Naomi Niari Dalimunthe1, Sari Harahap1, Rahmad Isnanta1, Zainal Safri1, Refli Hasan1
1 Division of Cardiovascular, Department of Internal Medicine Faculty of Medicine, Sumatera Utara University, Indonesia
Abstract: Background – Hyponatremia is a common electrolyte disorder among patients with heart failure and associated with poor clinical outcomes. This study aims to assess the prevalence and clinical outcomes in hyponatremia compared to normonatremia patients hospitalized for heart failure. Methods – This was a cohort retrospective study using medical record of patients hospitalized for heart failure between January and December 2015 in Adam Malik Hospital, Medan, Indonesia. Patients were assigned to one of two groups; hyponatremia with admission serum sodium <135 mg/dl or normonatremia with admission serum sodium ≥135 mg/dl. Differences in variables between two groups were evaluated using chi-square test for categorical variables and independent samples t test or Mann Whitney U test for continuous variables. Furthermore, hyponatremia group was classified into mild, moderate and severe to analyses outcomes based on severity of hyponatremia. Results – Of 497 patients, hyponatremia was present in 230 patients (46.27%) with mean admissions serum sodium 129.16±5.17 mg/dl. Patients with hyponatremia had signifi cantly higher in-hospital mortality (p=0.034, OR=1.999, 95% CI 1.044-3.828) and longer hospital stays (p=0.023) compared to normonatremia but no difference in readmission rate was observed between groups (p=0.414). Among hyponatremia groups, severe hyponatremia had worse clinical outcomes, with highest in-hospital mortality (19.35%) and longest length of stays (11.16±8.04 days). Conclusions – Hyponatremia was a relatively common condition found in patients hospitalized for heart failure and associated with higher in-hospital mortality and longer hospital stays. Poorer clinical outcomes were observed in severe hyponatremia group.
Keywords: Hyponatremia; heart failure; in-hospital mortality; length of stays; readmission.
INTRODUCTION
Hyponatremia defined as serum sodium concentration <135 mEq/L is one of the major electrolyte disorders in-hospitalized patients1 . Prevalence of hyponatremia in heart failure patients ranges from 4-45%2 , in the Organized Program to initiate Lifesaving Treatment in-hospitalized Patients with Heart Failure (OPTIMIZE-HF) study 20% of patients present with hyponatremia while in Acute and Chronic Therapeutic Impact of a Vasopressin Antagonist in Congestive Heart Failure (ACTIV in CHF) trial 21% heart failure patients hospitalized with hyponatremia2 . Hyponatremia has repeatedly been shown to be a marker of increased morbidity and mortality in heart failure population. Several previous study demonstrated that both admission and hospitalized acquired hyponatremia are associated with and increase adverse outcomes including prolonged hospital length of stays, frequent rehospitalization, and associated with increased in-hospital and post discharge mortality3 . In daily clinical practice, hyponatremia has not been considered significant unless the serum sodium was <125 mg/dl. However, in heart failure population even mild hyponatremia has been recognized as a risk factors for poor prognosis4 . Therefore this study aims to assess the prevalence and severity of hyponatremia and evaluate the relationship among admission serum sodium, patients characteristic and clinical outcomes among patients hospitalized for heart failure.
MATERIAL AND METHODS
This was a cohort retrospective study using medical record of patients hospitalized for heart failure between January and December 2015 in Adam Malik Hospital, Medan, Indonesia. Eligible patients were enrolled if they were at least 18 years and diagnosed with heart failure according to the clinical practice guidelines of European Society of Cardiology based on the presence of heart failure symptoms and signs5 . Detailed clinical data were collected regarding patients characteristics, laboratories, echocardiography variables and co morbidities. Serum sodium concentration was recorded at the day of hospital admission. Patients were categorized to one of two groups; hyponatremia with admission serum sodium <135 mg/dl or normonatremia with admission serum sodium ≥135 mg/dl. Furthermore, hyponatremia group was classifi ed into mild (serum sodium 130-134 mg/dl), moderate (serum sodium 125- 129 mg/dl) and severe (serum sodium <125 mg/dl) to analyses outcomes based on severity of hyponatremia. Means, standard deviations and percentages were used to describe the characteristics of study population. Differences in variables between groups were evaluated using chi-square test for categorical variables and independent samples t test or Mann Whitney U test for continuous variables. A value of p<0.05 was considered statistically significant.
RESULTS
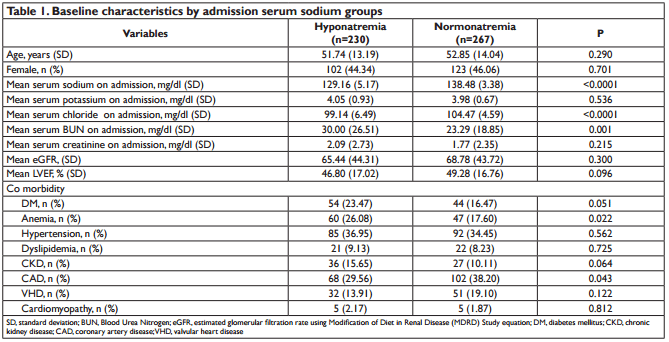
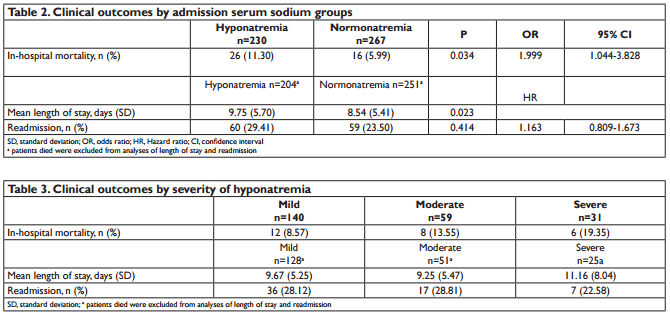
A total of 610 patients diagnosed with heart failure during period of study, of which 113 patients were excluded do to missing data. From 497 patients eligible for this study, hyponatremia was present in 230 patients (46.27%) with mean admissions serum sodium 129.16±5.17 mg/dl. Patients mean age were similar in the two groups (51.74 and 52.86; p=0.290) and no gender predominance were found between groups. Patients in hyponatremia groups were statistically had lower serum chloride and higher blood urea nitrogen. No difference in ejection fraction were found between groups, both groups had ejection fraction <50% (p=0.096). Anemia was more profound in hyponatremia groups, while coronary artery disease frequently found in normonatremia groups. Analysis of other cardiovascular risk factor and co morbidities revealed no statistically significant differences. The characteristics of two groups are shown in Table 1. Hyponatremia was associated with higher in-hospital mortality (p=0.034, OR=1.999, 95% CI 1.044- 3.828) and longer hospital stays (p=0.023) compared to normonatremia. No difference in readmission rate was observed between groups (p=0.414, HR 1.163, 95% CI 0.809-1.673) as shown in Table 2. Among hyponatremia groups, severe hyponatremia had worse clinical outcomes, with highest in-hospital mortality (19.35%) and longest length of stays (11.16±8.04 days) as shown in Table 3.
DISCUSSIONS
Heart failure represent a major public health problem due to high in-hospital and post discharge mortality, longer length of stay, frequent hospital readmission and that has significant association with higher medical cost. Several prognostic markers has been associated with poor adverse outcomes in heart failure patients such as age, functional class of heart failure, low blood pressure, higher blood urea nitrogen (BUN) and hyponatremia6,7. Identifi cation of these predictors could potentially aid in making clinical decision and help patients who might benefit from aggressive monitoring and intervention7,8.
Hyponatremia on hospital admission is a relatively common condition in patients hospitalized for heart failure. Previous studies reported 19-25% of heart failure patients have hyponatremia, while this study found 46.27% of patients in hyponatremia groups2 . Hyponatremia often parallels the severity of cardiac dysfunction while this study was conducted in a tertiary hospital which received referral patients with severe conditions could explain higher prevalence of hyponatremia found in this study. OPTIMIZE-HF study reported that patients in hypo natremia groups were clinically similar with patients in normonatremia groups in terms of age, gender, heart failure etiology, diabetes, heart rate, ejection fraction and symptom of congestion9 . Previous study by Lu D, et al found that patients with hyponatremia were older, more likely to have diabetes, hypertension and stroke but no difference in sex distribution, left ventricular ejection fraction and presence of coronary artery disease10. Baseline characteristic of age, gender, ejection fraction and creatinine in this study were not significantly different between hyponatremia and normonatremia groups. Hyponatremia groups were more likely to have higher blood urea nitrogen, lower serum chloride, higher cases of anemia but fewer cases of coronary artery disease. This study found that blood urea nitrogen was higher in hyponatremia group compared to normonatremia. Lower serum sodium was associated with more severe heart failure which also correlated with higher blood urea nitrogen. Reduction in renal perfusion, renin angiotensin aldosterone and sympathetic activation lead to increased sodium and water reabsorption that is coupled with enhanced urea reabsorption in proximal tubules7 . Vasopressin on binding to V2 receptors in the inner medullary collecting ducts increases urea permeability though activation of urea transporter which enables its reabsorption7 . Admission chloride levels were directly correlated to admission sodium levels as we found in this study. Serum chloride act as a buffer for cations including acid and sodium therefore had a role in the kidney’s ability to eliminate salt and water. Although not completely understood, chloride might represent the downstream effect of adverse prognostic maladaptive neurohormonal, renal and acid base disturbance in heart failure11. In this study, hyponatremia groups had higher anemia cases than normonatremia groups. Renal dysfunction, neurohormonal and proinfl ammatory cytokine activation found in heart failure participate in the development of anemia. While on the other hand anemia increases myocardial workload and worsen cardiac dysfunction12. This study demonstrated that the more severe the hyponatremia, the poorer the outcome. This fi ndings were similar with the result of OPTIMIZE-HF registry which conclude that hyponatremia is associated with longer hospital stays and higher in-hospital mortality and early post discharge mortality9 . In the OPTIMIZEHF, the in-hospital and post discharge mortality risk increased 19.5% and 10.0% for each 3 mg/dl decreased in serum sodium up to 140 mg/dl after adjustment for other prognostic variables9 . The underlying pathophysiology of hyponatremia related to mortality is still unclear, whether hyponatremia is an active contributor to poor clinical outcomes in heart failure or it is simply reflects a more advanced disease. Decrease stimulation of mechanoreceptors in the left ventricle, carotid sinus, aortic arch and renal afferent arterioles in heart failure patients leads to increased neurohormonal activation such as sympathetic nervous system, renin angiotensin aldosterone system and non osmotic release of vasopressin8,7. Increased sympathetic drive contributes to sodium and water retention through renal vasoconstriction, stimulation of renin angiotensin aldosterone system and direct effect on the proximal convulated tubules. Increase angiotensin II and aldosterone levels lead to decreased sodium and water delivery to the collecting duct which combined with resistance to the action of natriuretic peptides, results in impairment of free water excretion and hyponatremia3,7. The non osmotic stimulation of vasopressin released results in an increased number of aquaporin water channels in the collecting duct of the kidney that promote abnormal free water retention and contribute to the development of hyponatremia. This raised the hypothesis that low serum sodium may be a marker of neurohormonal activation refl ecting the severity of heart failure. Moreover, this study adds the information that poorer clinical outcomes found in a more severe hyponatremia state. There were several limitations in the present study. First, this study conducted in a single tertiary hospital which may led to selection bias given that patients were more likely in severe conditions. Second, patient’s clinical characteristics and medication history were not recorded in this present study. Third, this study could not differentiate patient’s fl uid and hyponatremia status, whether in euvolemic, hypervolemic or normovolemic state3 .
CONCLUSIONS
Hyponatremia was a relatively common condition found in patients hospitalized for heart failure and associated with higher in-hospital mortality and longer hospital stays. Poorer clinical outcomes were observed in severe hyponatremia group.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial or not-for profit sectors.
Conficts of interest: The authors have no conflicts of interest to declare.
References
1. Wald R, Jaber BL, Price LL, Upadhyay A, Madias NE. Impact of hospital-associated hyponatremia on selected outcomes. Arch Intern Med 2010;170:294–302. doi:10.1001/archinternmed.2009.513.
2. Jao GT, Chiong JR. Hyponatremia in acute decompensated heart failure: Mechanisms, prognosis, and treatment options. Clin Cardiol 2010;33:666–71. doi:10.1002/clc.20822.
3. Verbrugge FH, Steels P, Grieten L, Nijst P, Tang WHW, Mullens W. Hyponatremia in acute decompensated heart failure: Depletion versus dilution. J Am Coll Cardiol 2015;65:480–92. doi:10.1016/j.jacc.2014.12.010.
4. Diaconu CC, Bartoş D. Frequency and Outcomes of Hyponatremic Patients with Heart Failure Hospitalized in the Clinical Emergency Hospital of Bucharest n.d.
5. Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJV, Ponikowski P, Poole-Wilson PA, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008‡. Eur J Heart Fail 2008;10:933–89. doi:http://dx.doi.org/10.1093/eurheartj/ehw128.
6. Abraham WT, Fonarow GC, Albert NM, Stough WG, Gheorghiade M, Greenberg BH, et al. Predictors of In-Hospital Mortality in Patients Hospitalized for Heart Failure. Insights From the Organized Program to Initiate Lifesaving Treatment in-hospitalized Patients With Heart Failure (OPTIMIZE-HF). J Am Coll Cardiol 2008;52:347–56. doi:10.1016/j.jacc.2008.04.028.
7. Klein L, Connor CMO, Leimberger JD, Gattis-stough W, Piña IL, Felker GM, et al. Short-Term Mortality in-hospitalized Patients With Worsening Heart Failure Results From the Outcomes of a Prospective Trial of Intravenous Milrinone for Exacerbations of Chronic Heart Failure ( OPTIME-CHF ) Study. Circulation 2005;111:2454–61. doi:10.1161/01.CIR.0000165065.82609.3D.
8. Romanovsky A, Bagshaw S, Rosner MH. Hyponatremia and congestive heart failure: a marker of increased mortality and a target for therapy. Int J Nephrol 2011;2011:732746. doi:10.4061/2011/732746.
9. Gheorghiade M, Abraham WT, Albert NM, Gattis Stough W, Greenberg BH, O’Connor CM, et al. Relationship between admission serum sodium concentration and clinical outcomes in patients hospitalized for heart failure: An analysis from the OPTIMIZE-HF registry. Eur Heart J 2007;28:980–8. doi:10.1093/eurheartj/ehl542.
10. Lu D, Cheng H, Cheng Y, Hsu P, Huang W, Guo C, et al. Hyponatremia and Worsening Sodium Levels Are Associated With n.d.:1–9. doi:10.1161/JAHA.115.002668.
11. Grodin JL, Simon J, Hachamovitch R, Wu Y, Jackson G, Halkar M, et al. Prognostic Role of Serum Chloride Levels in Acute Decompensated Heart Failure. J Am Coll Cardiol 2015;66:659–66. doi:10.1016/j. jacc.2015.06.007.
12. Alexandrakis MG, Tsirakis G. Anemia in Heart Failure Patients. ISRN Hematol 2012;2012:1–9. doi:10.5402/2012/246915.
 This work is licensed under a
This work is licensed under a