Marin Postu1, Adrian Bucșa1, Mihaela Mihăilă1, Constantin Gîngu2, Marian Croitoru1
1 ”Prof. Dr. C.C.Iliescu” Emergency Institute for Cardiovascular Diseases, Bucharest, Romania
2 Fundeni Clinical Institute, Bucharest, Romania
Contact address:
Adrian Bucșa, MD
”Prof. Dr. C.C.Iliescu” Emergency Institute for Cardiovascular Diseases, Bucharest, Romania. E-mail: abucsa@yahoo.com.
A 63-years-old female patient is admitted in our center for claudication in the right tight at about 20 meters. The symptoms developed gradually over the last year. She has the following risk factors: dyslipidemia, hypertension, altered glucose tolerance. She is slightly obese, with a BMI of 27 kg/m², has normal blood pressure (110/60 mm Hg) after medication and the pulse
in the right femoral artery is very weak. Among the lab tests we find mild hyperglycemia (121 mg/dl) and hypercholesterolemia (204 mg/dl), and normal values for the hemoglobin (13 g/dl) and creatinine (1.06 mg/dl). An invasive angiography performed five months before via the left femoral approach in another hospital revealed a 90% stenosis in the common right iliac artery, with no other major lesions in the arteries of the lower limbs. After premedication with aspirin and clopidogrel we scheduled the patient for an iliac angioplasty in the next morning.
The arterial approach was right femoral, with a 6F introducer sheath. The angiography confirmed the presence of a sub-occlusive stenosis in the right common iliac artery (Figure 1), with important calcification of the terminal aorta and of both common iliac arteries. 5000 IU of unfractioned heparin were given intravenousely. After the passage of a hydrophilic wire through the lesion into the abdominal aorta, a pre-dilatation was made, with a 6 mm diameter balloon. After that we implanted an Express LD stent, 8 mm diameter, 37 mm long and performed a post-dilatation with a 9 mm diameter balloon. The final result was good (Figure 2).
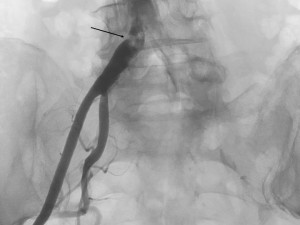
Figure 1. Sub-occlusive stenosis of the right common iliac artery; note the intense calcification of the terminal aorta and both iliac arteries.
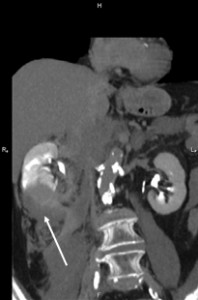
The patient was under observation on the cathlab floor during the next 60 minutes and after that the sheath was removed and hemostasis was achieved. She returned to her room but no longer then 15 minutes after she reported nausea, diaphoresis and weakness. Hypoglycemia was initially suspected but the glucotest showed a 260 mg/dl value of the serum glucose. The patient became hypotensive (systolic blood pressure 80 mm Hg) and soon after she complained of increasing pain in the right lumbar area. An ultrasound made at the bedside showed a right perirenal hematoma. The lab test indicated a dramatic decrease in the hemoglobin level, from 13 mg/dl to 8.0 mg /dl. The patient was practically in hemorrhagic shock. The decision was to transfer immediately the patient to the cathlab for an angiographic control. A new puncture of the right femoral artery was made, because the initial suspicion was an iliac rupture or perforation in the stent area, due to the extensive calcification of the arterial wall. The first injection of contrast media through the sheath showed that there was no problem with the stent. After that a global injection into the abdominal aorta, at the renal arteries level, was made, and a small effraction in the right renal parenchyma was observed (Figure 3). Selective intubation of the right renal artery was made with a JR 4.0 diagnostic catheter and that confirmed the source of bleeding in the right posterior segmental artery (Figure 4). Careful superselective intubation of this branch was performed (Figure 5), and small particles of gelatin sponge (Gelaspon) mixed with contrast media were delivered through the catheter. The embolization7 was successful in stopping the bleeding (Figure 6) but since there was about 20% of the renal parenchyma without vascularization and the patient still had important pain in the lumbar area, the decision was to transfer her to the urology department. A CT-scan (Figure 7) indicated a large subcapsular and retroperitoneal hematoma and also the presence of the contrast media in the urinary tract, an indication that the renal function was still preserved. In accordance with these findings, a renal lobectomy (partial nephrectomy) was performed, along with the evacuation of the hematoma. There was a parenchymal sparing intervention that preserved almost the entire kidney. The outcome was complicated by a pneumothorax after a central venous catheter insertion and by a right femoral hematoma following the two arterial punctures. However, after 14 days the patient was discharged in pretty good condition. One year later she has no claudication, the pulse in the right femoral artery is very good and the serum creatinine is normal.
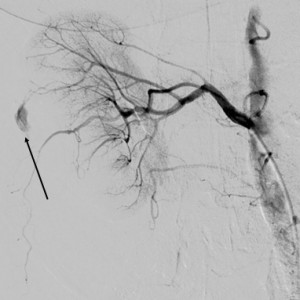
Figure 4. Selective injection in the right renal artery; arrow indicates the site of the effraction.
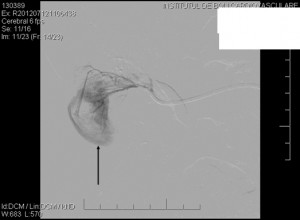
Figure 5. Superselective intubation of the “guilty” segmental artery; arrow indicates the large subcapsular hematoma.
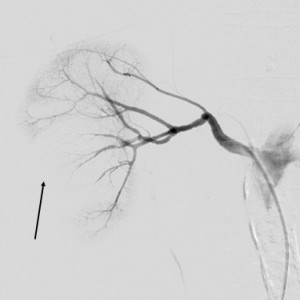
Figure 6. Result after embolisation: the bleeding has been stopped but about 20% of the renal parenchyma is not vascularised.
DISCUSSION
The hydrophilic guidewires are very often used in the peripheral procedures, especially in the angioplasties of the lower limb arteries. These are lubricated wires, with a soft-angled tip, that can easily surpass obstacles like stenosis or total occlusions. However they are also pretty stiff wires that can penetrate normal structures and create serious problems1-4. One basic rule in the interventional cardiology is that one should always watch the tip of the guidewire (both in coronary or peripheral procedures2). However, these slippery guidewires are not always easy to control and there are numerous reports of more or less severe accidents1-4. Some very experienced interventionalists say that if you had not had this type of complication until now than you had not done enough cases. It is most probable that the tip of the guidewire engaged unwillingly in the right renal artery and after that penetrated the right renal capsule, leading to this dramatic complication2,3. In fact, when we reviewed the case we observed on one single angio run, on very few frames (Figure 8), that the tip of the guidewire was not in the proper position. It is very clear that the immediate recognition of the perirenal hematoma was crucial5. It is most probable that the embolization of the renal artery branch was life-saving in this dramatic case. Also of note is the careful surgery that was performed, which led to the preservation of most of the right kidney.

Figure 8. Still frame of the predilatation; arrow indicates the tip of the guidewire engaged in the right renal artery and parenchyma.
SUMMARY
In the present days the interventions for peripheral artery disease are performed very frequently by the interventional cardiologists and radiologists. These interventions involve very often the use of the hydrophilic guidewires, which can be very useful tools but sometimes can also create serious problems. In this case, an iliac artery stenting was complicated by a right renal capsular perforation with the tip of the guidewire, that led to a large retroperitoneal hematoma and a clinical scenario of hemorrhagic shock. Fortunately, the complication was readily identified and treated, first by the embolization7 of the perforated arterial branch, and after that by the meaning of a conservative surgery that preserved most of the renal tissue. This case illustrates, in our opinion, that the number of potential complications that can appear during a coronary or peripheral intervention is very high6,7 but quick diagnosis, immediate action using personal or team experience, and tight co-operation with other medical specialties can lead to a positive result for the patient.
Conflict of interests: none declared.
References
1. Lee SY1, Kim SM, Bae JW, Hwang KK, Bae IH, Kim DW, Cho MC. Renal artery perforation related with hydrophilic guide wire during coronary intervention: successful treatment with polyvinyl alcohol injection. Can J Cardiol. 2012 Sep-Oct;28(5):612.e5-7. doi: 10.1016/j.cjca.2012.03.007. Epub 2012 May 8.
2. Bates MC1, Shamsham FM, Faulknier B, Crotty B. Successful treatment of iatrogenic renal artery perforation with an autologous vein-covered stent. Catheter Cardiovasc Interv. 2002 Sep;57(1):39-43.
3. Jeffrey M. Friedel, MD, Ramzi Khalil, MD, David Lasorda, MD. Treatment of Iatrogenic Renal Artery Perforation with a Covered Stent and Subsequent Rheolytic Thrombectomy. Vascular Disease Management, Volume 2 – Issue 4 – July/August 2005 Posted on: 9/5/08 0 Comments 8679 reads.
4. David J. Axelrod, MD, Hank Freeman, MD, Lev Pukin, MD, Jeffrey Guller, MD, Harold A. Mitty, MD. Guide Wire Perforation Leading to Fatal Perirenal Hemorrhage from Transcortical Collaterals after Renal Artery Stent Placement. Journal of Vascular and Interventional Radiology. Volume 15, Issue 9 , Pages 985-987, September 2004.
5. Bates MC, Shamsham FM, Faulknier B, Crotty B. Artery perforation during catheterization: Fighting with a catastrophe. Catheter Cardiovasc Interv 2002;57:44–46.
6. Zeller T, Frank U, Muller C, et al. Technological advances in the design of catheters and devices used in renal artery interventions: Impact on complications. J Endovasc Ther 2003;10:1006–1014.
7. Luca Favero, Salvatore Saccà, Carlo Cernetti, Giampaolo Pasquetto, Dimitris Nikas, Bernhard Reimers. Department of Cardiology, Mirano Hospital, Mirano, Italy. Superselective embolization of renal hemorrhage occurring after percutaneous coronary intervention. Cardiovascular revascularization medicine: including molecular interventions 01/2009; 10(1):62-5. DOI:10.1016/j.carrev.2007.11.008.
8. Soeren A Peters, Aydan Yazar, Stefan P Lemburg, Christoph M Heyer Institute of Diagnostic Radiology, Interventional Radiology, and Nuclear Medicine, BG Clinics Bergmannsheil, Ruhr-University of Bochum, Buerkle-de-la-Camp Platz, Bochum, 44791, Germany. Renal perforation and retroperitoneal hematoma: an unusual complication following cardiac catheterization. The International Journal of Cardiovascular Imaging (Impact Factor: 2.65). 01/2008; 23(6):805-8. DOI:10.1007/s10554-006-9202-8.


 This work is licensed under a
This work is licensed under a