Anca-Maria Popară-Voica1, Ioana Ghiorghiu1, Claudia Folescu1, Carmen Ginghină1,2
Article received on the 27th of September 2012. Article accepted on the 6th of October 2012.
1 ”Prof. C. C. Iliescu” Emergency Institute for Cardiovascular Diseases Bucharest
2 “Carol Davila” University of Medicine and Pharmacy Bucharest
Dr. Anca-Maria Popară-Voica, ”Prof. C. C. Iliescu” Emergency Institute for Cardiovascular Diseases Bucharest
E-mail: poparaanca@yahoo.com
Case presentation no. 1: M.A.R., 27 years old, F
Personal history: Patient documented with patent ductus arteriosus (PDA), with ligatured of PDA in 1995 in the stage of severe pulmonary arterial hypertension (Qp/Qs = 3.03; pulmonary arterial hypertension represents 75% of the systemic arterial hypertension), with a postoperative progressive evolution of the pulmonary arterial hypertension up to class III NYHA heart failure symptoms. Cardiac catheterization was repeated in 2010 and it revealed increased of total pulmonary resistance (25 Wood units, of which 83% were arteriolary). Clinical evolution was initially favorable under treatment with specific pulmonary vasodilators such as phosphodiesterase inhibitors (Sildenafil), diuretics and oral anticoagulants. The patient accuses the graduate loss of her functional pulmonary capacity (dyspnea when climbing one flight of stairs).
The clinical examination shows a hemodynamically stable patient, BP=100/65 mmHg, pulse = 88 bpm, rhythmic heart beat, second heart sound splitting, accentuated P2 component in the pulmonary auscultation area, diastolic murmur in the II left parasternal space, a systolic murmur in the tricuspid auscultation area and discrete lower-limb edema.
The ECG shows sinus rhythm, pulse = 86 bpm, QRS axis at 120 degrees, right atrium anomaly, elements of biventricular hypertrophy with secondary repolarization modifications:
Postero-anterior and left profile chest Xray shows: right heart hypertrophy, discretely prominent middle left arch in the superior 2/3, moderate dilatation of the central pulmonary arteries, pulmonary circulation cephalization. Pleuropericardial adhesion on the left inferior arch (Figure 1A and 1B).


Figure 1A and 2B. Postero-anterior and left profile chest X-ray shows: right heart hypertrophy, discretely prominent middle left arch in the superior 2/3, moderate dilatation of the central pulmonary arteries, pulmonary circulation cephalization. Pleuropericardial adhesion on the left inferior arch.
The echocardiography reveals important right cavity dilatation (right ventricle (RV) 52 mm, TAPSE 17 cm, pulmonary artery acceleration time = 63 ms), normal global systolic function of the left ventricle (LV), slight systolic dysfunction of the RV, severe pulmonary hypertension (PAPs 140 mmHg), dilatation of the pulmonary trunk and pulmonary artery (PA) (pulmonary artery ring = 29 mm, pulmonary trunk 31 mm, left branch 18 mm, right branch 21 mm), mild pulmonary regurgitation and moderate tricuspid regurgitation (39 mm tricuspid ring).
The six minute walk test was used to estimate functional exercise capacity and it showed a decrease of effort capacity compared to previous evaluations (she walked 280 m, with palpitations and dyspnea occurring at 120 m as opposed to 500 in 6 minutes in earlier tests). Based on the clinical and paraclinical evaluations, the patient is considered stable, but her functional capacity is unsatisfactory. Considering this situation it is decided to adjust the treatment with a second pulmonary specific vasodilator (a type of endothelin receptor antagonist – Bosentan).
Case presentation no. 2: C.M.L., 38 years old, F
Personal history: the patient was diagnosed in 2008 with severe idiopathic pulmonary arterial hypertension, in New York Heart Association functional class IV with a relatively good response to the specific pulmonary treatment with two vasodilators (Sildenafil + Bosentan). The treatment with Bosentan had to be interrupted in november 2011 due to significant hepatic cytolisys. The patient complained about the progressive loss of her effort capacity, which was interpreted in the context of renouncing the treatment with Bosentan.
The clinical examination concluded that the patient is hemodynamically stable, BP = 90/60 mmHg, pulse 65 bpm, rhythmic heart beat, splitting of second heart sound, prominent P2 component in the pulmonary area, diastolic murmur in the IInd left parasternal space, systolic murmur in the tricuspid area, without pulmonary or systemic congestion.
The six minute walk test used to estimate functional exercise capacity showed the decrease of the capacity to perform physical efforts (she walked 320 m, with palpitations after 120 m and with dyspnea and fatigue after 160 m).
The ECG indicated the presence of sinus rhythm, AV 68 bpm, QRS axis at 100 degrees, elements of RVH with secondary repolarization anomalies:
Postero-anterior and left profile chest X-ray shows: enlargement of the right heart, left middle arch is intensely prominent in its superior 2/3 (the infundibulum of the PA), significant dilatation of the central pulmonary arteries, with a sharp reduction of their peripheral caliber. Right base pleuropulmonary adhesion (Figure 2A and 2B).

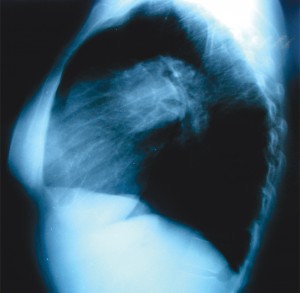
Figure 2A and 2B. Postero – anterior (A) and left profile chest X-ray (B) shows: enlargement of the right heart, left middle arch is intensely prominent in its superior 2/3 (the infundibulum of the PA), significant dilatation of the central pulmonary arteries, with a sharp reduction of their peripheral caliber. Right base pleuropulmonary adhesion.
The echocardiography reveals dilated right cavities, normal global systolic function of the LV, preserved global systolic function of the RV (RV 44mm, TAPSE 20mm, TDE 182 ms), severe pulmonary hypertension (PAPs 98 mmHg), aneurismal dilatation of the pulmonary artery (pulmonary artery ring = 28mm, pulmonary artery trunk = 56 mm, right branch 35 mm, left branch 31 mm), mild pulmonary and tricuspid regurgitations.
Considering that, it is decided to introduce a second pulmonary specific vasodilator, an endotheline receptor antagonist – ambrisentan. It is recommended for patients who had to interrupt treatment with Bosentan due to hepatic cytolysis.
Discussion
Although the medical condition seems to be the same, pulmonary arterial hypertension, the radiological examination reveals notable differences between the two cases presented. The patient suffering from idiopathic pulmonary hypertension has a slight increase of the cardio-thoracic index, with an aneurismal dilatation of the pulmonary trunk and branches of the pulmonary arteries. For the same pressure values (measured by cardiac catheterization), the patient suffering from a corrected congenital affliction has a significantly increased cardio-thoracic index, with a moderate dilatation of the trunk and branches of the pulmonary arteries visible on the chest X-ray.
The echocardiography confirms the data revealed by the radiological examination. The patient suffering from idiopathic pulmonary arterial hypertension has a mild dilatation of the right heart cavities, having a preserved contractile function of the RV. The patient with a congenital heart condition has a significant dilatation of the right cavities accompanied by a systolic dysfunction of the RV.
It is important to note the different reactions of the heart, trunk and branches of the pulmonary arteries to similar values for the arterial pulmonary pressures. In the case of the corrected ACP it is initially a case of pulmonary hypertension owed to the increased blood flow and (after the late repair of the defect) it had an independent evolution due to the increase in the resistance in the pulmonary arterial system. The predominance of the right heart condition can be noticed after the closure of the arterial canal, but with elements suggesting biventricular affliction present on the ECG. The literature documented the association of ACP and pulmonary artery dilatation. In the case presented here we could see the moderate dilatation of the pulmonary artery which has not progressed in time. On the other hand, in the case of idiopathic pulmonary hypertension we could see the aneurismal dilatation of the pulmonary artery, a case seldom encountered in literature descriptions. We must also note the favorable response to pulmonary vasodilators obtained in this case, with a significant improvement of the life span.
Confllict of interests: none declared.
Bibliography
1. Carmen Ginghină. Hipertensiunea pulmonară în practica de cardiologie. Editura Academiei Române, 2006.
2. Carmen Ginghină. Mic tratat de cardiologie. Editura Academiei Române, 2010.
3. Webb, W. Richard.; Higgins, Charles B. Thoracic Imaging: Pulmonary and Cardiovascular Radiology 2nd Edition, Lippincott Williams & Wilkins (LWW), 2010.
 This work is licensed under a
This work is licensed under a