Adrian Bucșa1, Cristina Bucșa2, Costel Matei1, Cristina Chirion2, Marian Croitoru1
1 „Prof. Dr. C. C. Iliescu” Emergency Institute for Cardiovascular Diseases, Bucharest
2 Fundeni Clinical Institute, Bucharest
Contact address:
Adrian Bucsa, MD, „Prof. Dr. C. C. Iliescu” Emergency Institute for
Cardiovascular Diseases, Bucharest
E-mail: abucsa@yahoo.com
CASE PRESENTATION
We present the case of a 45-year-old female patient admitted for increases in the values of the blood pressure and of the serum creatinine during the last four weeks. The patient underwent a renal transplantation fourteen weeks ago. She was diagnosed with chronic renal failure when she was 33-year-old and after several years of conservative treatment she entered in the hemodialysis program. After four months she received a kidney from her brother. The post-transplantation outcome was favourable and she was discharged 3 weeks after the surgery with a serum creatinine of 1.6 mg/dl and with normal blood pressure with only minimal medication (metoprolol 50 mg bid). At 10 weeks post-transplant there was a progressive increase in the blood pressure values to about 170/100 mm Hg and a gradual increase in the serum creatinine to 2.2 mg /dl and subsequently to 3.7 mg/dl. The investigations conducted by the nephrologist included among other tests, a Doppler ultrasonography of the renal graft. This examination showed turbulent flow proximal to the arterial anastomosis with a maximum velocity of 180 cm/s; the blood flow at the level of the interlobar arteries had a slow ascending slope and the resistance index (RI) at this level was 0.5. These parameters are strong indicators for a high-grade stenosis in the transplant renal artery1. The patient was sent to the department of interventional cardiology for confirmation of the diagnosis and invasive treatment with angioplasty and stenting.
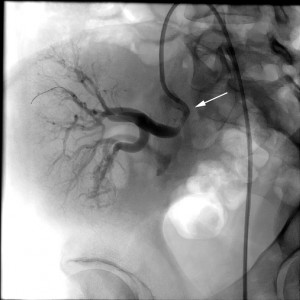
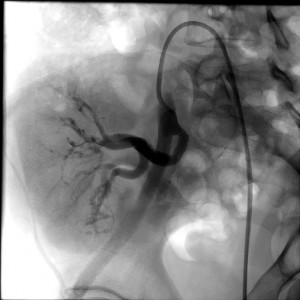
The physical exmination was not remarkable and the routine electrocardiogram and echocardiogram showed no abnormalities. The lab data indicated mild anemia (Hb=11.2 g/dl) and thrombocytopenia (131.000/mm3) and a serum creatinine of 3.4 mg/dl. The transplanted kidney was, in this case, placed in the right iliac fossa, the renal artery was connected end-to-end to the internal iliac artery of the recipient and the renal vein was connected end-to-side to the external iliac vein; the ureter was anastomosed with the bladder. The patient was premedicated with 250 mg aspirin and 300 mg clopidogrel the day before the intervention. The arterial approach was made by inserting a 6F sheath in the left femoral artery. After that, a diagnostic catheter JR 4.0 was advanced in cross-over into the right common iliac artery and subsequently in the right internal iliac artery. Manual injection of contrast medium confirmed the presence of 90% stenosis at the presumed site of surgical anastomosis with the graft artery (Figure 1). Angioplasty of the lesion was decided and performed by the direct implantation of a Herculink Elite renal stent, 5.5/18 mm, expanded at 11 atm. The angiographic result was very good (Figure 2). The postprocedural outcome was complicated by the formation of a pseudo-aneurysm at the puncture site, which was resolved by manual compression. The blood pressure normalised whithin 48 hours and a Doppler ultrasonography performed in fifth day after the procedure showed a normal flow in the interlobar arteries with an RI of 0.63. The serum creatinine values dropped in the first 48 hours at 2.2 mg/dl but after that rose again to 3.8 mg/dl in the seventh day, decreasing again at 2.1 mg/dl at 14 days and 1.6 mg/dl at one month after the stent implantation. This evolution, with initial decrease followed by gradual increase and return to normal was interpreted as an episode of contrast induced nephropathy. It is known that the renal grafts may be particularly sensitive to ischemia and this can amplify the effects of other injuries, like the contrast media administration2. Also, the calcineurin inhibitor that the patient took as an immunosuppresive agent can have a deleterious effect on the allograft function.
The patient was discharged with double antiplatelet medication (aspirin 100 mg and clopidogrel 75 mg), statin, beta-blocker and, of course, the post-transplant medication. The follow-up was made at 1, 3, 6 and 12 months. The values of the serum creatinine and the blood pressure were stable and a Doppler examination performed at six months showed an RI of 0.7 and a maximum velocity of 103 cm/s. At six months the aspirin was discontinued due to the fear of gastric bleeding that may have occur. At 12 months there was a discussion between the cardiologist and the nephrologist about the oportunity of continuing colpidogrel administration and the decision was to continue this medication for the next 12 months.We don’t expect to have any further problems with the stent because, as in all bare metal stent cases, the restenosis can occur only in the first 6 months after implantation.
DISCUSSION
There are several causes of impaired blood flow to the renal allograft. The lesions situated in the iliac artery, proximal to the anastomosis, are often of atherosclerotic origin while those found in the allograft’s artery are often due to progressive stenosis at the surgical anastomosis site. Transplant renal artery stenosis is more often found in the recipients of living donor kidneys (as is the case of our patient) than in those of deceased donor grafts3. The explanation is the difference in the surgical technique for the arterial anastomosis. In living donor transplants the end of the donor renal artery is connected directly to the side of the recipient’s internal iliac artery, while in deceased donor transplants, a patch of donor aorta connected to graft’s artery is sewn to the recipient’s iliac artery. This latter surgical technique (which, obviously can not be used in living donor transplants) is less likely to cause stenosis at the origin of the transplant renal artery4.
Table 14 summarizes the clinical presentations of the transplant artery stenosis. Of note, the presence of the bruits or murmurs in the area of the transplanted kidney can be misleading and is not necessarily an indicator for a vascular stenosis. The Doppler examination for the diagnosis must be performed by experienced operators because of unusual anatomic features and ultrasound angles found in the pelvic area in this kind of situations. Magnetic resonance arteriography can also be used as a diagnostic tool but it is reported to have a high rate of false positive results5. The treatment of choice is the angioplasty with stenting but surgical correction might be needed in case of repeated restenosis.
Table 1. Common clinical features of transplant recipients with renal artery stenosis
| Symptoms/signs |
| De novo hypertension any time posttransplant |
| Unexplained worsening of blood pressure control |
| Volume retention |
| Worsening renal graft function |
| Worsening renal graft function after angiotensin II inhibition |
| Bruits over the allograft |
The experience of our department of invasive cardiology in this field consists in three case of angioplasty and stenting and one with balloon angioplasty only. The case we presented here is the most recent of all four. In all cases the angiographic results were good and the clinical improvement was evident and stable in time.
SUMMARY
The increase in number of renal transplants in the recent years led to the appearance of a less known pathology until now: the transplant renal artery stenosis. The clinical features that are usually worsening hypertension and deterioration of the graft’s function with rise in the serum creatinine’s values. The cause is often a progressive stenosis at the site of the arterial anastomosis and the diagnosis is generally made by Doppler ultrasound examination. The endovascular treatment consisting in angioplasty with stenting leads to good results both immediately and in long-term, and can save the transplanted kidney. The renal graft’s function can be transiently impaired due to the combined effect of ischemia, iodinated contrast media administration and other drugs that may interfere.
Conflict of interest: none declared.
References
1. Baxter GM. Ultrasound of renal transplantation. Clin Radiol 2001; 56: 802-818.
2. Napoli V, Pinto S, Bargellini I, et al. Duplex doppler sonography of transplant renal artery stenosis before and after renal stenting. Eur Radiol 2002; 12:796-803.
3. Curtis JJ. Hypertension and kidney transplantation. Am J Kidney Dis 1986; 7:181-196.
4. FG Cosio, SC Textor. Hypertension after transplantation. In Weir RM, Medical management of kidney transplantation,Ed. Lippincott Williams& Wilkins, 2005.
5. Loubeyre P, Cahen R, Grozel F, et al. Transplant renal artery stenosis. Transplantation 1996; 62:446-450.
 This work is licensed under a
This work is licensed under a