Irina Spînu1, Ioana Ghiorghiu1, P. Platon1, Carmen Ginghină1,2, Ioana Lupescu3, R. Capşa3
Article received on the 26th of September 2012. Article accepted on the 15th of October 2012.
1 ”Prof. C.C. Iliescu” Emergency Institute for Cardiovascular Diseases Bucharest
2 “Carol Davila” University of Medicine and Pharmacy Bucharest
3 Fundeni Clinical Institute
Dr. Irina Spânu, ”Prof. Dr. C.C. Iliescu” Emergency Institute for Cardiovascular Diseases Bucharest
Coarctation of the aortic isthmus is a localized narrowing of the aorta situated at the junction between the distal aortic arch and the descending aorta, immediately beneath the origin of the left subclavian artery, at the insertion of the arterial ligament. It is a relatively frequent malformation, representing 5-8% of the total congenital heart conditions. From the anatomical point of view we have: a localized form – the most frequent, a diffuse form – it interests the aortic arch and the aorta distal from the origin of the left subclavian artery and a third form – atypical coarctation of the aorta (the aortic arch, ascending aorta, abdominal aorta, descending thoracic aorta).
CASE PRESENTATION
Patient BC, aged 17, diagnosed with coarctation of the aortic isthmus and bicuspid aortic valve in October 2011 is admitted for cardiologic evaluation. Clinically she is asymptomatic, with blood pressure values kept within normal limits with antihypertensive treatment. We mention that the patient also has Turner’s syndrome, confirmed by karyotyp (45X) in December 2011, with the following manifestations: stature hypotrophy secondary to growth hormone deficit (under substitutive therapy until April 2012), primary ovarian insufficiency – expressed through amenorrhea (treated with progesterone), discrete hypothyroidism (treated with levothyroxinum since the age of 13) and multiple cardiovascular malformations syndrome.
Physical examination on admission: patients with hypotrophy stature (W: 61 kg, H: 1.60 m), blood pressure (BP)= 140/60 mmHg measured at the superior limbs, bilaterally, undetectable at the inferior limbs, pulse = 60 beats per minute, rhythmic heart beat, diastolic murmur in the aortic area, grade III/IV left subclavicular systolic murmur radiating to the entire cardiac area and interscapular dorso-vertebral region, ample, symmetrical pulse on both radial arteries, faint pulsation was detectable in both femoral arteries and no pulsation could be felt in the dorsalis pedis and posterior tibial arteries, bilaterally.
The ECG (Figure 1) shows a narrow-complex regular rhythm at 70 beats per minute, PR interval 0.12 s, QRS axis at 60 degrees.
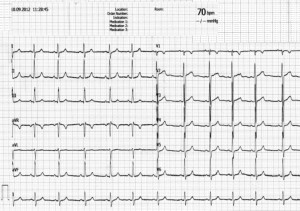
Figure 1. ECG: regular rhythm at 70 beats per minute, PR interval 0.12 s, QRS axis at 60 degrees with normal QRS morphology.
Chest X-ray (Figure 2): heart apex located above the diaphragm, superior arch reduced in dimensions, without thoracic aorta dilatations, without signs of rib erosion; pleuropulmonary aspect are within normal limits.

Figure 2. PA thoracic X-ray: heart apex located above the diaphragm, reduced superior arch dimensions, pleuropulmonary aspect within normal limits.
Transthoracic echocardiography (Figures 3 and 4): revealed normal size of the heart cavities, both left and right ventricular contractility with the range of normal values, bicuspid aortic valve (anterior and posterior cusps) – with cusps of different sizes (the anterior cusp was larger); second degree aortic regurgitation, normally sized aortic arch, with coarctation of the descending aorta at the isthmus – with a maximum gradient of the coarctation of 70.7 mmHg and maximum systolic velocity of 3.97 m/s in the descending aorta.
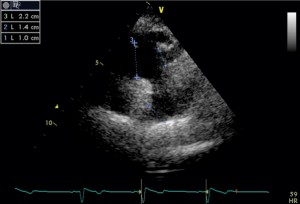
Figure 3. 2D echocardiography, suprasternal short-axis view: normal sized aortic arch, coarctation of the descending aorta at the isthmus.
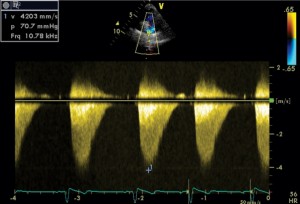
Figure 4. 2D echocardiography, suprasternal short-axis view: the continuous-wave Doppler interrogation showed a peak gradient of 70.7 mmHg.
Thoracic Magnetic Resonance Investigation with contrast (Figure 5): short stenosis, apparently large at the aortic isthmus, with a diaphragmatic aspect, located immediately caudally of the origin of the left subclavian artery, with a minim dilatation of the poststenosis aortic segment (24 mm); minimum thoracic collateral circulation.

Figure 5. Thoracic MRI with contrast: short stenosis, apparently large at the aortic isthmus, immediately caudal of the emergence of the left subclavian artery (arrow); minimal dilatation of the poststenotic aortic segment; minimal thoracic collateral circulation.
Considering the differences between the clinical manifestations (the significant differences between upper and lower limbs BP and pulse amplitude) characteristic to a tight aortic coarctation and the imagistic data, echocardiography and MRI, suggesting a large aortic stenosis it is decided to perform an invasive angiographic exploration.
Aortic arch arteriography (Figure 6): revealed a short stenosis area located immediately below the origin of the left subclavian artery, determining a 62 mmHg pressure gradient at that level. The following aortic diameters were measured: aortic arch 14.42 mm, stenosis area 5.17 mm, descending aorta 12.55 mm. The arteriographic aspect is suggestive for a tight aortic isthmus stenosis, with a recommendation for surgical correction.
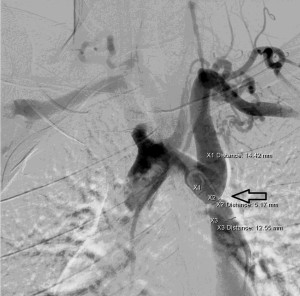
Figure 6. Aortic arch arteriography: short stenosis area located immediately below the origin of the left subclavian artery. Diameters: aortic arch (XI): 14.42 mm, stenosis area (X2): 5.17 mm, descending aorta (X3): 12.5 mm.
Discussions
The particularities of the case consist of the presence of complex cardiovascular malformations (tight aortic coarctation, bicuspid aortic valve with moderate aortic insufficiency) accompanied by a genetic syndrome with reduced frequency in the general population (Turner’s syndrome). We also notice the differences between the clinical manifestations – specific for a tight coarctation of the aorta (the significant difference between the upper and lower limb concerning BP and pulse amplitude) and the echocardiographic aspect (systolic velocities increased exclusively at the level of the stenosis) corroborated with the one revealed by the magnetic resonance investigation – suggestive for a large coarctation of the aorta. These differences justified the use of arteriography in order to establish the exact severity of the coarctation, as well as determining a proper therapeutic conduit – in the discussed case: surgical correction for a tight coarctation of the aorta.
Conflict of interests: none declared.
Bibliography
1. Ginghină C. Mic tratat de cardiologie. Editura Academiei Române, Bucureşti 2010: 575-577.
2. Webb Gd, Smallhorn Jf, Therrien J, Congenital heart disease, in Bonow RO, Mann DL, Zipes DP, eds. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 9th ed. Philadelphia, Saunders Elsevier; 2011: cap.65
3. Fraser CD Jr., Carberry KE. Congenital heart disease, in Townsend CM, Beauchamp RD, Evers BM, Mattox Kl, eds. Sabiston Textbook of Surgery. 18th ed. Philadelphia, Saunders Elsevier; 2007: cap.60.
 This work is licensed under a
This work is licensed under a