Gabriela Mut-Vitcu1,3, Svetlana Mosteoru1,2,3, Romulus Timar1,4, Laura Gaita4, Dan Gaita1,2,3
1 “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania
2 Department of Cardiology, Institute for Cardiovascular Diseases, Timisoara, Romania
3 CardioPrevent Foundation, Timisoara, Romania
4 Department of Diabetes, Nutrition and Metabolic Disorders, Emergency County Hospital, Timisoara, Romania
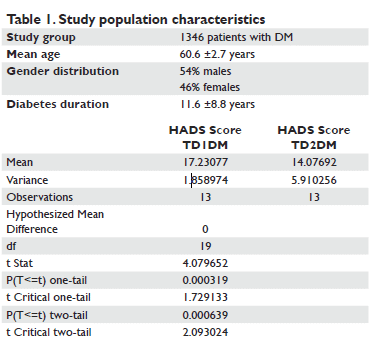
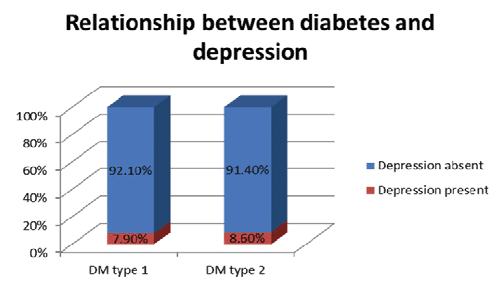
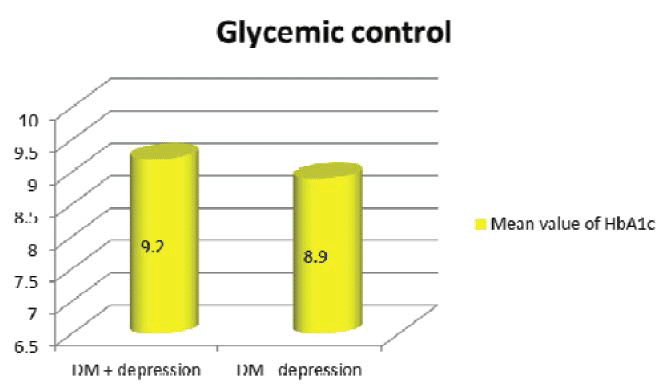
Abstract: Objectives – We have conducted a study aimed at uncovering if depressed diabetic patients have a higher incidence of cardiovascular complications and have also evaluated the relationship between the presence of depression and glycemic control in these patients. Methods – A cross-sectional study was conducted on 1346 patients suffering from DM admitted to the Diabetes Department of the Emergency County Hospital Timişoara, between January and December 2012. Results – Out of the 1346 patients included in our study 8.5% have been also diagnosed with depression. Depression was found in 7.9% of patients with type 1 DM, while the prevalence of depression was 8.6% in the type 2 DM category. There was a statistic significance between diabetes mellitus and depression (p <0.05). The mean value of HbA1c was 9.2% in patients suffering from both DM and depression and 8.9% in diabetic patients only. Patients with DM and depression were able to achieve the <8% HbA1c target in 29.31% of the cases, while those without depression in 32.59% of the cases. Our conclusions highlight the need for active screening for depression in diabetic patients due to the potential of this complication being overlooked and also in order to ensure that preventive action is taken.
Keywords: diabetes mellitus, depression, cardiovascular disease, life quality
INTRODUCTION AND OBJECTIVES
Recent studies have brought to light the fact that people with diabetes mellitus (DM) have twice the risk compared to the general population of developing long-term symptoms of depression or anxiety. This however is a two way pathway because depression is associated with hyperglycemia and increased risk for diabetic complications while relief of depression improves glycemic control1. The odds for depression are signifi cantly higher in women with DM rather than men, precisely due to the fact that depression overall is more likely to affect the female population1. However, a link between type 1 or 2 DM and depression was not established, possibly because many studies failed to fully characterize the depressed and non-depressed populations1. The complex relationship between depression and diabetes mellitus revolves around physical, physiological and genetic factors which until now remain uncertain. Depression may occur due to the hardships of advancing diabetes or to diabetes related abnormalities in neurohormonal function. On the other hand, depression doubles the risk of developing type 2 DM, independent of other risk factors. Moreover, in patients already diagnosed with type 2 DM, suffering from depression represents a risk factor for coronary heart disease and appears to accelerate the presentation of the ischemic heart disease1. It has long been recognized that mild forms of depression are found in up to two-thirds of patients hospitalized for acute myocardial infarction2, with major depression being found in ~15% of cardiovascular disease patients3. The negative implications of depression in patients suffering from diabetes include worsening glycemic control, nonadherence to treatment, poor metabolic control and increased risk of vascular complications (diabetic retinopathy, neuropathy and macrovascular complications)4. Furthermore, depression can lead to increased disability, decreased quality of life, more somatic symptoms, increased healthcare costs and even increased mortality4. There are however, certain limitations to studies published so far due to the lack of an adequate control group or the use of self-report questionnaires to document depression. If comparing the prevalence of depression in the diabetic population using formal psychiatric criteria, Anderson and all found a 11.4% prevalence of depression, while using self-report scales the prevalence rose up to 31.0% according to the same study1. Having in view the potential for further inquiry and the need to establish an in depth association between diabetes mellitus, depression and cardiovascular disease, we have conducted a study aimed at uncovering if depressed diabetic patients have a higher incidence of cardiovascular complications. We have also evaluated the relationship between the presence of depression and glycemic control as well as the presence of depression in patients suffering from diabetes mellitus.
MATERIAL AND METHODS
We have conducted a cross-sectional study on 1346 patients suffering from DM admitted to the Diabetes Department of the Emergency County Hospital Timisoara over the period of a year, between January and December 2012. We have obtained the permission of the ethics committee of the Timisoara Emergency County Hospital and all the principles of the Helsinki Declaration were fulfilled. All relevant information was extracted from patient charts: demographic data, DM type and duration, DM treatment, weight status (using the body mass index), glycated hemoglobin (HbA1c), presence of cardiovascular complications (coronary heart disease, stroke, peripheral artery disease and gangrene). Depression had been diagnosed by the hospital psychiatrist using the Hamilton Depression Scale. The presence or absence of diabetes mellitus was analyzed in connection to a number of variables such as HbA1c, body mass index (BMI), diabetes duration, presence or absence of cardiovascular disease and type of antidiabetic medication (insulin or oral antidiabetic drugs). All the data gathered was statistically processed using descriptive statistics and chi-square and unpaired student’s t test of EpiInfo software.
RESULTS
Out of the 1346 patients included in our study, more than half were males, 54%. The mean age was 60.6 years ±2.7 years SD and they had been diagnosed with diabetes mellitus for the past 11.6 ±8.8 years SD (Table 1). 8.5% of the entire population studied had been also diagnosed with depression. However, when dividing the patients by the type of diabetes they suffered from,
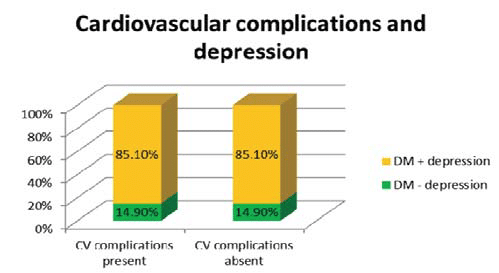
depression was found in 7.9% of patients with type 1 DM, while the prevalence of depression was 8.6% in the type 2 DM category (Figure 1A). In addition, two thirds of these patients had also anxiety besides depression. We have applied the HADS (Hospital Anxiety and Depression Scale) questionnaire to the patients diagnosed with depression in order to quantify the severity of their depression. We have matched equal groups of patients with DM type 1 and 2 and have applied the student t test uncovering a strong association between the type of DM and the severity of depression (p <0.01) (Figure 1B). Regarding glycemic control, the mean value of HbA1c was 9.2% in patients suffering from both DM and depression, and 8.9% in diabetic patients only (Figure 2). The prevalence of diabetic retinopathy was almost similar in patients diagnosed with depression (28.95%) compared to patients without depression (30.5%). There was a slight difference regarding diabetic neuropathy, where 62.28% suffering from depression had also been diagnosed with this complication, while 60.69% of diabetic patients without depression had neuropathy. We were able to compare the weigh status and the presence or absence of depression in the population we studied. Thus, 23.42% of the patients with depression had normal weight, 34.23% were overweight, 21.62% had stage 1 obesity, 11.72% stage 2 obesity and 9.01% stage 3 obesity. Patients with DM and depression were able to achieve the <8% HbA1c target in 29.31% of the cases, while those without depression were able to achieve this target in 32.59% of the cases. However, when set at <7% the target for HbA1c, 15.52% of patients suffering from depression were able to reach this target and only 13.48% of those without depression. We were not able to find any difference in cardiovascular complications in diabetic patients with or without depression (Figure 3), as well as regarding the type of medication prescribed.
Figure 1A. Relationship between diabetes and depression. 1B Association between the type of diabetes and the severity of depression.
Figure 2. Mean value of HbA1c in diabetic patients.
Figure 3. Relationship between cardiovascular complications and depression.
DISCUSSIONS
A growing body of research suggests that coexisting depression has a negative impact on patients suffering from diabetes. Previous studies have shown that depression is associated with poor glycemic control, increased risk of complications, decreased quality of life and increased health care utilization and costs5. There is considerable evidence that diabetes is a leading cause
of coronary heart disease (CHD) and is connected to increased CHD mortality. Moreover, accumulating evidence points to the association of depression to increased CHD mortality6. The prevalence of depression in various heart conditions ranges from 15% to 20%7. According to data from the World Health Organization, by the year 2020 depression will be the second leading cause of disability in developed countries8. In the large INTERHEART study, the four most important factors contributing to presentation with acute coronary syndromes were a comprehensive lipid profile using Apolipoprotein B/Apolipoprotein A ratio, smoking, psychosocial factors (predominantly depression, stress, life events and locus of control) and then diabetes. In the control group, the prevalence of major depression was about the same as in most non-cardiac populations (7%), but ~50% higher in the AMI group. However, this only contributed about 9% of the attributable risk, less than some of the other psychosocial factors9. Our results were not able to confi rm these fi ndings. These differences could possibly be explained by the fact that our cohort consisted mainly in a relatively young population (mean age 60.6 years old), who although having a high comorbidity burden in terms of diabetes complications had not yet developed major cardiovascular events. Moreover, our sample consisted mostly in male patients (54%), and previous studies suggested that the contribution of depression to chronic disease outcomes might be stronger in women due to differential coping mechanisms10. The association between depression and diabetes is complex and there is evidence that the association is bidirectional. People with established diabetes have higher rates of depression than the general population, while depression has become established as a risk factor for diabetes. There are several mechanisms to explain this association from the ‘‘psychological stress’’ resulting from the diagnosis and treatment of the physical illness, through the metabolic derangement leading to mood disturbance to alterations in cytokines and stress hormones11. The underlying mechanisms between depression and diabetes complications are multifactorial, impairing the ability of patients for self-care as well as leading towards lack of physical activity and in turn to obesity12. Our study has several potential limitations. First of all, the diagnosis of depression was not based on the gold standard of a clinical interview, but data was taken from patient history, being highly likely that some patients had not been yet diagnosed because they were not actively searched for depression. This should be considered for further research. An active screening for depression in patients with diabetes is necessary due to the potential of this complication being overlooked in a diabetes centered department. Second of all, this was a retrospective study, thus patients were not interviewed but data was collected from patient files.
CONCLUSIONS
Our conclusions highlight the need for active screening for depression in diabetic patients due to the potential of this complication being overlooked and also in order to ensure that preventive action is taken. Further research will be necessary to disentangle causal relationships among depression, behavioral risk factors (adherence to medical regimens), diabetes complications, cardiovascular disease and mortality. Comorbid depression and diabetes is often an under- recognized clinical problem and does not only impair the patient’s quality of life but also adds difficulties to the self-management of diabetes13. It has been pointed out that depression in diabetes results in a high economic burden to society in terms of both direct and indirect costs14,15. It is therefore mandatory that careful attention should be rendered to this segment of the population in order to achieve an optimum management of depression in primary care settings which would then result in appreciable alleviation of suffering in those with diabetes and depression. More so, failure to manage depression may compromise the management of diabetes itself, which can have a severe impact on the quality of life itself.
Conflict of interests: none declared
References
1. Anderson RJ, Freedland KE, Clouse RE, Lustman PJ, The prevalence of comorbid depression in adults with diabetes, Diabetes Care June 2001 vol. 24 no. 6 1069-1078
2. Cay EL, Vetter N, Philip AE, Dugard P. Psychological status during recovery from an acute heart attack. J Psychosom Res 1972;16:425– 435
3. Colquhoun DM, Bunker SJ, Clarke DM, Glozier N, Hare DL, Hickie IB, Tatoulis J, Thompson DR, Tofl er GH, Wilson A, Branagan MG, Screening, referral and treatment for depression in patients with coronary heart disease. Med J Aust 2013;198: 483–484.
4. Campayo A, Gomez-Biel CH, Lobo A, Diabetes and depression, Curr Psychiatry Rep (2011) 13:26–30
5. Egede LE, Nietert PJ, Zheng D, Depression and All-Cause and Coronary Heart Disease Mortality Among Adults With and Without Diabetes, Diabetes Care 28:1339–1345, 2005
6. Carney RM, Blumenthal JA, Catellier D: Depression as a risk factor for mortality after acute myocardial infarction. Am J Cardiol 2003, 92:1277–1281
7. Lichtman JH, Bigger JT, Blumenthal JA, Frasure-Smith N, Kaufmann PG, Lespérance F, Mark DB, Sheps DS, Taylor CB, Froelicher ES, Depression and coronary heart disease: recommendations for screening, referral and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association, Circulation 2008; 118: 1768-1775
8. Murray CJ, Lopez AD, Global mortality, disability and the contribution of risk factors: Global Burden of Disease Study. Lancet 1997; 349: 1436-1442
9. Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L, INTERHEART Study Investigators. Effect of potentially modifi able risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case–control study. Lancet 2004;364:937–952.
10. Demmer RT, Gelb S, Suglia SF, Keyes KM, Aiello AE, Colombo PC, Galea S, Uddin M, Koenen KC, Kubzansky LD, Sex differences in the association between depression, anxiety, and type 2 diabetes mellitus. Psychosom Med 2015;77:467–477
11. De Hert M, Dekker J.M, Wood D, Kahl K.G, Holt R.I.G, Möller H.-J, Cardiovascular disease and diabetes in people with severe mental illness position statement from the European Psychiatric Association (EPA), supported by the European Association for the Study of Diabetes (EASD) and the European Society of Cardiology (ESC), European Psychiatry 24 (2009) 412–424
12. Marta Novak, Istvan Mucsi, Connie M. Rhee, Elani Streja, Jun L. Lu, Kamyar Kalantar-Zadeh, Miklos Z. Molnar, Csaba P. Kovesdy, Increased Risk of Incident Chronic Kidney Disease, Cardiovascular Disease, and Mortality in Patients With Diabetes With Comorbid Depression, Diabetes Care Nov 2016, 39 (11) 1940-1947
13. Holt RIG, de Groot M, Golden SH. Diabetes and Depression. Current diabetes reports. 2014;14(6):491.
14. Egede LE, Zheng D, Simpson K: Co-morbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes Care 25:464–470, 2002
15. Finkelstein EA, Bray JW, Chen H, Larson MJ, Miller K, Tompkins C, Keme A, Mandersheid R: Prevalence and costs of major depression among elderly claimants with diabetes. Diabetes Care 26:415–420, 2003.
 This work is licensed under a
This work is licensed under a