the study was to evaluate the compliance with angiotensin II receptor blockers (ARBs) treatment in hypertensive patients persistent on this medication for at least 6 month and to identify the factors asociated with it. Material and method – Open-label, non-randomized, national, retrospective disease registry, that collected data from 12,538 hypertensive patients in treatment with an ARB for the last 6 months, from 621 study centers of ambulatory clinical practice, mainly cardiological or primary medical care all over the country. The study evaluated the level of ARBs treatment compliance, assessed by applying the adapted Medication Adherence Self-Report Inventory questionnaire (MASRI) part I and estimated the medication possesion rate (MPR). The MASRI is a questionnaire filled in by patients addresseing the frequency and correct timing of medication intake. Results – The patients, 45.4% male and 54.3% female, with a mean age of 60.9 years old, were treated with combination therapy in >80% of cases and the drugs most frequently associated to sartans were diuretics (~57%).The mainly associated risk factors were hypercholesterolemia (73,7%) and obesity (59,6%) and the most part of the patients are coming from urban environment (73,7%). MPR was above 80% value, considered to be the inferior level of adherence to antihypertensive therapy, in 96.6% of the patients on ARB monotherapy and in 96.5% of those with ARB in combinations. None of the evaluated demographic or medical factors influenced significantly the compliance with ARB treatment. In the subgroup of patients with ARBs in combinations, urban environment determined significantly higher compliance than rural environment [relative risk (RR) = 1.093, confidence interval (CI) = 1.018 – 1.173]. Conclusion – Our study showed a very good compliance with ARB treatment in hypertensive patients persistent on ARB treatment for 6 month, in ambulatory practice; MPR> 80% has been registered in 96.5% of the patients with ARBs treatment, in monotherapy or in combinations.
Keywords: Hypertension, compliance, angiotensin II receptor blockers
Abstract: Obiectivele studiului – Evaluarea complianţei la tratamentul cu blocanţi ai receptorilor de angiotensină II (BRA) la pacienţii hipertensivi cu o persistenţă de cel puţin 6 luni pe această terapie şi, de asemenea, identificarea factorilor asociaţi. Material și metodă – Registru de boală naţional, retrospectiv, nerandomizat în care au fost colectate date de la 12,538 de pacienţi hipertensivi care urmau tratament cu un BRA de 6 luni, din 621 de centre de consultaţie de specialitate în ambulatoriu, în principal de cardiologie sau de medicină primară, din toată ţara. Studiul a evaluat complianţa la tratamentul cu BRA, determinată prin aplicarea unui chestionar adaptat de auto-raportare a aderenţei la medicație (MASRI partea I) şi estimarea ratei de posesie a medicaţiei (medication possesion rate, MPR). MASRI este un chestionar completat de către pacienţi care se referă la frecvenţa şi la corectitudinea administrării medicaţiei. Rezultate – Pacienţii, 45,4% bărbaţi şi 54,3% femei, cu o vârstă medie de 60,9 ani, primeau terapie combinată în mai mult de 80% din cazuri, iar medicamentele cel mai frecvent asociate sartanilor au fost diureticele (~57%). Principalii factori de risc asociaţi au fost hipercolesterolemia (73,7%) şi obezitatea (59,6%) iar majoritatea pacienţilor provenea din mediul urban (73,7%). MPR a fost peste valoarea de 80%, considerată a fi limita inferioară pentru aderenţa la terapia antihipertensivă, pentru 96,6% dintre pacienţii cu BRA în monoterapie şi pentru 96,5% pentru cei cu BRA în terapie combinată. Niciunul dintre factorii demografici sau medicali evaluaţi nu a influenţat semnificativ complianţa la tratamentul cu BRA. În subgrupul de pacienţi cu BRA în cadrul unei terapii combinate, provenienţa din mediul urban a determinat o complianţă semnificativ mai mare comparativ cu cel rural [risc relativ (RR) = 1.093, interval de încredere (II) = 1.018 – 1.173]. Concluzie – Studiul nostru a arătat o complianţă foarte bună la tratamentul cu BRA la pacienţii hipertensivi persistenţi pe această terapie timp de 6 luni, trataţi in ambulator; indicele de posesie a medicaţiei MPR> 80% a fost înregistrat la 96,5% dintre pacienţii în tratament cu BRA, în monoterapie sau în terapie combinată.
Cuvinte cheie: hipertensiune arterială, complianţă, blocanţi de receptor de angiotensină II
INTRODUCTION
The World health statistics – Geneva 2012 report, released on 16 May 2012, puts the spotlight on the growing problem of the noncommunicable diseases burden. One in three adults worldwide, according to the report, has raised blood pressure – a condition that causes around half of all deaths from stroke and heart disease1. Epidemiological data for Romania are coming from SEPHAR studies which took place in 2005 and 2011, being initiated with the purpose of estimating the hypertension’s prevalence, treatment and control in adult population for developing prevention strategies in hypertension management. In SEPHAR II study hypertension was recorded in 40.4% of cases (798 subjects from 1975 responders)2. Other studies conducted on selected populations showed a variable HT prevalence3,4.
The raised levels of blood pressure represent the consequence of a complex interplay of environmental and genetic factors. The primary goal of treatment of the patient with high blood pressure is to achieve the maximum reduction in the long-term total risk of cardiovascular morbidity and mortality. This requires treatment of all identified risk factors and the appropriate management of associated clinical conditions, as well as treatment of the raised blood pressure per se5. The use of antihypertensive drug therapy has been shown to reduce the risk of stroke and coronary heart disease by an estimated 30-40% and 20%, respectively, in long-term randomized controlled trials (RCTs)6.
The underlying haemodynamic disorder in the majority of cases is a rise in peripheral vascular resistance, so the vasodilatator effect was an important feature for the strategies developed over time for the treatment of hypertension7. Among the antihypertensive clases, a special interest is given to the renin-angiotensin system (RAS) blockers, related to the role of this sistem in the pathophysiology of hypertension and organ injury8.
Angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin II receptor blockers (ARBs) are widely used in patients with hypertension, heart failure and diabetes as well as in other clinical conditions sharing an increased cardiovascular risk9. Individual trials and meta-analyses showed that both ACEIs and ARBs are effective in reducing the risk of total cardiovascular events and specific events such as stroke, myocardial infarction and heart failure10,11. Despite the availability of safe and effective antihypertensive agents, hypertension and its concomitant risk factors remain uncontrolled in most patients12.
One of the major factor of poor control of hypertension is nonadherence of the patients to medical treatment. Studies have shown that around 50% of individuals discontinue antihypertensive medications within 6 to 12 months of their initiation13.
Overall, one third of patients used antihypertensive therapy continuously during the 10 years of follow-up and one third permanently discontinued therapy14.
Nonadherence to medical treatments is an increasingly recognized cause of adverse outcomes and increased health care costs. Drug compliance is defined as the extent to which patients follow medical instructions. This term was replaced by ‘adherence’ which includes also the responsibility of the caregivers. Adherence has been defined as ‘the active, voluntary, and collaborative involvement of the patient in a mutually acceptable course of behaviour to produce a therapeutic result’15. Medication persistence refers to the act of continuing the treatment for the prescribed duration. It may be defined as “the duration of time from initiation to discontinuation of therapy”16.
There are many different methods of assessing adherence to medications. Osterberg et al17 categorized these methods as either direct or indirect. Direct methods include directly observed therapy, measurement of the level of medicine or metabolite or the biological marker in blood sample. Despite the fact that these direct methods are considered to be more robust than indirect methods, they are not practical for routine clinical use. Indirect methods of adherence assessment include patient questionnaires, self-reports, pill counts, rate of prescription refills, assessment of the patient’s clinical response, electronic medication monitors, measurement of physiological markers and patient diaries. The most commonly used indirect methods include patient self-report, pill counts and pharmacy refills18.
The objective of our study is to evaluate the compliance with ARBs medication of hypertensive patients already treated for at least 6 month with these drugs. Another goal is to raise the awereness on the importance of treatment adherence in chronic patients and to identify the factors asociated with it.
MATERIALS AND METHODS
I ADHERE is an open-label, non-randomized, national (Romania), multicentric, retrospective disease registry, sponsored by Sanofi, that collected data from 12,538 patients, in 621 study centers of ambulatory clinical practice, cardiological or primary medical care all over the country. All patients signed an informed consent for participation and were informed on the study objectives.
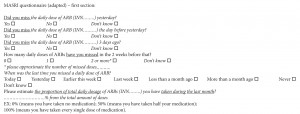
The purpose of I ADHERE was to establish the achievement of the prescribed regimen of ARBs (amount of medication actually taken), based on a questionnaire filled by patients, in a population persistent on ARBs treatment for at least 6 months. The study evaluated the level of ARBs treatment compliance, assessed by applying the adapted Medication Adherence Self-Report Inventory questionnaire (MASRI) part I and estimated the medication possesion rate (MPR). The MASRI is a 12-item questionnaire originally developed for use in Human Immunodeficiency Virus (HIV) populations. The MASRI addresses the frequency and correct timing of medication intake. Its reliability and specificity were high using a set of measures such as test-retest consistency and internal consistency19. In our study we used only the first adapted section of the questionnaire related to the amount of medication actually taken (Figure 1).
Patients included in this study were adults hypertensive patients (according to ESC/ESH guidelines, 2007), age >18 years, men and women, in treatment with an ARBs (in either monotherapy or in combination) for the last 6 months, who accepted to sign the informed consent. Exclusion criteria were: patient’s refusal to sign the informed consent; patient’s refusal or incapacity to complete the MASRI questionnaire; ARB treatment for other indication than hypertension.
Primary objectives were the assessment of adherence on ARB treatment in hypertensive patients who are persistent on ARBs treatment for at least 6 months, evaluating the level of compliance, in ambulatory practice, by the use of a MASRI (Medication Adherence Self-Report Inventory) type auto-evaluation questionnaire and the estimation of MPR (medication possession rate) considering that MPR 0.80 is the inferior margin of adherence to antihypertensive therapy (according with Siegel D et al.).
We looked also (as secondary objectives) for: finding factors associated with adherence (MPR >0.80) to ARBs given in monotherapy or given in combinations in a population persistent on this medication for 6 months; assessment of standard diagnostic procedures for hypertension in the ambulatory clinical practice and for assessment of standard therapy for hypertension in the ambulatory clinical practice. We collected demographic data of the patients, and also we noted personal history of cardiovascular disease and organ damages, risk factors / comorbidities, standard of diagnostic procedures for hypertension (type of laboratory exams / other exploratory investigations recommended) and previously antihypertensive treatment prescribed.
Statistical methods
The main statistical analysis was descriptive: for the continuous data the mean, median and mode values, standard deviations and 95% two-tailed confidence interval (CI) have been calculated and for categorical data the proportions and 95% CI (two-sample Z-test). Presuming that 50% of patients have a good treatment adherence, for estimating the adherence rate with a precision of 1.5% and assuming a level of alpha error of 0.05 and a power of 90%, we needed to include at least 4538 patients. If we also assume an attrition rate of 25%, then 5672 patients should have been included. This sample size has been amended one month after the first patient was enrolled. For establishing positive correlation between some factors and drug therapy adherence, the Odds Ratio (OR) had to be calculated, the cut-off value for positive correlation being fixed at 1.5. For the secondary exploratory end-points, the sample-size estimation had to take into consideration the frequency of the factors involved as independent variables in the regression model. For some certain valuable factors, these frequencies estimated are low (no more than 2%). Assuming a cut-off value for OR of 1.5 and also a p-value of 0.05 and a power of 90%, the sample-size had to be at least of 10,555 patients.
RESULTS
Characteristics of the patients
Data were collected for 12,538 patients out of whom only 12,483 were eligible according to the inclusion criteria and were included in the study analysis. 55 patients have been excluded from the analysis because they didn’t meet the inclusion criteria – 13 were not hypertensive patients (according to ESC/ESH guidelines, 2007), and 42 were not treated with ARBs during the 6 months preceding the study visit. The 12,483 eligible patients were diagnosed with arterial hypertension (according to ESC/ESH guidelines, 2007) and were treated with sartans 6 months before the enrollment. 45.4% were male and 54.3% were female (for 0.4% data were missing) and the mean age was 60.9 years. 24.8% of them were living in rural areas, while 73.7% were coming from urban environment, for 1.5% this data were missing.
The mean duration of the arterial hypertension was 6.3 years. The mean values of blood pressure (BP) registered at the study visit were: 153.6 mmHg (sistolic BP), 89.3 mmHg (diastolic BP), (with a maximul value of 280 mmHg for sistolic BP and 160 mmHg for diastolic BP).
Associated risk factors: 34.4% of the patients were smokers (for 0.8% data were missing); 73.7% had hypercholesterolemia (HC) (for 2.9% cholesterol was not determined and for 0.6% data were missing), and 52.8% hypertriglyceridemia (HT) (for 3.7% triglycerides were not determined and for 0.9% data were missing). 59.6% of the patients had abdominal obesity, defined as: > 102 cm for male and > 88 cm for female patients (for 1.6% was not determined, for 1% data were missing); 32.6% had diabetes mellitus (DM) type 1 or type 2 (for 2.7% unknown, for 0.9% data were missing) (Figure 2).
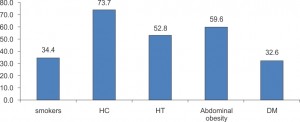
Figure 2. Percentages (%) of patients with associated risk factors: HC – hypercholesterolemia; HT – hypertriglyceridemia; DM – diabetes mellitus.
Many of the patients had target organ damage: 49.8% had left ventricular hypertrophy (ECG diagnosed) with 4.1% not determined (for 1.1% data were missing); 38% had retinopathy (for 1.7% data were missing). Proteinuria (>300 mg/24 hours) was determined for 15.4% of the patients and it was present in 8.9% of the cases. Mean value of serum creatinine was 1.07 mg/dl; 8.8% of patients had chronic renal failure (for 2.4% data were missing).
Another important aspect was the high frequence of cardiovascular diseases in hypertensive patients included in this study. 40.3% of the patients had history of coronary disease (angina pectoris and/or myocardial infarction), for 0.8% data were missing; 16.8% had history of cerebrovascular disease (stroke/transient ischemic attack), for 1.7 data were missing; 13.9% had peripheral artery disease (for 9.3% was undetermined and for 0.9% data were missing), 11% of the patients had atrial fibrillation with 1.9% not determined and 25% had heart failure (10.3% with reduced ejection fraction and 14.7% with preserved ejection fraction), for 1.5% data were missing (Figure 3). The data regarding previous history of cardiovascular diseases were based upon the patients’ medical documents.
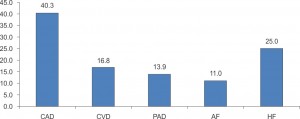
Figure 3. Percentages (%) of patients with associated cardiovascular diseases: CAD – coronary diseases;CVD – cerebrovascular diseases; PAD – peripheral artery diseases; AF – atrial fibrillation; HF – heart failure.
Blood pressure measurement was based on specific recommendations of the European Society of Hypertension 6; the methods used for BP monitoring in patients with hypertension are represented in Figure 4, with the measure of blood presure in the clinic office beeing performed at almost half of the patients.
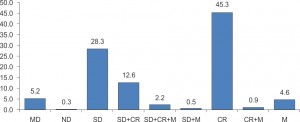
Figure 4. Percentages (%) of patients with BP determined by the following methods: missing data-MD; not determined-ND; self-determination-SD; self-determination +consulting room–SD+CR; self-determination +consulting room+24h monitoring-SD+CR+M; self-determination+24h monitoring- SD+M; consulting room- CR; consulting room+24h monitoring- CR+M; 24h monitoring- M.
The laboratory investigations and the search for subclinical organ damage are presented in Table 1.
Table 1. ABI – Ankle Brachial Index, FBG – Fasting Blood Glucose, TC – Total Cholesterol, HDL-C – HDL Cholesterol, LDL-C – LDL Cholesterol, TG – Triglyceridemia.
| EKG | Echo cardiography |
Optic fundus exam | Chest radiography | ABI | FBG | TC | HDL C | LDL C | TG | Albuminuria | Serum creatinine | Natremia | Kalemia | |
| Yes n (%) | 12186 (97.6%) |
9822 (78.7%) | 9681 (77.6%) |
7895 (63.2%) |
5538 (44.4%) | 12181 (97.6%) | 12097 (96.9%) | 10894 (87.3%) | 10676 (85.5%) | 11894 (95.3%) | 6411 (51.4%) | 11708 (93.8%) | 7452 (59.7%) | 7757 (62.1%) |
| No n (%) |
238 (1.9%) |
2406 (19.3%) | 2577 (20.6%) |
4128 (33.1%) | 6158 (49.3%) | 222 (1.8%) | 305 (2.4%) | 1389 (11.1%) | 1575 (12.6%) | 589 (4.7%) | 5383 (43.1%) | 609 (4.9%) | 4404 (35.3%) | 4111 (32.9%) |
| Missing data n (%) |
59 (0.5%) | 255 (2%) | 225 (1.8%) | 460 (3.7%) | 787 (6.3%) | 80 (0.6%) | 81 (0.6%) | 200 (1.6%) | 232 (1.9%) | 0 | 689 (5.5%) | 166 (1.3%) | 627 (5%) | 615 (4.9%) |
The antihypertensive treatment
In the 6 months before the enrollment in the study the recommended antihypertensive treatment was ARBs in 12,483 patients (100% as per inclusion criteria), ACEIs in 1271 patients (10.2%), calcium channel blockers (CCB) in 3484 patients (27.9%), beta-blockers in 7063 patients (56.6%) and diuretics in 7178 patients (57.5%). ARBs were recommended as monotherapy in 15.9% and in combinations in 84.1% of the patients. At the study visit the treatment recommended was represented by the following: ARBs in 12,467 patients (99.9%), ACEIs in 1201 patients (9.6%), CCB in 3537 patients (28.3%), beta-blockers in 4690 patients (37.6%) and diuretics in 7164 patients (57.4%) of the patients.
As a profile, the enrolled patients were hypertensives mainly comming from urban environment, had abdominal obesity and dyslipidemia, many of them were on combination therapy and the drugs most frequently associated to sartans were diuretics.
The compliance on ARBs treatment was evaluated in patients treated with ARBs at least 6 months before the enrollment by using an adapted MASRI (Medication Adherence Self-Report Inventory) questionnaire section I (Table 2).
Table 2. Adapted MASRI type auto-evaluation questionnaire section I; (a) and (b) denotes a subset of categories which column proportions differ (a/b) or do not differ (a/a) significantly from each other at the 0.05 le
| Did you miss your daily dose of ARB yesterday? | ARB in combination (n=10504) | ARB monotherapy (n=1979) | Total | ||
| No | 10,234 | 97.4% (a) | 1930 | 97.5% (a) | 97.4% |
| Yes | 188 | 1.8% (a) | 40 | 2.0% (a) | 1.8% |
| I don’t know | 44 | 0.4% (a) | 6 | 0.3% (a) | 0.4% |
| No answer | 38 | 0.4% | 3 | 0.2% | 0.3% |
| Did you miss to your daily dose of ARB the day before yesterday? | ARB in combination | ARB monotherapy | Total | ||
| No | 10,261 | 97.7% (a) | 1939 | 98% (a) | 97.7% |
| Yes | 102 | 1.0% (a) | 21 | 1.1% (a) | 1.0% |
| I don’t know | 68 | 0.6% (a) | 13 | 0.7% (a) | 0.6% |
| No answer | 73 | 0.7% | 6 | 0.3% | 0.6% |
| Did you miss your daily dose of ARB three days ago? | ARB in combination | ARB monotherapy | Total | ||
| No | 10,081 | 96% (a) | 1883 | 95.1% (b) | 95.8% |
| Yes | 144 | 1.4% (a) | 30 | 1.5% (a) | 1.4% |
| I don’t know | 204 | 1.9% (a) | 59 | 3.0% (b) | 2.1% |
| No answer | 75 | 0.7% | 7 | 0.4% | 0.7% |
| How many daily ARB doses have you missed during last 2 weeks? | ARB in combination | ARB monotherapy | Total | ||
| No dose | 9446 | 89.9% (a) | 1781 | 90% (a) | 89.9% |
| 1 dose | 616 | 5.9% (a) | 96 | 4.9% (a) | 5.7% |
| 2 or more doses | 114 | 1.1% (a) | 30 | 1.5% (a) | 1.2% |
| I don’t know | 225 | 2.1% (a) | 62 | 3.1% (b) | 2.3% |
| No answer | 103 | 1% | 10 | 0.5% | 0.9% |
| When was the last time when you missed a daily dose of ARB ? | ARB in combination | ARB monotherapy | Total | ||
| Today | 215 | 2% (a) | 28 | 1.4% (a) | 1.9% |
| Yesterday | 140 | 1.3% (a) | 27 | 1.4% (a) | 1.3% |
| This week | 265 | 2.5% (a) | 47 | 2.4% (a) | 2.5% |
| Last week | 617 | 5.9% (a) | 92 | 4.6% (b) | 5.7% |
| Less than 1 month ago | 334 | 3.2% (a) | 54 | 2.7% (a) | 3.1% |
| More than 1 month ago | 511 | 4.9% (a) | 75 | 3.8% (b) | 4.7% |
| Never | 7496 | 71.4% (a) | 1515 | 76.6% (b) | 72.2% |
| I don’t know | 832 | 7.9% (a) | 130 | 6.6% (b) | 7.7% |
| No answer | 94 | 0.9% | 11 | 0.6% | 0.8% |
Medication Possession Rate (MPR) was evaluated in relation with the answers given to the last questions of the adapted questionnaire: What is the approximate percentage of the total ARB daily doses that you have been taking during the last month?
According to the answers to this question, in 1912 (96.6%) of the patients who have been recommended ARB in monotherapy and in 10,136 (96.5%) of those with ARB in combinations, it has been registered a MPR above 80%, value considered the inferior level of adherence to anti HTN therapy.
DISCUSSION
Hypertension, defined as a systolic blood pressure (SBP) ≥140 mmHg and/or a diastolic blood pressure (DBP) ≥90 mmHg, is one of the most important preventable causes of premature death worldwide, contributing to approximately half of all global cardiovascular disease5. In many countries, up to 30% of adults have hypertension; cardiovascular disease incidence doubles for every 10 mmHg increase in DBP or every 20 mmHg increase in SBP20.
Blood pressure can be reduced either by lifestyle interventions or by pharmacotherapy to obtain the best outcome for the patient21.
Adequate measurement of BP is the most-important requirement for the diagnosis and treatment of patients with suspected hypertension. The use of methodologies such as ambulatory and home BP monitoring have become powerful tools for defining the ‘real’ BP of patients.
An important issue reffers to following the physician’s therapy by the patient. Nonadherence to antihypertensive treatment is a common problem in cardiovascular prevention and may influence prognosis.
Data published in 2009 by Mazzaglia et al., on newly diagnosed hypertensive patients initially free of cardiovascular diseases, obtained from 400 Italian primary care physicians, showed that only high adherence to treatment (proportion of days covered, ≥80%), significantly decreased risk of acute cardiovascular events22. Adherence to prescription, investigated based on a questionnaire in a female population aged 35-65 years in Sweden, revealed that age, scheduled check-up, perceived importance of medication, concerns about medication safety and taking medication for a respiratory or a cardiovascular disease were significantly related to adherence. Adherence ranged from 15-98% being the lowest among young women who regarded their medication as unimportant and who had no scheduled check-up and the highest among elderly women who regarded their medication as important and who had a scheduled check-up23. Adherence is better when the patient accepts the severity of his/her illness, trusts the therapist and believes in the effectiveness of the recommended therapeutic measures. Non-adherence is, among other factors, negatively associated with the level of education. Another important factors influencing adherence include the affordability of the therapy and the susceptibility to adverse effects of drugs in individual patients15.
ARBs adherence was previously studied evaluating persistence in newly diagnosed hypertensive patients who were initiated on irbesartan. Patients on irbesartan had statistically significant higher persistence (of 60.8% for monotherapy and of 76.8% for either monotherapy or in combinations), followed by patients who were initiated on all other ARBs with a persistence rate of 51.3% (74.9% either as monotherapy or in combination). Diuretics scored lowest with a persistence rate of 34.4% (65.5% either as monotherapy or in combinations) at 1 year24.
In a more recent study adressing persistence with antihypertensive treatments for a period of 3 years, Hasford et al. concluded that persistence differs markedly among the drug classes (p≤0.001) but even persistence of the best drug class is not sufficient to provide an adequate blood pressure control in the population. The largest decline in persistence occurs in the first 3 months of treatment. In our study the patients were already persistent on ARB treatment for 6 months, aspect which may explain the high level of compliance.
In Hasford at al. study, persistence with the initially prescribed antihypertensive treatment was significantly different (p<0.001) and longest for patients whose initial prescription was for a free combination based on ACEIs, followed patients initially receiving a fixed combination, including ARBs and ARBs monotherapy. Persistence was shortest with diuretics25.
Our study was addressing compliance and show high compliance rate to ARBs in a population persistent on this treatment for at least 6 months and also demonstrate that urban environment, possibly in relation with the level of education, and history of coronary disease are positively corelated with adherence to ARBs. None of the other factors including age, gender, hypertension duration, history of cerebrovascular diseases, diabetes mellitus or heart failure influenced significantly the adherence to ARB treatment in our study.
The comparison between the answers to adapted MASRI questionnaire given by the group of patients with ARBs monotherapy vs. ARBs in combinations has been performed using Chi-Square Test. Differences statistically significant between these subgroups have been identified for the patients who didn’t miss (higher % in combination group) and those who didn’t know if they missed (higher % in monotherapy group) the daily dose of ARB 3 days before, for those who didn’t know how many daily ARB doses have missed during last 2 weeks (higher % in monotherapy group), and for those for whom the last day when they missed a daily ARB dose was last week or more than a month before (higher % in combination group), or never (higher % in monotherapy group) or who didn’t know the answer (higher % in combination group).
Our study was based on a questionnaire filled in by patients. An aspect that should be considered is that physicians generally overestimate the level of adherence to therapy. Poor adherence should be suspected in those whose blood pressure appears resistant to treatment. Monitoring prescription refills and pill-counting are of value when nonadherence is suspected but can be unreliable in patients who wish to avoid admitting their failure to adhere to prescribed regimens26.
A limitation of this retrospective registry is that the concept of adherence was separated in two parts – persistence being part of the inclusion criteria and compliance part of the primary objective and the purpose of the registry was to analyse the compliance with ARBs treatment in an already persistent population. Another limitation is that medication adherence appeared to be higher when measured using self-reported questionnaires than when measured using electronic monitoring devices. This questionnaires are subject to measurement bias such as social desirability, recall bias and response bias17. There are mixed reports about the accuracy of self reported adherence, compared with the Medication Event Monitoring System –monitored adherence. MASRI questionnaire used in our study is one of the most commonly used and have shown good validity with Medication Event Monitoring System.
CONCLUSIONS
Our study showed a very good compliance with ARB treatment in hypertensive patients persistent on ARB treatment for 6 month, in ambulatory practice. The level of Medication Possession Rate (MPR) above 80%, has been registered in 96.5% of the patients with ARBs treatment, even in monotherapy or in combinations.
The following factors potentially associated with compliance with ARB therapy have been evaluated for those sub-groups of patients (ARB monotherapy and in combinations): age (with 50 years as threshold), gender, living environment (urban / rural), hypertension duration, history of coronary or cerebrovascular diseases, diabetes mellitus and heart failure. None of these individual factors influenced significantly the compliance with ARB treatment.
In the subgroup of patients with ARBs monotherapy the potential factors evaluated did not significantly influence patients compliance with the recommended treatment. In the subgroup of patients with ARBs in combinations urban environment determined significantly higher compliance than rural environment (RR = 1.093, CI = 1.018-1.173).
The logistic regression calculation (taking into account all these potential factors simultaneously) identified that patients living in urban area (p=0.017) and those with history of coronary disease (p=0.025) have a significantly better treatment compliance with ARB treatment.
This research was funded by Sanofi.
Conflict of interests:
D.Gherasim: Speaker fees from Novartis and Les Laboratoires Servier for case presentations
M. Iurciuc: None declared.
Cristina Voiculet: Speaker fees from Astra Zeneca for case presentations
Alina Giucă: Speaker fees from Novartis, Les Laboratoires Servier and Astra Zeneca LTD for case presentation
V. Petrescu: Speaker fees from Astra Zeneca, Boehringer-Ingelheim and KRKA for case presentations
F. Maghiar: None declared.
Alexandra Gherghină: Speaker fees from Astra Zeneca, Les Laboratoires Servier and Berlin Chemie for case presentations
A.Tase: Research fees from Les Laboratoires Servier, Sanofi and Novartis
Carmen Ginghină: None declared.
References
1. The World health statistics – Geneva 2012 report http://www.who.int/mediacentre/news/releases/2012/world_health_statistics_20120516/en/index.html
2. Dorobanţu M, Darabont R, Ghiorghe S, Babes K, Pop D, Toma D, Vasilescu M, Dobreanu M, Tăutu O. Profile of the Romanian Hypertensive Patient Data from SEPHAR II Study. Rom. J. Intern. Med., 2012, 50, 4, 285-296.
3. Ginghină C, Popescu B, Şerban M, et al.The Prevalence of hypertension and left ventricular hypertrophy in a Romanian population. A clinical – echocardiographic study. J. Hypertension, vol.22, suppl 2, June 2004, S307.
4. Apetrei E, Kulcsar I, Stănescu Cioranu Rodica, Matei C, Cochino E, Ginghină C. Studiul Urziceni-Studiu populaţional retrospectiv de depistare a factorilor de risc pentru bolile cardiovasculare şi intervenţie în populaţie, depistarea precoce a bolilor cardiovasculare. Revista Română de Cardiologie, vol.XXIII, Nr.2, 2008, p.136-145.
5. Kjeldsen S, Aksnes T, Fagard R, Mancia G. Hypertension in The ESC Textbook of Cardiovascular Medicine (2 ed.), edited by Camm AJ, Luscher T, Serruys P, Oxford University Press 2009.
6. 2007 Guidelines for the management of arterial hypertension European Heart Journal 2007; 28: 1462-1536.
7. Sever PS, Messerli FH. Hypertension management 2011: optimal combination therapy. European Heart Journal 2011p; 32: 2499-2506.
8. Kobori H, Nangaku M, Navar LG, Nishiyama A. The Intrarenal Renin-Angiotensin System: From Physiology to the Pathobiology of Hypertension and Kidney Disease. Pharmacol Rev 2007; 59:251-287.
9. Wong J, Patel RA, Kowey PR. The clinical use of angiotensin-converting enzyme inhibitors. Prog Cardiovasc Dis 2004; 47:116-130.
10. Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet 2003; 362:1527-1535.
11. Staessen JA, Wang JG, Thijs L. Cardiovascular prevention and blood pressure reduction: a quantitative overview updated until 1 March 2003. J Hypertens 2003; 21:1055-1076.
12. Messerli F, Williams B, Ritz E. Essential hypertension. Lancet 2007; 370:591-603.
13. Burnier M. Medication adherence and persistence as the cornerstone of effective antihypertensive therapy. Am J Hypertens. 2006;19:1190-1196.
14. Van Wijk BLG., Klungel OH, Heerdink ER, de Boer A. Rate and determinants of 10-year persistence with antihypertensive drugs. J Hypertens 2005;23:2101-7.
15. Laufs U, Rettig-Ewen V, Böhm M. Strategies to improve drug adherence. European Heart Journal 2011; 32: 264-268.
16. Cramer JA, Roy A, Burrell A, Fairchild CJ, Fuldeore MJ, Ollendorf DA, Wong P K. Medication Compliance and Persistence: Terminology and Definitions. Value in health 2008;11:44-47.
17. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;
353:487-497.
18. Ho P. M., Bryson C. L., Rumsfeld J. S. Medication Adherence Its Importance in Cardiovascular Outcomes. Circulation. 2009;119:3028-3035.
19. Shi L, Liu J, Koleva Y, Fonseca V, Kalsekar A, Pawaskar M. Concordance of Adherence Measurement Using Self-Reported Adherence Questionnaires and Medication Monitoring Devices. Pharmacoeconomics 2010; 28 (12): 1097-1107.
20. Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360:1903-13.
21. Ruilope L. M. Current challenges in the clinical management of hypertension. Nat. Rev. Cardiol. 2012; 9:267-275.
22. Mazzaglia G, Ambrosioni E, Alacqua M, Filippi A, Sessa E, Immordino V, Borghi C, Brignoli O, Caputi AP, Cricelli C, Mantovani LG. Adherence to Antihypertensive Medications and Cardiovascular Morbidity Among Newly Diagnosed Hypertensive Patients. Circulation 2009;120:1598-1605.
23. Bardel A,Wallander MA, Svardsudd K. Factors associated with adherence to drug therapy: a population-based study. Eur J Clin Pharmacol 2007;63:307-314.
24. Hasford J, Mimran A, Simons WR. A population-based European cohort study of persistence in newly diagnosed hypertensive patients. Journal of Human Hypertension 2002; 16: 569-575.
25. Hasford J, Schröder-Bernhardi D, Rottenkolber M, Kostev K, Dietlein G. Persistence with antihypertensive treatments:results of a 3-year follow-up cohort study. Eur J Clin Pharmacol 2007; 63:1055-1061.
26. Chobanian AV. Impact of Nonadherence to Antihypertensive Therapy. Circulation 2009;120:1558-1560.
 This work is licensed under a
This work is licensed under a