Lucian M. Predescu1,2, Marin Postu1, Lucian Zarma1, Adrian C. Bucsa1, Pavel Platon1,2, Marian Croitoru1, Adrian Mereuta1,2, Dan M. Dorobantu3, Leonard A. Lichiardopol4, Alexandra G. Predescu5, Carmen Ginghina1,2, Dan E. Deleanu1
1 „Prof. Dr. C. C. Iliescu” Emergency Institute for Cadiovascular Diseases, Bucharest, Romania
2 „Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
3 University of Bristol, Bristol, United Kingdom
4 Tulcea County Hospital, Tulcea, Romania
5 Colentina Clinical Hospital, Bucharest, Romania
Abstract: Background – Coronary artery bypass surgery (CABG) has been considered the gold standard for the treat-ment of left main coronary artery disease, for many years. However, the development from last years in stent technology and the use of intravascular imaging to assess the results after percutaneous coronary interventions (PCIs) have rapidly increased the number of patients with unprotected left main coronary artery disease (ULMCAD) treated by PCI. The aim of the current study was to report the current practice of ULMCAD PCI in a Romanian high-volume PCI center and compare the results with those reported by other studies. Methods and Results – A total of 146 patients with ULMCAD treated by PCI were included, 52% presenting with acute coronary syndrome (ACS). Outcomes at 4 years were estimated using the Kaplan Meier methsod. Baseline SYNTAX II score for PCI was intermediate, at a median of 28.9. The early mortality rate was 8.2% with a 2% peri-procedural mortality. 4-year mortality, target lesion revascularization (TLR) and major adverse cardiac events (MACE) were 21.9%, 14% and 32.5%, respectively. The rates of in-stent thrombosis and in-stent restenosis at 4 -year follow up were 2.74% and 11.1%, respectively. Conclusions – The early mortality rate in our study, which included an important number of patients presenting with ACS, was not signifi cantly higher than in other studies with fewer ACS pa-tients. The main difference with other studies was the higher in-stent thrombosis and in-stent restenosis rate. However, the rate of TLR and mortality at 4-year follow up was not significantly different than those previously reported by other studies. Keywords: percutaneous coronary intervention; left main coronary artery disease.
INTRODUCTION
Coronary artery bypass surgery (CABG) has been considered the best treatment option for left main coronary artery disease for a long time. However, the recent developments from past years in stent te-chnology and the utilization of intravascular imaging to assess the results after percutaneous coronary in-terventions (PCIs) have led to a rapid increase in the number of patients with unprotected left main coro-nary artery disease (ULMCAD) treated by PCI1. Many studies have excluded patients with acute coronary syndrome (ACS)2,3. Therefore, there is a significant gap in knowledge regarding the treatment of patients with ULMCAD in a mixed, acute and elective patients. The aim of our study was to defi ne the current prac-tice of ULMCAD PCI in a Romanian high-volume PCI center and compare its outcomes with those reported by other studies, including the patients presented with ACS.
METHODS
Study Population
All patients with ULMCAD treated by PCI between January 2014 and December 2018 were reviewed from the electronic hospital records at the “Prof. Dr.
- Iliescu” Institute for Cardiovascular Diseases, Bucharest, Romania. Patients with a history of CABG and occluded grafts and patients presenting with ACS were included, also. Only patients with ULMCAD and complete data (discharge letter, angiography and an-gioplasty operation notes) were included. This resul-ted in a total of 146 patients for which demographic, clinical, angiographic, procedural, post-procedural and outcome data were extracted from the hospital elec-tronic records. All patients were followed by in-hospi-tal reevaluation. Data analysis was performed with the approval of the institutional ethics committees of the hospital involved.
Study Outcomes
MACEs were defined as the occurrence of death, myocardial infarction (MI) or target lesion revascula-rizations (TLRs). ACS was defined as either unstable angina, non-ST segment elevation MI (NSTEMI) or ST segment elevation MI (STEMI). The diagnosis of peri-procedural MI was made when after PCI there was an increase in CK-MB or troponin levels that was 5 times the upper normal level. TLR was defined as repeated PCI for restenosis of the entire segment involving the implanted stent. Stent thrombosis was defined as acute (0-24 hours), subacute (1–30 days), late (31–360 days), or very late (>360 days)4. Angiographic success was defined as residual stenosis of <30% by visual es-timation in the presence of Thrombosis in Myocardial Infarction (TIMI) fl ow grade 3. Complete revasculari-zation was defined as any attempt to revascularize all diseased segments (≥2.5 mm in diameter).
Statistical Analysis
Frequencies are given as numbers and percentages, continuous values as median (inter-quartile range or minimum-maximum values). Early outcomes (morta-lity, stent thrombosis, need for intra-aortic balloon pump (IABP), access site complications) are based on known status at 30 days and presented as percentage. Late outcomes are estimated using the Kaplan Meyer method. Late outcomes of interest were mortality, TLR and MACE. Statistical analyses were done with STATA/SE 12.0 (StataCorp LP, College Station, TX).
RESULTS
A total of 146 patients undergoing unprotected left main PCI were included, age ranging from 33 to 86 years (mean of 62 years). Detailed demographic and baseline clinical characteristics and laboratory tests are presented in Table 1 and 2. The most prevalent cardiovascular risk factors were dyslipidemia (87%) and hypertension (84%). 40% of patients with ULM-CAD had a history of ACS and 23% of previous non-left main PCI. The most frequent comorbidity was the chronic kidney disease, which was present in 77% of patients.
52% of patients with ULMCAD presented with ACS, 12.33% with STEMI and 8.2% with ACS com-plicated with cardiogenic shock (Figure 1). The asso-ciation of coronary artery disease with heart failure was common (77% of patients). Most patients were on antianginal treatment (90.2%) at admission.
56% of patients had an abnormal electrocardiogram tracing at presentation. The mean left ventricular ejec-tion fraction at diagnosis was 46%.
Angiographic characteristics
The mean Syntax Score was 21. The mean Syntax Sco-re II for PCI and CABG were 28.9 and 31.5. The cor-responding 4-year mortality estimate were 8.3% for PCI and 6.2% for CABG. The mean EuroSCORE II was 1.1%.
Table 3 shows the main angiographic findings of pati-ents with ULMCAD. Coronary angiogram was done in more than two third of patients by femoral approach.
76.7% of lesions involved the distal segment of left main (Figure 2). The left main lesions were associated with triple vessel disease in 9.59% of patients and a chronic total occlusion was present in 21% of patients. Approximately, one third of patients had complex left main lesions, calcified, ulcerated and diffuse lesions. According to Medina classification, the most prevalent lesions involved the ostium of left anterior descending artery (LAD) (27.4%) and the distal left main bifurcati-on (Medina 1/1/1 lesion) (25.2%).
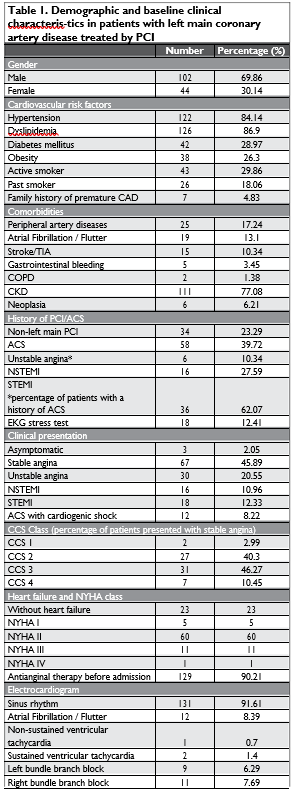
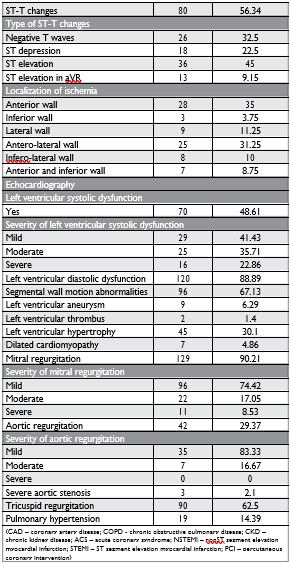
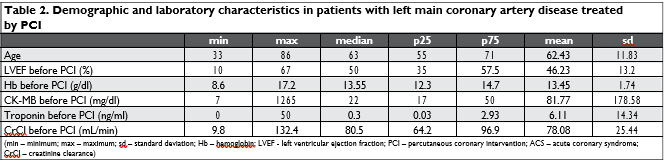
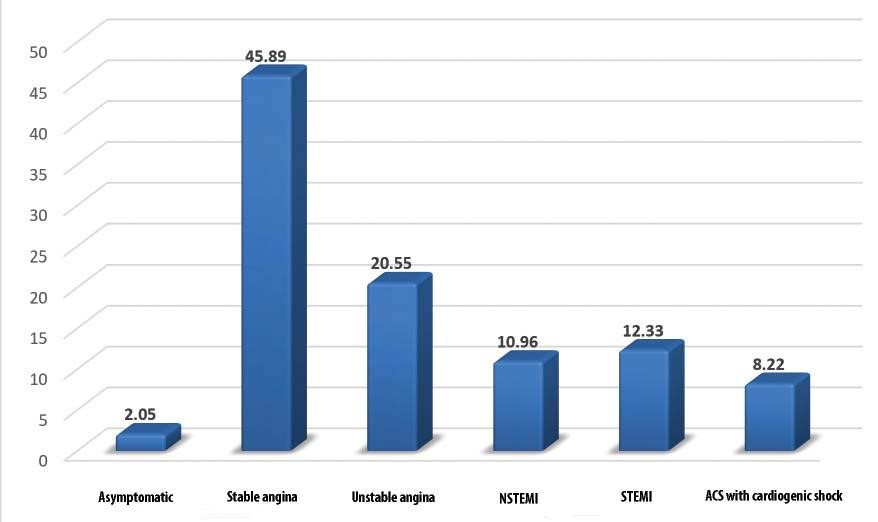
Figure 1. Clinical presentation of patients with unprotected left main coronary artery disease (percentage) (NSTEMI – nonST segment elevation myocar-dial infarction; STEMI – ST segment elevation myocardial infarction; ACS – acute coronary syndrome).
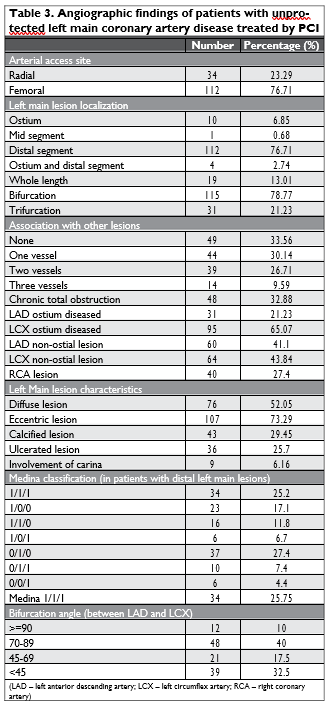
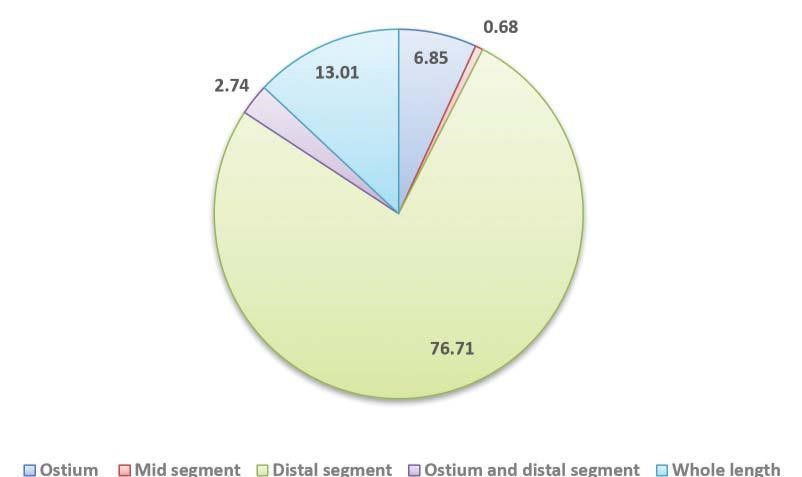
Figure 2. Localization of left main lesion (percentage).
Procedural characteristics
In 59 cases (40.4%) the PCI procedure was performed during the same session as the diagnostic coronary an bigger than the mean reference LAD diameter before PCI (Figure 3).
Early outcomes
Peri- and post-procedural complications are summa-rized in Table 5. The most common peri-procedural complications were: bradyarrhythmia (6.85%), peri-procedural myocardial infarction (2.74%) and ven-tricular tachycardia or fi brillation (2.74%). Vascular puncture site complications were present in 4.1% of cases, in the context of a high proportion of patients treated by a femoral approach.
There was an 8.2% early mortality (30 days morta-lity) (n=12), with a 2% peri-procedural mortality (n=3) (Table 6). Most deaths occurred in patients presenting with ACS (n=11) and mostly in patients complicated with cardiogenic shock (n=8). As such, early mortality in non-ACS patients was 1.4% with no peri-procedural deaths and early mortality in ACS patients was 14.47% with 3.95% peri-procedural mortality.
Three patients underwent an emergency angiogra-phic reevaluation during the same hospitalization. In two cases an acute in stent thrombosis was found, while in the third case an acute LCX thrombosis was found, with permeable left main stent. All three pati-ents had presented initially with MI and died during the same hospitalization.
Post-procedural IABP was used in 8 cases (n=5.5%), only in ACS patients, with 4 of them having IABP support prior to the PCI procedure. We found that in patients with cardiogenic shock at presentation pre-procedural IABP was not associated with decreased early mortality (60% vs 71%, p=0.6), but use of IABP for post-procedural support was associated with a de-crease in early mortality (20% vs 100%, p=0.01).
Late outcomes
59% of patients had no angina after ULMCAD PCI on long-term follow up. In 29.8% of patients the coronary angiogram was repeated, routinely only in 11.2% of patients. The in-stent restenosis rate was 11.1% and the in-stent thrombosis rate was 2.74%. Only 0.68% of patient had a late in-stent thrombosis (Table 6).
The mortality, TLR and MACE rates at 1 years were 16.5%, 10.9%, 27.2% and at 4 years 21.9%, 14% and 32.5% overall (Figure 4). In non-ACS patients, the mortality, TLR and MACE rates at 4 years were 9.6%, 15% and 24.1% compared to 33.3%, 12.8% and 40.1% in ACS-patients.
DISCUSSIONS
Our study included an unselected population with ULMCAD PCI without considering the clinical presen-tation. Patients presenting with ACS and ULMCAD were not excluded. The aim of this study was to show the result of real-life practice of ULMCAD PCI in a Romanian high-volume PCI-center with experience in treating elective and urgent patients with complex LM lesions. The study included 146 patients with ULM-CAD PCI of which 52% presented with ACS.
Although, mean Syntax score, that depends on the anatomical complexity of left main lesions, was 21, the study population included high risk patients conside-ring that 8.2% of cases presented with ACS complica-ted with cardiogenic shock. Many patients (39.7%) had a history of ACS, also. The study population wasn’t an elderly population considering the mean age was 62 years. The most prevalent comorbidity was chronic kidney disease (77%) followed by peripheral artery di-sease (17%).
Only half of patients had an abnormal EKG tracing. Although, even if we are referring to patients with ULMCAD, only 9% of cases had ST segment elevation in aVR lead. 48% of patients had an abnormal LVEF, but the mean LVEF of study population was 46%.
Although, a lot of studies recommended the use of radial approach, especially in STEMI patients, both co-ronary angiogram and PCI were done using femoral approach (76% for coronary angiogram and 89% for PCI)5,6.
Only 4.1% of patients received an IABP (the only available hemodynamic support system in our institu-tion at that time), although 8.2% of patients were in cardiogenic shock at presentation. The use of IABP after the procedure was associated with a decrease in early mortality, but this result must be interpreted with caution due to the low number of patients.
One third of patients had complex left main lesions (calcified, ulcerated, diffuse lesions), 25% had a Medina 1/1/1 lesion, 21% had a chronic total occlusion and only 11 patients had an ostial or mid segment left main lesion. Given the complexity of left main lesions, only 58.9% of patients were treated with a one-stent stra-tegy. The most common two-stent strategies were TAP (35.1%), mini-crush (31.6%) and culotte (22.8%). The use of two-stent strategy for ULMCAD PCI was signifyingly higher than in other studies7.
The use of POT and KBPD was low when compa-red to other studies7,8. This can be explained by the high number of STEMI patients were the “keep it sim-ple” principle is highly recommended. Another reason is the high number of patients treated with a self-appo-sing stent (42%). Although there is no clear recom-mendation, with self-apposing stents there is no need to perform routinely POT and KBPD, considering that the stents have the property to continue their expan-sion and appose to the vessel wall.
The use of intracoronary imaging was low (17.8%) considering that around 40% of patients were treated with a two-stent strategy. This can also be explained by the high number of patients with ACS, also.
The procedural success rate was 94.5% and comple-te revascularization was achieved in 74.6% of patients.
Although, our study has included the patients pre-sented with ACS, the early mortality was similar to the EXCEL (Evaluation of XIENCE Versus Coronary Ar-tery Bypass Surgery for Effectiveness of Left Main Revas-cularization) trial (8.2% in our study vs 8.1% in EXCEL trial)9,10. The early mortality in our study is slightly hi-gher when we compare with a recent american regis-try (8.2% vs 5%)11.
The 4-year mortality rate and TLR were signifi-cantly higher than those in the NOBLE (Nordic-Baltic-British left main revascularization) trial at 5 year follow up (mortality and TLR rate in our study were 21.9% and 14%, respectively versus 12% and 16% in NOBLE trial) 12. When we excluded the patient presented with ACS, the long-term mortality and TLR rates were comparable in the two studies (mortality and TLR rate in our study were 9.6% and 15%, respectively versus 12% and 16% in NOBLE trial)12. In EXCEL trial the 3-year TLR and mortality rates were 9.5% and 8.2%, respectively9,10.
The rates of in-stent thrombosis and in-stent re-stenosis were 0.7% and 7.4%, respectively, in a recent American registry and 2.74% and 11.1% in our study11.
In the EXCEL trial the in-stent thrombosis was 1.3%9,10.
The 4-year mortality after PCI estimated by the SYNTAX score II was 8.3% that is similar with the 4-year mortality of 9.64% from our study.
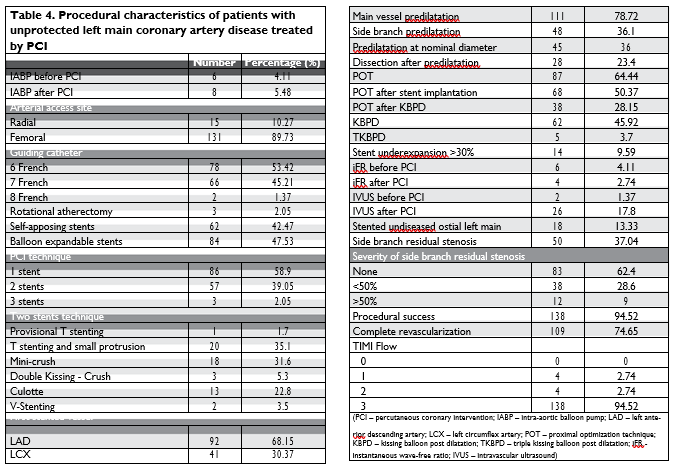
Figure 3. Mean left main, LAD and LCX diameters before and after PCI – mm (LAD – left anterior descending artery; LCX – left circumflex artery; PCI – percutaneous coronary intervention).
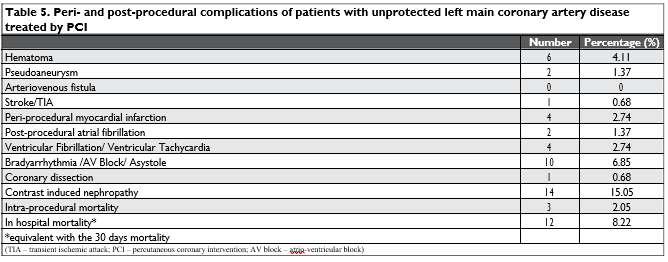
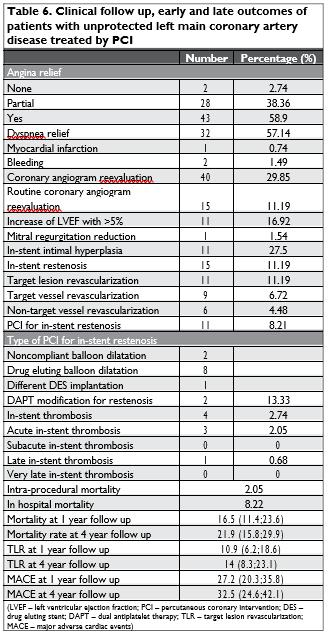
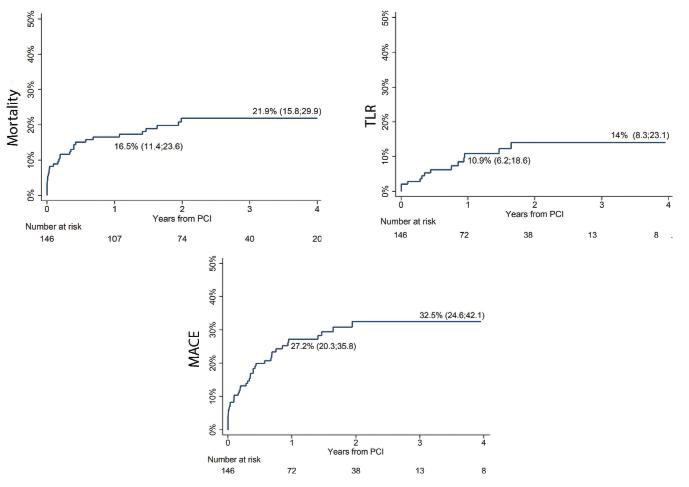
Figure 4. Mortality, TLR and MACE rates at 4-year of patients with unprotected left main coronary artery disease treated by PCI – Curves represent Kaplan-Meier failure function (TLR – target lesion revascularization; MACE – major adverse cardiac events; PCI – percutaneous coronary intervention).
STUDY LIMITATIONS
Although it might have offered more data on resteno-sis, routine angiographic reevaluation is no longer re-commended and was not performed. The small number of early events prevented multivariable analyses, so the results are subject to confounding. The use of various types of stents introduces a degree of hetero-geneity.
CONCLUSIONS
Although, our study included patients presented with ACS, the early mortality rate was not significantly higher than in other studies, that included less ACS patients. The main difference with other studies was the higher in-stent thrombosis and in-stent restenosis rate. However, the rates of TLR and death weren’t significantly different of other studies.
Conflict of interest: none declared.
References
1. Predescu L.M, Zarma L, Platon P, et al, Current treatment of left main coronary artery disease, Cor et Vasa 58 (2016), pp. e328-e339, DOI information: 10.1016/j.crvasa.2015.05.007.
2. Park SJ, Ahn JM, Kim YH, Park DW, Yun SC, Yoon SH, et al. Tem-poral trends in revascularization strategy and outcomes in left main coronary artery stenosis: data from the ASAN Medical Center-Left MAIN Revascularization registry. Circulation Cardiovascular inter-ventions. 2015;8(3):e001846.
3. Lassen JF, Burzotta F, Banning AP, Lefevre T, Darremont O, Hildick-Smith D, et al. Percutaneous coronary intervention for the left main stem and other bifurcation lesions: 12th consensus document from the European Bifurcation Club. EuroIntervention : journal of EuroP-CR in collaboration with the Working Group on Interventional Car-diology of the European Society of Cardiology. 2018;13(13):1540-53.
4. Cutlip DE et al, Academic research consortium. Clinical end points in coronary stent trials: A case for standardized definitions. Circula-tion 2007;115:2344–2351.
5. Bernat I, Horak D, Stasek J, Mates M, Pesek J, Ostadal P, et al. ST-segment elevation myocardial infarction treated by radial or fem-oral approach in a multicenter randomized clinical trial: the STE-MI-RADIAL trial. Journal of the American College of Cardiology. 2014;63(10):964-72.
6. Mason PJ, Shah B, Tamis-Holland JE, Bittl JA, Cohen MG, Safirst-ein J, et al. An Update on Radial Artery Access and Best Practices for Transradial Coronary Angiography and Intervention in Acute Coronary Syndrome: A Scientific Statement From the Ameri-can Heart Association. Circulation Cardiovascular interventions. 2018;11(9):e000035.
7. Lee PH, Ahn JM, Chang M, Baek S, Yoon SH, Kang SJ, et al. Left Main Coronary Artery Disease: Secular Trends in Patient Characteristics, Treatments, and Outcomes. Journal of the American College of Car-diology. 2016;68(11):1233-46.
8. Fajadet JC, A. Current management of left main coronary artery dis-ease. European heart journal. 2012;33(1):36-50b.
9. Stone GW, Sabik JF, Serruys PW, Simonton CA, Genereux P, Pus-kas J, et al. Everolimus-Eluting Stents or Bypass Surgery for Left Main Coronary Artery Disease. The New England journal of medicine. 2016;375(23):2223-35.
10. Kandzari DE, Gershlick AH, Serruys PW, Leon MB, Morice MC, Simonton CA, et al. Outcomes Among Patients Undergoing Distal Left Main Percutaneous Coronary Intervention. Circulation Cardio-vascular interventions. 2018;11(10):e007007.
11. Valle JA et al., Contemporary Use and Trends in Unprotected Left Main Coronary Artery Percutaneous Coronary Intervention in the United States: An Analysis of the National Cardiovascular Data Reg-istry Research to Practice Initiative., JAMA Cardiol. 2019 Feb 1;4(2): 100-109.
12. Makikallio T, Holm NR, Lindsay M, Spence MS, Erglis A, Menown IB, et al. Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NO-BLE): a prospective, randomised, open-label, non-inferiority trial. Lancet. 2016;388(10061):2743-52.
 This work is licensed under a
This work is licensed under a