Dan-Andrei Radu1, Radu Vatasescu1
1 Clinic of Cardiology, Emergency Clinical Hospital, Bucharest, Romania
Abstract: The anatomy of the cardiac conduction system has been studied extensively in the past. Some of the most notable contributors were Jan Evangelista Purkinje, Walter Gaskell, Wilhelm His Jr., Sunao Tawara and Ludwig Aschoff, Arthur Keith and Martin Flack while many others remain unnamed. In a medical academic era dominated by the neurogenic vs. myogenic theory of cardiac impulse generation, one of Tawara’stask under Aschoff’s indication was to dissect and examine 150 myocarditic human hearts (thus, rheumatic myocarditic nodules – later called bodies of Aschoff and Tawara – were discovered). Personally, Tawara saw it as an opportunity to refi ne Wilhelm His’s former studies that proposed the existence of a unique, central, muscular atrioventricular (AV) bridge that somehow connected the atrium to the ventricular myocardium after extensively dividing (peculiarly, he did not pursue a functional analysis). Since in rheumatic myocarditis Tawara performed extensive ventricular dissections he retrogradely followed His’s bundle (HB) back to the inferior interatrial septum (IAS), thus describing the AV node. Antegradely, he described the progressive division of the bundle, while realizing that his observations were consistent with those of Purkinje’s 60 years prior discovery of a “network of gelatinous fibers”1,2.
Keywords: left bundle-branch block, cardiac conduction system
ANATOMY OF THE LBBB
After passing through the central fi brous body (CFB) of the heart the HB runs down through the membranous part of the interventricular septum (IVS), occasionally in a bit leftward fashion2. At the junction of the membranous and muscular parts of the IVS it divides into the right bundle (RB) and the left bundle (LB). We nowadays know that the LB divides as following3:
– a pre-divisional segment (also called the “deadend” tract, seen in fetal or infant hearts; it runs antero-superiorly and ends at the aortic root; sometimes it is described as arising from the HB itself2)
– an anterior fascicle (sprouts the Purkinje fibers of the antero-lateral aspect of the LV)
– a posterior fascicle (sprouts the Purkinje fibers of the postero-inferior aspect of the LV)
– a median fascicle (to the interventricular septum; also called the septal branch).
Many authors ignore the existence of the septal branch, while others consider it is rather present in a minority of cases3. However, according to Tawara himself the triple branching of the proximal part of the LB is rather typical1,2.
ELECTRICAL ACTIVATION
The first ventricular part of the normal heart to be activated is the left side of the IVS. This occurs particularly due to the short septal branch that quickly connects with working myocardium at the inferior border of the middle septum4. The right side of the septum also becomes activated only a few milliseconds later but at a very distal, apical point where the RB first connects with working myocardium. Therefore, the overall septal activation vector of the normal heart (responsible for the initial 10-20% of the QRS complex) points in a rightward, anterior and upward fashion. Thus, on the normal surface ECG we frequently observe sharp and small r waves in leads V1 and V2 (because of the rightward and anterior orientation) as well as sharp and shallow q waves in leads DI and aVL (because of the rightward and upward orientation). The aforementioned anatomical and electrocardiographic considerations have clearly been confirmed by classic endocardial catheter mapping of the normal LV. Not only did this prove that the earliest EGM of the normal LV can be collected on the inferior septum4 but with some authors it also concluded that a normal LV is most often characterized by three endocardial breakthrough sites5. While due to catheters’ inter-electrode distance some authors’ observations were only consistent with two of the breakthrough sites initially described by Durrer et al, using the CARTO® (Biosense, Inc.) electrical-anatomic mapping system Josephson et al agree on the frequent existence of another activation point.
CURRENT DEFINITION OF LBBB
The AHA/ACCF/HRS recommendations regarding the diagnostic of intraventricular conduction disturbances, specifi cally LBBB, include the following6:
– QRS duration greater than or equal to 120 ms in adults
– Absent q waves in leads I, V5, and V6, but in the lead aVL, a narrow q wave may be present in the absence of myocardial pathology.
– R peak time greater than 60 ms in leads V5 and V6 but normal in leads V1, V2, and V3, when small initial r waves can be discerned in the above leads.
Therefore with current defi nition of “complete” LBBB we admit that the normal left-sided activation vectors can exist; the term “complete LBBB” is only width-oriented.
Furthermore, it has been long observed that the response to cardiac resynchronization therapy (CRT) of patients who meet the current guideline criteria is very heterogenous, with slight to no improvement in almost a third of them. Tremendous efforts have been put into identifying the possible cause of this (with huge financial implications). Non-contact mapping studies as early as 2003-2004 observed that the patterns of LV depolarization in the presence of LBBB vary widely from one heart failure (HF) patient to another7-9. In one of these studies two more crucial observations were made: first, the septal branch of the LB was the least often compromised part. Second, in the case of so-called “complete” LBBB, the activation of the LV would occur in an apical part of the anterior wall (opposite to the breakthrough point of the RB at the RV apex) and not in a trans-septal manner as observed in dog models7,10. Since block in the LB can occur at different levels, the authors of a more recent non-contact mapping publication state that preserved left-sided septal activation in the presence of LBBB on the surface ECG suggests reserved septal branch conduction10. Analyzing pre-operative ECG traces of patients with current ESC guideline CRT-P/D implant indication from our center we observed that the surface r and q waves associated with left-sided septal activation almost always persisted in the presence of classic LBBB morphology14. Notably, this observation stays valid also when applying the Strauss criteria (which anticipated the 2016 HF guidelines minimum recommended LBBB width for CRT change) for defi ning LBBB in CRT candidates, specifi cally a QRS width of ≥140 msec in men and ≥130 msec in women, along with mid-QRS notching or slurring in ≥2 contiguous leads11. Intraprocedural evaluation of the activation sequence in these patients almost always indicated significantly shorter midseptal timings vs. apical timings14. As a consequencethere is consistent data suggesting that in patients with HF due to systolic LV dysfunction and so-called “complete” LBBB left-sided activation of the IVS through the septal branch of the LB is generally preserved. Conservation of intrinsic IVS activation during CRT delivery may increase the percentage of CRT responders as well as the magnitude of response13,15,16.
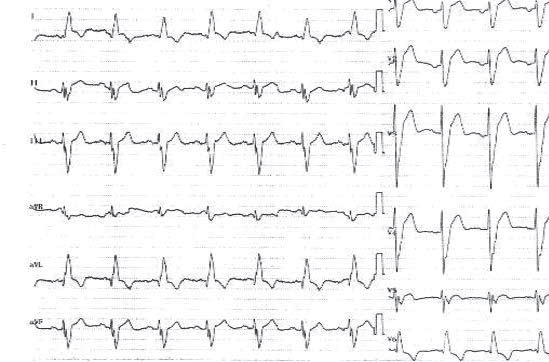
Figure 1. LBBB (~200 msec) with persistence of left-sided septal vectors (r-wave in V1, V2; q-wave in DI and aVL).
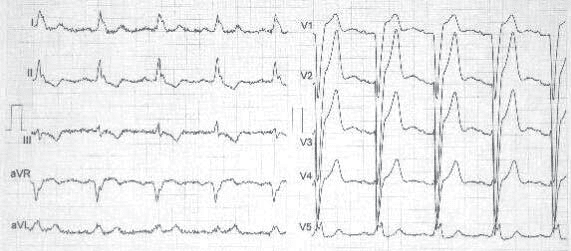
Figure 2. True complete LBBB; although only ~160 msec width, notice complete absence of r-wave in V1, V2 and q-wave in DI and aVL.
DISCUSSION
The pattern of RV delays along the course of the septum from the base to the apex cannot be explained by a purely right-sided depolarization through a patent RB. Aside from the fact that this would clearly not explain persistence of the r and q waves on the surface ECGs with LBBB, strong arguments against this have been around since Tawara himself described the conduction system. The AV node is the lowest part of the specialized cardiac conduction tissue that is not thoroughly insulated from adiacent cells, on the contrary it is coupled to the working myocardium of the atrium by intermediate transitional cells that create an electric “funnel”2. The HB however is closely surrounded by connective tissue from the CFB and therefore completely isolated; this is also true for its divisions, the RB and the LB and their main branches. The connective tissue is still present but progressively lost at the level of the His-Purkinje coupling sites which is far distal along the specialized conduction tissue2. Specifically, in the case of the RB this happens at the RV apex in the area of the fi rst RV endocardial breakthrough point, creating the leftward, minor, component of the septal depolarization, which has a minor delay by comparison with the rightward, major component in normal hearts). Thus, if it were for the depolarization pattern to be explained by the RB, less delay apically and more delay in the midseptal region (by retrograde, upward activation) would be systematically observed. Since most so-called “complete” LBBBs observed in CRT candidates have an early septal breakthrough point, it means that after implantation most resynchronized patients are triple-sites in fact, with varying degrees of fusion during BiV pacing (except for those with very short set AVs). Small series have demonstrated singnificantly improved responses to resynchronization with BiV pacing that favors fusion with the septalwavefront (probably due to shorter LV activation times)13, thus, recognizing preserved left-sided septal activation is defi nitely valuable. Data from 56CRT cases within our department clearly point to more electrical delay in the apical region than in the mid-septal region in the vast majority of presumed “complete” LBBBs according with the surface ECG characteristics (52 out of 56, p<0.0 01)14. Such data were also confi rmed bysinus rhythm LV endocardial activation mapping done with atraumatic remote magnetic navigation catheter in 10 patients with CHF due systolic LVD and LBBB (unpublished observations).
CONCLUSION
Current data strongly suggests that left-sided activation of the interventricular septum is preserved in the majority of patients of so-called “complete LBBBs”. From the electrical point of view it is improper to call a certain LBBB “complete” only because of its width. Morphological analysis of the presence/absence of the septal vectors is necessary to describe a truly complete block; at the same time presence of a preserved septal breakthrough should be accounted for when implanting a patient with a resynchronization device especially if CRT with fusion is pursued.
Conflicts of interest: none declared.
References
1. Silverman ME, Grove D, Upshaw CB Jr. Why does the heart beat?. Circulation 2006; 113:2775-2781.
2. Sánchez-Quintana D, Ho SY. Anatomy of Cardiac Nodes and Atrioventricular Specialized Conduction System. Rev EspCardiol 2003;56:1085-92
3. Sauer WH. Left bundle branch block. UpToDate Online
4. Josephson ME. Clinical Cardiac Electrophysiology: Techniques and Interpretations
5. Durrer D, van Dam RT, Freud GE, Janse MJ, Meijler FL, Arzbaecher RC. Total excitation of the isolated human heart. Circulation 1970; 41:899-912
6. Surawicz B, Childers R, Deal BJ, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part III: intraventricular conduction disturbances: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am CollCardiol 2009; 53:976.
7. Fung JWH, Yu CM, Yip G, Zhang Y, Chan H, Kum CC, Sanderson JE. Variable left ventricular activation pattern in patients with heart failure and left bundle branch block. Heart 2004 Jan; 90(1):17-19
8. Rodriguez LM, Timmermans C, Nabar A, Beatty G, Wellens HJ. Variable patterns of septal activation in patients with left bundle branch block and heart failure. Journal of Cardiovascular Electrophysiology 2003; 14:135-141
9. Auricchio A, Fantoni C, Regoli F, Carbucicchio C, Goette A, Geller C et al. Characterization of left ventricular activation in patients with heart failure and left bundle-branch block. Circulation 2004; 109: 1133-1139
10. Strik M, Regoli F, Auricchio A, Prinzen F. Electrical and Mechanical Ventricular Activation During Left Bundle Branch Block and Resynchronization. J. of Cardiovasc. Trans. Res. 2012; 5:117-126
11. Strauss DG, Selvester RH, Wagner GS. Defi ning left bundle branch block in the era of cardiac resynchronization therapy. Am J Cardiol 2011; 107(6):927-34
12. Massing GK, Thomas NJ. Anatomical Confi guration of the His Bundle and Bundle Branches in the Human Heart. Circulation 1976; 53(4): 609-621.
13. Vatasescu, R., Berruezo, A., Mont, L., Tamborero, D., Sitges, M., Silva, E., … Brugada, J. (2009). Midterm “super-response” to cardiac resynchronization therapy by biventricular pacing with fusion: insights from electro-anatomical mapping. Europace, 11(12), 1675–1682.
14. Radu DA, Iorgulescu CN, Bogdan SN, Ene E, Vatasescu R (2017). Left bundle branch block is incomple in the majority of patients with heart failure due to systolic left ventricular dysfunction: a simple intraprocedural demonstration. Journal of the American College of Cardiology, Volume 69, Issue 11, Supplement, 21 March 2017, Page 390.
15. David O. Martin et al, Adaptive CRT Study Investigators. Investigation of a novel algorithm for synchronized left-ventricular pacing and ambulatory optimization of cardiac resynchronization therapy: Result of the adaptive CRT trial. Heart Rhythm 2012: 9: 1807-1814.
16. Vatasescu RG, Berruezo A, Iorgulescu C, Vasile A, Constantinescu D, Dorobantu M. New Algorhythm for Pacing with Optimal Fusion During Cardiac Resynchronization Therapy Induces Extensive Reverse-Remodeling in Heart Failure Patients With Normal Atrio-Ventricular Conduction and Concordant Left Ventricular Lead Position. Circulation, November 3, 2009, Volume 120, Issue Suppl 18.
 This work is licensed under a
This work is licensed under a