Smaranda Radu1, Mariana Floria1,2, Genoveva Livia Baroi1,2, Cristina Bocinca1, Anca Ouatu1,2, Daniela Maria Tanase1,2, Ovidiu Mitu1,2, Florin Mitu1,3
1 “Gr. T. Popa” University of Medicine and Pharmacy, Iasi, Romania.
2 “Sf. Spiridon” Emergency Hospital, Iasi, Romania.
3 Cardiology Clinic of Rehabilitation Hospital, Iasi, Romania.
Abstract: Nowadays the new concept in cardiovascular disease namely Heart Team, a multidisciplinary team created in tertiary hospitals to find the best medical care or to decide and assist complex surgical or percutaneous interventional cardiology procedures (e.g. for high risk patients with severe aortic stenosis referred to transcutaneous valve implantation or electrophysiology procedures) in patients with severe or life threating cardiac disease, might be created and function in all tertiary hospitals. Multidisciplinary collaboration between experts for early diagnosis and appropriate/optimal treatment might prevent or reduce long hospitalization, temporary or permanent incapacitation and implicitly social costs in coronary heart disease, valvulopathies, atrial fi brillation, infective endocarditis, heart failure, peripheral artery disease or congenital heart disease. Moreover new multidisciplinary teams like cardiometabolic team will be appearing. However, Heart Team concept, this useful tool for obtaining optimal clinical outcomes, has not been widely implemented. Delayed diagnosis and inappropriate treatment in the absence of a heart team might have medical, social, legal and ethical outcomes. This article underlies the utility and the limits of Heart Team, a multidisciplinary team of experts, created in tertiary hospitals involved in
complex medical care of patients with cardiovascular diseases. Keywords: heart team, multidisciplinary team, cardiology, complex medical care.
INTRODUCTION
For the first time described by John Venn in the 1880s, Venn diagrams can be useful for understanding the roles of various stakeholders in the management of cardiovascular disease from its diagnosis through its treatment1. The overlap of the Venn diagrams for interventional cardiology and cardiovascular surgery has grown larger since the promulgation of the multidisciplinary
Heart Team concept. In medical practice, multidisciplinary decision-making could improve both the level and the consistency of the care delivered. A pretreatment multidisciplinary discussion is reported to be an independent factor for treatment decisions to be in accordance with guidelines2. The area of overlap of the cardiovascular disease Venn diagram continues to expand.
Used for the first time for heart failure, pediatric and adult cases of congenital heart disease treatment, than for critical limb ischemia and myocardial revascularization, Heart Team was more recently introduced for aortic and mitral valve interventions and endocarditis. However the use of Heart Team was recently incorporated in some cardiology guidelines. Therefore multidisciplinary team for ischemic heart disease, valvulopathies, infective endocarditis, heart failure, peripheral artery disease or congenital heart disease should be created and should function in all tertiary hospitals. New multidisciplinary teams like cardiometabolic team seem to be necessary in clinical practice; however this is another type of multidisciplinary collaboration/management that applies to chronic medical care (similarly to cardiac rehabilitation team). The advent ages of a well-designed and functional heart team are: improved medical decision making (especially risk vs. benefit determinations) with collaborative input from multiple physicians on essentially every case; improved patient and family communication, leading to greater satisfaction with the knowledge of a multidisciplinary team approach; physician benefit by sharing the burden and liability during intense patient care experiences; improved access to and enrollment in clinical research studies; and overall improvement in team morale, active collaboration, and efficiencies in executing complex clinical care plans. Multidisciplinary collaboration
for early diagnosis and appropriate treatment might prevent or reduce long hospitalization, temporary or permanent incapacitation and implicitly social costs. In tertiary hospitals involved in complex medical care it could be a potential tool to avoid malpractice. Delayed diagnosis and appropriate treatment in the absence of a Heart Team could have medical, social, legal and ethical
outcomes.
Heart Team in coronary heart disease
Coronary revascularization by coronary artery bypass grafting or percutaneous coronary intervention improves both symptoms and survival in patients with signifi cant coronary artery disease3. The safety and efficacy of both procedures have been well established, but there is great variability in their use in clinical practice. Typically, and according to the guidelines, revascularization
is indicated if there is significant angiographic diameter stenosis (≥50–70%) with documented ischemia or fractional fl ow reserve <0.803. A useful tool when talking about surgical risk are risk scores for assessing operative mortality risk. The STS score and logistic EuroSCORE are the most commonly used models to assess the patient’s operative mortality risk3. A joint consensus between surgeons and cardiologists is required to assist in decision making for patients requiring elective coronary revascularization. A group composed of cardiac surgeons and interventional
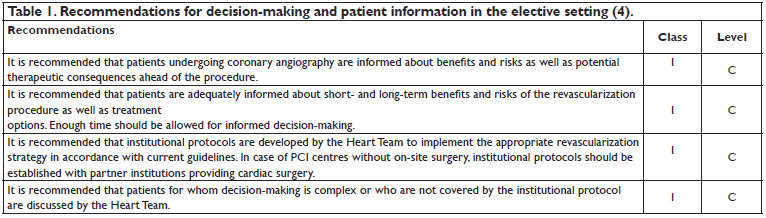
and non-interventional cardiologists has recently produced joint guidelines for the European Society of Cardiology and European Association for Cardiothoracic Surgery4. According to these guidelines, patients with stable coronary artery disease, those with 1- or 2-vessel disease, not involving the proximal left anterior descending artery, should be offered percutaneous coronary intervention4. More extensive disease involving the left main stem or proximal left anterior descending, or those with 3-vessel disease should be considered for coronary artery bypass grafting in the fi rst instance4. Specifi c mention is made of high-risk groups, including patients with chronic kidney disease, left ventricular failure, and diabetes, in whom surgery is the preferred option. All patients with coronary artery disease who are being considered for revascularization will undergo a diagnostic coronary angiogram. Intervention performed during this procedure is known as ad hoc percutaneous coronary intervention. The guidelines make a specific recommendation that stable patients should have intervention deferred. This allows discussion with a surgeon and provides time for the patient to understand the options available to them. Evidence suggests that the current decision-making process and treatment selection in stable complex coronary artery disease is questionable, thereby potentially resulting in suboptimal care and increased health care expenditures. Multidisciplinary decision-making has gained more emphasis over the recent years to select the most optimal treatment strategy for individual patients with stable complex coronary artery disease5. Multidisciplinary Heart Team for patients with stable complex coronary artery disease consisting of at least a clinical/non-invasive cardiologist, interventional cardiologist, and cardiac surgeon that together can better analyze and interpret the available diagnostic evidence,
put into context the clinical condition of the patient as well as consider individual preference and local expertise, and through shared decision-making with the patient can arrive at a most optimal joint treatment strategy recommendation (Table 1).
The European Society of Cardiology and European Association for Cardiothoracic Surgery Guidelines place particular emphasis on a multidisciplinary approach and suggest that a Heart Team containing both cardiologists and surgeons discuss complex patients before intervention. Furthermore, patients being treated against the guidelines, for whatever reason, should be discussed with the Heart Team before intervention. While decision-making for patients with acute indications or less complex coronary disease may be straightforward, for patients with stable complex coronary
artery disease, a Heart Team consisting of a clinical/non-invasive cardiologist, interventional cardiologist, and cardiac surgeon is considered optimal to best assess the advantages and disadvantages of the various treatment strategies. The development of a Heart Team and blending the disciplines of cardiology and cardio-thoracic surgery was deemed to enhance optimal patient selection, procedural performance and outcome. This Heart Team approach has been codifi ed in the European Society of Cardiology/European Association for Cardio-Thoracic Surgery guidelines on Myocardial Revascularization, which recommend that patients with stable complex coronary artery disease be seen by a Heart Team, which includes cardiovascular surgeons and interventional cardiologists6. The 2011 Heart Team has become a class 1C recommendation in European and American guidelines on myocardial revascularization3,4. Working together, a team composed of
a surgeon, an interventional cardiologist, a primary cardiologist, and the patient agreed upon the optimal revascularization strategy. A multidisciplinary Heart Team approach as well as a multi-modality imaging assessing of post infarction ventricular septal defect, a life threating complication of myocardial infarction, is necessary for selecting the appropriate closure device and for successful deployment of the percutaneous occluder7. However, in some cases, it provides time to allow the ventricular septum defect to mature and the patient to stabilize and be optimized acting as a bridge to surgery to offer the best possible outcome for the patient8. The structured Heart Team approach is an effective tool for ad hoc and conference-based clinical decisionmaking
with a sustained clinical benefit9, demonstrated by a low late coronary bypass grafting (and percutaneous coronary intervention) rates after a first percutaneous coronary intervention, without elevated mortality9. Heart failure secondary to coronary artery disease, also known as ischemic cardiomyopathy, is an important cardiovascular condition that has a signifi cant impact on both morbidity and mortality that is managed across different disciplines within the field of cardiology. There is no trial data to support revascularization in all patients with ischemic cardiomyopathy, but demonstration of coronary artery disease and myocardial viability can be important for both future management and prognostic purposes. There is a large body of observational data that suggests a mortality benefit with revascularization in patients with ischemic cardiomyopathy. However, STICH trial underscores the benefit of revascularization in all patients with ischemic
cardiomyopathy with proved myocardial viability10. There are different factors that may predict benefit from revascularization like severity of left ventricular dysfunction, severity of coronary artery disease, evidence of viability and presence or absence of ischemia; the role of Heart Team in the management of this complex and high-risk group of patients to ultimately improve outcomes is very important. The optimal revascularization strategy of patients with multivessel coronary artery disease, a common condition in clinical practice, is infl uenced by the clinical situation, comorbid conditions, and anatomical variables. Data continue to emerge on the potential benefi ts of complete revascularization on clinical outcomes and suggest that complete revascularization should be the goal of therapy whenever possible. However, there are several defi nitions of what constitutes a complete revascularization procedure12. The heart team should carefully review the degree to which each revascularization modality can achieve this goal during procedural planning.
Heart Team in valvular heart disease
The complexity of diagnosing and managing patients with severe symptomatic valvular disease (especially aortic stenosis) and multiple comorbidities in the elderly population has required the combined efforts of multiple subspecialties. A structured Heart Team guidance for surgical replacement, percutaneous implantation or medical treatment is now generally accepted and recommended in current guidelines, at least for patients with severe comorbidities and high operative risk mortality (assessed by risk scores like EUROSCORE II or STS score). The routine use of a heart valve team (in essentially every case) is now the guideline- recommended approach for percutaneous aortic valve replacement and is a Class I indication in both the ACC/AHA and the European Society of Cardiology guidelines13,14. For a precise diagnosis subspecialists are used as members of the heart valve team, including clinical cardiologists, cardiac surgeons, interventional cardiologists, imaging experts (echocardiography and computed tomography), anesthesiologists, geriatricians, intensive care specialists, and other medical specialists (e.g., neurologists, nephrologists). In addition, a vital component of the heart valve team involves a dedicated and custom-trained group of non-physician health care specialists, such as hospital administrators, nurse coordinators, nurse practitioners and physician assistants, physical therapists, social service experts, and clinical research personnel. Surgical valve replacement has evolved over the past 50 years as the standard-of-care in patients with severe symptomatic valvular disease. Minimally invasive aortic valve replacement and minimally invasive mitral valve surgery have proved to be safe alternatives for conventional surgery in terms of mortality and complications over the past two decades. Consensus has not yet been reached regarding absolute contraindications
for minimally invasive mitral valve surgery due to both differences in surgical and perfusion techniques, as well as different approaches used by surgeons and centers. It has therefore been diffi cult to test potential superiority of the minimally invasive technique over conventional surgery. However, with the emergence of a new concept of individualization of patient care, the focus will shift from whether a minimally invasive procedure is better than conventional treatment, to the question of which patients will benefi t most from which technique. Percutaneous aortic valve implantation has now been fully integrated into the therapeutic armamentarium for managing aortic stenosis in patients who are not good candidates for conventional surgery and are either denied surgery or are at high risk for complications and protracted recovery. Heart Team concept has also been employed in the fi eld of aortic stenosis and transcatheter aortic valve implantation. The team approach adopted in France, including standardized medical therapy, surgical indications following guideline recommendations and 1 year of close follow-up, has been shown to significantly reduce the 1-year mortality15. Recently was shown that TAVI is feasible and has comparable results to surgery in terms of early, 1-year mortality, as well as cerebrovascular events in patients with severe aortic stenosis and intermediate-low operative risk16. Heart Team conferences are also important tools in cases of valvular and end-stage heart disease8.
Heart Team in infective endocarditis
No single practitioner will be able to manage and treat a patient in whom the main clinical symptoms might be cardiac, rheumatologic, infectious, neurological or other. Infective endocarditis, through its types of clinic manifestation, lays many diagnosis traps for the infectious disease specialist, neurologist, internal medicine specialist and even for the cardiologist. Stroke is one
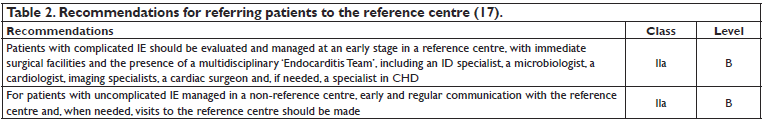
of the most severe complications of this disease, which affects the short and long term prognosis. A stroke in febrile context asks for a complete exam with the collaboration of the cardiologist, infectious disease specialist, microbiologist, imaging specialist, cardiac surgeon and sometimes of the interventional cardiologist. Recently, new endocarditis guidelines were published17.
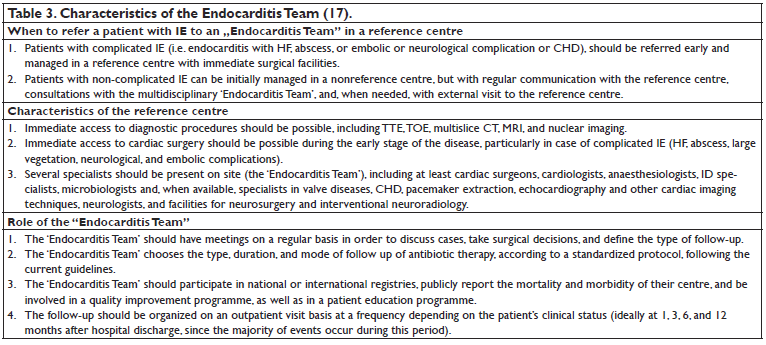
A very high level of expertise from several specialties practitioners including cardiologists, cardiac surgeons, imaging specialists, microbiologists, neurologists, neurosurgeons, experts in coronary heart disease and others, is needed17. It is very clearly noted that patients should be evaluated and managed at an early stage in a reference center (Table 2), with immediate surgical facilities and the presence of a multidisciplinary team, the Endocarditis Team (Table 3)17. The statement that the Heart Team should include a cardiologist, an infectious disease specialist, a microbiologist, imaging specialist, a cardiac surgeon, cardiovascular anesthetist, neurologist or nephrologist (if necessary) may have multiples effects in clinical practice with consequences in the malpractice fi eld.
Heart Team in heart failure
There are several types of HF according to the ejection fraction of the left ventricle (LVEF); guidelines consider patients with a normal EF (>50%) to have HF with preserved EF (HFpEF) and those with an EF <40% to have HF with reduced EF (HFrEF)18. It is estimated that >10% of the population >70 years has HF19. Not only the incidence and prevalence are rising, but the costs for caring for such patients are high20. HF patients are mostly elderly; they have a great number of comorbities that, in the context of the underlining cardiovascular pathology, are difficult to manage. In patients with HFrEF, most of the hospitalizations are due to extra-cardiac causes18. The response to HF treatment is conditioned by accompanying disorders such as diabetes mellitus, obesity, respiratory infections (that are often a cause of congestion), chronic kidney disease. Comorbities affect HF treatment and also could lead to numerous drug interactions20. Also, the
numerous and variation causes of deterioration (cardiac and non-cardiac) require collaboration between several specialties21. Recent ESC guidelines suggest the use of a multidisciplinary
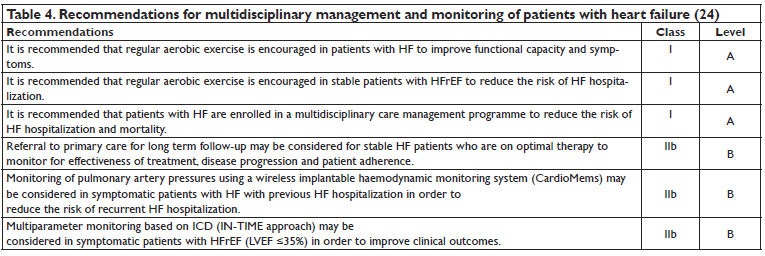
team in the management of patients with HF22-24. Implementing multidisciplinary management programs has shown to improve quality of life, reducing admission rates and mortality18. These programs link outpatient care to hospitals, requiring collaboration of general practitioners, primary cardiologists, HF nurse, geriatricians, internists, pharmacists, dieticians, physiotherapists, palliative care providers, social workers and psychologists. As patient’s compliance determines through the adherence to prescribed treatment the overall evolution and prognosis, the HF patient has to be closely monitored by his general practitioner. The coexistence of HF with dementia/degrading cognitive abilities strengthens the need for an interdisciplinary team. Attention should be given to the medication in use and the compliance to the therapeutic regimen. The Heart Team should also discuss with the family the option of palliative care. The decision to shift towards improving the quality of life should involve the patient, patient’s family, cardiologist, general practitioners, and nurse23. The use of a multidisciplinary team improves the patient’s quality of life and prognosis while making the healthcare system more effi cient: it lowers the costs, improves survival rates by reducing all-cause mortality to 25% and enhances specialists’ collaboration22,23. In older adult, frailty, with cognitive impairment, support from a multidisciplinary HF team in collaboration with specialist dementia support teams, alongside medication compliance aids, tailored self-care advice and involvement of family and caregivers, may improve adherence with complex HF medication and self-care regimens23. Multidisciplinary team management of heart failure is recommended by the brand new ESC guidelines; these teams “should employ a multidisciplinary approach (cardiologists, primary care physicians, nurses, pharmacists, physiotherapists, dieticians, social workers, surgeons, psychologists, etc.), should target high-risk symptomatic patients, should include competent and professionally educated staff”24. According with these
guidelines multidisciplinary management programs are designed to improve outcomes through structured follow-up with patient education, optimization of medical treatment, psychosocial support and improved access to care (Table 4)24. Cardiac resynchronization therapy (CRT) is indicated to lower the morbidity and mortality of patients presenting with symptomatic heart failure in sinus rhythm with a QRS duration ≥150 msec or 130–149 msec and left bundle block brand QRS morphology and with LVEF ≤35% despite optimal medical therapy24,25. Over two decades after the introduction of CRT into clinical practice, ~30% of candidates continues to fail to respond to this highly effective treatment of drug-refractory heart failure26. There are potentially reversible causes of non-responders to CRT because of loss of biventricular stimulation due to competing arrhythmias (atrial or ventricular) and secondary mitral regurgitation. Atrial fibrillation and ventricular extrasystoles ablation seems to be an option for selected non-responder patients treated in highly experienced medical centers26. In addition, mitral clips and new percutaneous tricuspid valve therapies may contribute to the management of non-responders to CRT who present with severe, persistent secondary mitral or tricuspid regurgitation25. Among CRT system recipients, 50% suffer from ischemic cardiomyopathy25.
However the preventive role of coronary revascularization in non-responsive CRT patients is unknown. The prevention of non-responders to CRT is essential to improve the overall performance of this treatment and lower its risk–benefi t ratio. These objectives require collaborative efforts by the heart failure team, the electrophysiologist and the cardiac imaging experts25. Palliative and end-of-life care approaches include a focus on symptom management, emotional support and communication between the patient and his/her family24. Ideally this should be introduced early in the disease trajectory and increased as the disease progresses. A decision to alter the focus of care from modifying disease progression to optimizing quality of life should be made in discussion with the patient, cardiologist, nurse and general practitioner25. The patient’s family should be involved in such discussions if requested by the patient.
Multidisciplinary Team in critical limb ischemia
Peripheral arterial disease is accompanied by several comorbidities and complications. Critical limb ischemia is defi ned as a triad of symptoms comprising of rest pain, gangrene and ulcerations, as a severe manifestation of peripheral artery disease. Critical limb ischemia should be differentiated from acute limb ischemia by the persistence of symptoms for at least two weeks. The severe ischemia leads to tissue loss caused by intractable ulcers and gangrene. It is generally admitted that ischemic tissue loss occurs below an ankle pressure of 70 mm Hg or toe pressure below 50 mm
Hg26. Studies show that critical limb ischemia patients have a 1-year mortality of 25%27. Patients suffering from critical limb ischemia are at risk for major amputations- both above the knee and below the knee. The treatment options currently consist of either revascularization procedures by classical surgery bypass or endovascular treatment with the end-goal of improving amputation-free survival rates. A multidisciplinary team is required in critical limb ischemia to analyze the available options regarding revascularization therapy. This team, comprising of cardiovascular surgeon, vascular technologist, cardiovascular anesthesiologist, plastic surgeon and interventional cardiologist/radiologist should discuss revascularization indication for each patient, taking into consideration the overall condition, wound status and target vessels lesions characteristics28. The team must also consider the appropriate time for amputations, being them major – above or
below the knee or minor. It is estimated that the amputation- free survival rate in a multidisciplinary cohort is 64%, as compared to 67% in the general population29. More than 50% of the peripheral artery disease cases are accompanied by coronary artery disease28. Therefore, another different concept in peripheral arterial disease is multidisciplinary chronic care team (not a multidisciplinary team created to analyze only the available options regarding revascularization therapy). This one, is comprising of a cardiologist, diabetologist, nephrologist, neurologist, plastic or general surgeon, or any other specialist possible involved in chronic medical care of a patient with peripheral arterial disease; it must be capable of offering a better chronic medical care, to improve both the overall survival rate and amputation-free survival, while contributing to a better quality of life. Managing patients with chronic limb ischemia requires a holistic approach of
the disease.
Heart Team in congenital heart disease
Congenital heart disease often leads to development of pulmonary arterial hypertension (PAH). Of such, several anomalies have been noted: ventricular and atrial septal defects with a low to moderate risk of developing PAH; unrepaired truncus arteriousus with a high risk for PAH; patent ductus arteriousus30. It has been estimated that 10% of the adult population suffering from congenital heart disease develop pulmonary hypertension30. Eisenmenger syndrome refers to PAH (mean pulmonary arterial pressure of at least 25 mm Hg at rest or over 30 mm Hg during exercise), reversal of preexisting shunt and cyanosis due to untreated congenital heart defects consisting of intracardiac communication (atrial, ventricular septal defects or patent ductus arteriosus). Though most cases develop before puberty, Eisenmenger syndrome in young adults has been reported (delayed on-set in case of medium-sized atrial septal defect)31. The need for a multidisciplinary approach to PAH is explained by the difficulty in prompt diagnosis, management and improvement of patient’s quality of life. PAH management is, in itself, a challenge for physicians, patients and caregivers all together. Guidelines recommend referral to specialized centers in case of intermediate to high risk patients (Reveal score ≥8)32. The first difficulty lies in the diagnosis itself. Manifesting at fi rst through unspecific symptoms such as exertion dyspnea, chest discomfort, and fatigue, this is a misleading diagnosis. It has been estimated that 33% of PAH patients were misdiagnosed at first and 57% have underwent inappropriate treatment32. Primary care physicians should be involved as to shorten the diagnosis interval and to better follow patients throughout the evolution of the disease. PAH is frequently misdiagnosed as asthma or other respiratory affections due to the initial manifestations of the disease31. A pulmonologist is required to accurately interpret pulmonary function and cardiopulmonary exercise tests, as well as blood gas results. The need for a cardiologist and cardiothoracic surgeon is obvious. It is through echocardiogram that the right ventricle failure is shown as an indirect sign of pulmonary hypertension. Also, the gold standard in certifying the elevated pulmonary pressure is right heart catheterization, which can only be performed in specialized centers. Performing an electrocardiogram brings additional information such as right axis deviation, right atrial enlargement and right ventricle hypertrophy31. Performing transthoracic/transesophageal echocardiography and electrocardiogram represent a class 1 indication, level of evidence C according to ACC/AHA
2008 guidelines for the Management of Adults with Congenital Heart Disease31. Regarding treatment, when faced with unresponsiveness to maximal medical therapy, there are two options available: either atrial septostomy (as a palliative procedure or bridging therapy) or lung transplant. Both require outstanding surgeons and trained specialists in centers capable of providing appropriate postsurgical care. The pharmacological options for treating PAH have recently improved32, but some drugs determine notable side effects such as hypotension, headache, diarrhea,
vomiting and nausea, requiring careful administration and appropriate dose titration, their use being limited to experienced centers. Frequently, patients with PAH suffer from depression, anxiety and insomnia due to the social and emotional impact of PAH31. Limitations in performing daily activities and restricted exercise capacity have great impact on patients. A psychologist is required to manage these conditions, provide counseling and prescribe treatment, if necessary.
The need for a radiologist is motivated by the numerous imagistic procedures required to properly diagnose PAH – such as chest radiographs, computertomography, magnetic resonance imaging. Moreover, in order to differentiate PAH from chronic thromboembolic pulmonary hypertension, a lung ventilation-perfusion scan is necessary. Pulmonary arterial hypertension patients have numerous comorbidities ranging from their underlying heart disease to newly developed right-heart failure, rheumatologic diseases, connective tissue disorders, liver impairment and other respiratory pathologies. Thus, variable specialists are necessary for proper management in the context of an already deteriorating state. Since PAH has a chronic and progressive evolution often with devastating effects on the quality of life, patients would benefi t from a palliative care specialist. Overcoming the misconception of end-of-life care will bring comfort to both patients and caregivers. Both patients’ survival rate and quality of life are improved with a prompt diagnosis, appropriate treatment establishment and adherence. Also, the costs for caring for such patients are lowered through the reduction of hospitalizations. A team consisting of a primary care physician, cardiologist, cardiothoracic surgeon, pulmonologist, radiologist, psychiatrist/psychologist, palliative care specialist working on PAH patients provides the required multidisciplinary approach that optimizes patient- centered care30.
Atrial fibrillation Heart Team
An atrial fibrillation Heart Team apply to reversal to a rate control strategy in patients with severe atrial fi brillation symptoms (EHRA III or IV) or in patients with failed rhythm control therapy and they need of advanced and complex rhythm control interventions33. In these patients a decision involving atrial fi brillation surgery or extensive atrial fi brillation ablation should be based on advice from an atrial fi brillation Heart Team. This should consist of a cardiologist with expertise in antiarrhythmic drug therapy, an interventional electrophysiologist, and a cardiac surgeon with expertise in appropriate patient selection, techniques, and technologies for interventional or surgical AF ablation. Heart Team limitations It has been brought up that a Heart Team approach
could result in an unnecessary step in the clinical process, resulting in a delay in treatment. This could be time-consuming for the involved physicians, as well as inefficient and more expensive2. A solution could be that the Heart Team only takes into consideration the patients in whom a discussion on treatment strategies is relevant. This implies that decisions on treatment can be made without a formal Heart Team meeting, for which cardiac surgeons and (interventional) cardiologists can use guidelines to formulate a local protocol2. For instance, according to the 2010 European Society of Cardiology/European Association for Cardio-Thoracic Surgery revascularization guidelines7, patients with single vessel coronary artery disease may undergo ad hoc stenting to avoid two separate catheterizations2. In this setting, an ad hoc Heart Team should be set up to allow surgical consultation in the catheterization laboratory2. In this way a delay is avoided; in ct, acceleration in the process of therapy can be accomplished. Ethically and legally considerations Sometimes there is a fine borderline between risk and benefit for some therapeutic options. Therefore the decision in favor of one specific therapy should be taken after interdisciplinary discussions. In these situations, following a standard protocol, regardless of the more expensive cost, is proved to be safer for both the patient and physician as it determines an early diagnosis and offers a better prognostic by avoiding severe complications that come with unfavorable social implications and higher costs. If there was a protocol of standard controls to be performed in these situations, despite the initial high costs, practitioners would be safeguarded against the much debated state of medical negligence, the diagnosis would be determined earlier, preventing the appearance of more serious incapacitating complications which in return cause very high social costs. On account of this defi ciency, the practitioner and the medical facility which employed him are always exposed to this kind of dispute with significant bioethical outcomes. More than that, the development of risk scores based on clinical, biological and/or echocardiographic criteria might promptly identify patients with high risk of severe complications; the specific empirical therapy would be immediately started, complications would diminish and the prognosis for this serious disease would be improved. This fact has become a reality, nowadays which makes physician-patient and illness-heath relationship more complex and vulnerable10. As physicians, it is natural to ask for and accept a second opinion for the patients’ safety. In Romania, the right for second opinion seems to be unknown by one third of physicians1; this right is unknown by the patients too. This is because illness and health are perceived not as states of being alive but as ways of being
alive5. An important role and frequently with a strong negative impact in Romania (as in all Eastern Europe countries) is played by the media, both in social and especially in medical environment3. Civil assurances fail to better protect the physicians if they do not follow the law1. The absence of a specialist with specific competence and⁄or the difficult interdisciplinary collaboration exposes the physicians that took care of patients to malpractice risk. These problems yet unresolved by the authorities continue to expose the Romanian physicians to malpractice risk. Evidence based medicine and the use of guidelines in daily practice lowers the amount of physician’s responsibilities and offers a protection in front of litigious and malpractice5. However, this could put the patient in situations in which professional responsibilities are not well delimited and imprecisely assumed. The ethically and legally aspects underlining this paper could be
a possible alarm for the vulnerable specialties that are implicated in diagnosing and treating the patients with complex and severe cardiac disease.
Before conclusions…
Similarly to the various stages of the cardiovascular disease continuum there is mandatory to have a continuum of medical care of patients with cardiovascular disease in order to slow or stop their evolution. For example, any of the above described pathologies must follow a cardiac rehabilitation therapy, a mandatory step in the continuum of medical care of patients with cardiovascular disease. Cardiac rehabilitation team may include a physician, exercise physiologist, specialist nurse, occupational therapist, physical educator, dietitian, psychiatrist or psychologist, physiotherapist and social worker. Another example is atrial fibrillation. A multidisciplinary atrial fibrillation team approach including physicians like general physicians, cardiology and stroke AF
specialists and surgeons, and allied health professionals work is recommended for an integrated management of atrial fibrillation care.
CONCLUSIONS
The new concept of Heart Team introduced in the recently published guidelines in cardiology, a multidisciplinary team of experts created in tertiary hospitals to fi nd the best medical care for a patient, might/should be set and work nationwide, including in our hospitals. Delayed diagnosis and appropriate treatment in the absence of a heart team might have medical, social, legal
and ethical outcomes. Heart Team is very important in tertiary hospitals involved in complex cardiovascular care for early diagnosis and appropriate treatment, to prevent or reduce long hospitalization, temporary or permanent incapacitation and implicitly social costs, and also as potential tool to avoid malpractice. However, this new concept in cardiovascular disease must be
differentiated by multidisciplinary chronic care team, another important step in the continuum of the medical care of patients with cardiovascular disease.
Conflict of interest: none declared.
Funding: none.
References
1. Holmes Jr DR, Mohr F, Hamm CW, Mack MJ. Venn diagrams in cardiovascular disease: the Heart Team concept. Eur Heart J 2014; 35: 66–68.
2. Head SJ, Kaul S, Mack MJ, Serruys PW, Taggart DP, Holmes DR Jr, Leon MB, Marco J, Bogers AJ, Kappetein AP. The rationale for the Heart Team decision-making for patients with stable complex coronary artery disease. Eur Heart J 2013;34:2510–2518.
3. Kolh P, Wijns W, Danchin N, Di Mario C, Falk V, Folliguet T, Garg S, Huber K, James S, Knuuti J, Lopez-Sendon J, Marco J, Menicanti L, Ostojic M, Piepoli MF, Pirlet C, Pomar JL, Reifart N, Ribichini FL, Schalij MJ, Sergeant P, Serruys PW, Silber S, Sousa Uva M, Taggart D. Guidelines on myocardial revascularization. Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS); European Association for Percutaneous Cardiovascular Interventions (EAPCI), Eur J Cardiothorac Surg 2010;38 Suppl:S1-S52.
4. Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, Falk V, Filippatos G, Hamm C, Head SJ, Jüni P, Kappetein AP, Kastrati A, Knuuti J, Landmesser U, Laufer G, Neumann FJ, Richter DJ, Schauerte P, Sousa Uva M, Stefanini GG, Taggart DP, Torracca L, Valgimigli M, Wijns W, Witkowski A. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 2014;35(37):2541-619.
5. Head SJ, Kaul S, Mack MJ, Serruys PW, Taggart DP, Holmes Jr DR, Leon MB, Marco J, Bogers AJJC, Kappetein AP. The rationale for Heart Team decision-making for patients with stable, complex coronary artery disease. Eur Heart J 2013; 34: 2510–2518.
6. Yates MT, Soppa GK, Valencia O, Jones S, Firoozi S, Jahangiri M. Impact of European Society of Cardiology and European Association for Cardiothoracic Surgery Guidelines on Myocardial Revascularization on the activity of percutaneous coronary intervention and coronary artery bypass graft surgery for stable coronary artery disease. J Thorac Cardiovasc Surg 2014;147:606-10.
7. Iyer S, Bauer T, Yeung M, Ramm C, Kiser AC, Caranasos TG, Vavalle JP. A heart team and multi-modality imaging approach to percutaneous closure of a post-myocardial infarction ventricular septal defect. Cardiovasc Diagn Ther 2016; 6:180-184.
8. Dawsona AG, Williamsb SG, Colec D. Does the placement of an Amplatzer septal occluder device confer benefi t in patients with a postinfarction ventricular septal defect? Interactive CardioVascular and Thoracic Surgery 2014; 19:1040–1047.
9. Bonzel T, Schachinger V, Dorge H. Description of a Heart Team approach to coronary revascularization and its benefi cial long-term effect on clinical events after PCI. Clin Res Cardiol 2016; 105:388–400.
10. Bonow RO, Maurer G, Lee KL, Holly TA, Binkley PF, Desvigne-Nickens P, Drozdz J, Farsky PS, Feldman AM, Doenst T, Michler RE, Berman DS, Nicolau JC, Pellikka PA, Wrobel K, Alotti N, Asch FM, Favaloro LE, She L, Velazquez EJ, Jones RH, Panza JA; STICH Trial Investigators. Myocardial viability and survival in ischemic left ventricular dysfunction. N Engl J Med 2011;364:1617–25.
11. Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL.2013ACCF/AHAguideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 2013;128(16): e240–327.
12. Sandoval Y, Brilakis ES, Canoniero M, Yannopoulos D, Garcia S. Complete Versus Incomplete Coronary Revascularization of Patients With Multivessel Coronary Artery Disease. Curr Treat Options Cardio Med 2015; 17: 8.
13. Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP III, Guyton RA, O’Gara PT, Ruiz CE, Skubas NJ, Sorajja P, Sundt TM III, Thomas JD. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;63:2438–2488.
14. Vahanian A, Alfi eri O, Andreotti F, Antunes MJ, Barón-Esquivias G, Baumgartner H, Borger MA, Carrel TP, De Bonis M, Evangelista A, Falk V, Lung B, Lancellotti P, Pierard L, Price S, Schäfers HJ, Schuler G, Stepinska J, Swedberg K, Takkenberg J, Von Oppell UO, Windecker S, Zamorano JL, Zembala M; ESC Committee for Practice Guidelines (CPG); Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC); European Association for Cardio-Thoracic Surgery (EACTS). Guidelines on the management of valvular heart disease (version 2012): the Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic
Surgery (EACTS). Eur J Cardiothorac Surg 2012;42(4):S1-44.
15. Holmes DR Jr, Mack MJ, Kaul S, Agnihotri A, Alexander KP, Bailey SR, Calhoon JH, Carabello BA, Desai MY, Edwards FH, Francis GS, Gardner TJ, Kappetein AP, Linderbaum JA, Mukherjee C, Mukherjee D, Otto CM, Ruiz CE, Sacco RL, Smith D, Thomas JD; American College of Cardiology Foundation, American Association for Thoracic Surgery, Society for Cardiovascular Angiography and Interventions, Society for Thoracic Surgeons, American Heart Association, American Society of Echocardiography, European Association for Cardio- Thoracic Surgery, Heart Failure Society of America; Mended Hearts, Society of Cardiovascular Anesthesiologists, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance.
2012 ACCF/AATS/SCAI/STS expert consensus document on transcatheter aortic valve replacement. Ann Thorac Surg 2012; 93:1340–95.
16. Castrodeza J, Amat-Santos IJ1, Blanco M, Cortes C, Tobar J, Martin- Morquecho I, López J, Di Stefano S, Rojas P, Varela-Falcon LH, Gomez I, San Roman JA. Propensity score matched comparison of transcatheter aortic valve implantation versus conventional surgery in intermediate and low risk aortic stenosis patients: A hint of real-world. Cardiol J 2016 Jul 21. doi: 10.5603/CJ.a2016.0051. [Epub ahead of print]).
17. Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta JP, Del Zotti F, Dulgheru R, El Khoury G, Erba PA, Iung B, Miro JM, Mulder BJ, Plonska-Gosciniak E, Price S, Roos-Hesselink J, Snygg-Martin U, Thuny F, Tornos Mas P, Vilacosta I, Zamorano JL. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC) Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J 2015;36:3075-128.
18. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P; Authors/Task Force Members.2016 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure. Eur Heart J 2016;37(27):
2129-200.
19. Grady KL, Dracup K, Kennedy G, Moser DK, Piano M, Stevenson LW, Young JB. Team management of patients with heart failure: A statement for healthcare professionals from The Cardiovascular Nursing Council of the American Heart Association. Circulation 2000; 102(19):2443-56.
20. Jaarsma T. Inter-professional Team Approach to Patients with Heart Failure. Heart 2005: ;91(6):832-8.
21. Larsen PM, Teerlink JR. Team-based Care for Patients Hospitalized with Heart Failure. Heart Fail Clin 2015;11(3):359-70.
22. Mebazaa A, Yilmaz MB, Levy P, Ponikowski P, Peacock WF, Laribi S, Ristic AD, Lambrinou E, Masip J, Riley JP, McDonagh T, Mueller C, DeFilippi C, Harjola V-P, Thiele H, Piepoli MF, Metra M, Maggioni A, McMurray J, Dickstein K, Damman K, Seferovic PM, Ruschitzka F, Leite- Moreira AF, Bellou A, Anker SD, Filippatos G. Recommendations on pre-hospital and early hospital management of acute heart failure: a consensus paper from the HFA of the ESC, the European Society of Emergency Medicine and the Society of Academic Emergency Medicine. Eur J Heart Fail 2015;17:544–558.
23. Mueller C, Christ M, Cowie M, Cullen L, Maisel AS, Masip J, Miro O, McMurray J, Peacock FW, Price S, DiSomma S, Bueno H, Zeymer U, Mebazaa A. European Society of Cardiology-Acute Cardiovascular Care Association position paper on acute heart failure: a call for interdisciplinary care. Eur Heart J Acute Cardiovasc Care 2015 Jun 29. pii: 2048872615593279.
24. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P; Authors/ Task Force Members. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016;37(27):2129-200. doi: 10.1093/eurheartj/ehw128.
25. Daubert C, Behar N, Martins RP, Mabo P, Leclercq C. Avoiding nonresponders to cardiac resynchronization therapy: a practical guide. European Heart Journal 2016 doi:10.1093/eurheartj/ehw270
26. Suzuki H, Maeda A, Maezawa H, Togo MT, Nemoto H, Kasai Y, Ito Y, Nakada T, Sueki H, Mizukami A, Takayasu M, Iwaku K, Takeuchi S, Tanaka H, Iso Y The Effi cacy of a Multidisciplinary Team Approach in Critical Limb Ischemia. Heart Vessels 2016 Apr 22. [Epub ahead of print].
27. Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG; TASC II Working Group, Bell K, Caporusso J, Durand-Zaleski I, Komori K, Lammer J, Liapis C, Novo S, Razavi M, Robbs J, Schaper N, Shigematsu H, Sapoval M, White C, White J, Clement D, Creager M, Jaff M, Mohler E 3rd, Rutherford RB, Sheehan P, Sillesen H, Rosenfi eld K. Inter-society consensus for the management of peripheral arterial disease (TASC II). Eur J Vasc Endovasc Surg 2007;33 Suppl 1:S1-75.
28. Hioki H, Miyashita Y, Miura T, Ebisawa S, Motoki H, Izawa A, Tomita T, Koyama J, Ikeda U. Prognostic Improvement by Multidisciplinary Therapy in Patients With Critical Limb Ischemia. Angiology 2015: 66(2): 187-94.
29. Chung J, Modrall G, Ahn C, Lavery LA, Valentine RJ. Multidisciplinary care improves amputation-free survival in patients with chronic critical limb ischemia. J Vasc Surg 2015; 61:162–169.
30. Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA, del Nido P, Fasules JW, Graham TP Jr, Hijazi ZM, Hunt SA, King ME, Landzberg MJ, Miner PD, Radford MJ, Walsh EP, Webb GD, Smith SC Jr, Jacobs AK, Adams CD, Anderson JL, Antman EM, Buller CE, Creager MA, Ettinger SM, Halperin JL, Hunt SA, Krumholz HM, Kushner FG, Lytle BW, Nishimura RA, Page RL, Riegel B, Tarkington LG, Yancy CW; American College of Cardiology; American Heart Association Task Force on Practice Guidelines (Writing Committee
to Develop Guidelines on the Management of Adults With Congenital Heart Disease); American Society of Echocardiography; Heart Rhythm Society; International Society for Adult Congenital Heart Disease; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons. ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Develop Guidelines on the Management of Adults With Congenital Heart Disease). Developed in Collaboration With the American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol 2008;52(23):e143-263.
31. Benza RL, Miller DP, Foreman AJ, Frost AE, Badesch DB, Benton WW, Mc Goon MD. Prognostic implications of serial risk score assessments in patients with pulmonary arterial hypertension: a Registry to Evaluate Early and Long Term Pulmonary Arterial Hypertension Disease Management (REVEAL) analysis. J Heart Lung Transplant 2015; 34:356361.
32. Taichman DB, Ornelas J, Chung L, Klinger JR, Lewis S, Mandel J, Palevsky HI, Rich S, Sood N, Rosenzweig EB, Trow TK, Yung R, Elliott CG, Badesch DB. Pharmacologic therapy for pulmonary arterial hypertension in adults: CHEST guideline and expert panel report. Chest 2014;146:449475.
33. 2016 ESC Guidelines for the management of atrial fi brillation developed in collaboration with EACTS The Task Force for the management of atrial fibrillation of the European Society of Cardiology (ESC). Eur Heart J 2016; 37: 2893–2962.
 This work is licensed under a
This work is licensed under a