Marian Simion1, Razvan Radu1, Anca Popară1, Mihaela Mihăilă1, Lucian Zarma1, Eduard Apetrei1,2
1 “Prof. Dr. C.C. Iliescu” Emergency Institute for Cardiovascular Diseases, Bucharest, Romania
2 “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania
Contact address:
Marian Simion, MD
“C.C. Iliescu” Emergency Institute for cardiovascular diseases, Bucharest.
We report the case of a patient aged 58 years, who required a preoperative cardiologic evaluation before a surgical mastectomy intervention of Madden type. At the time of the assessment the patient was symptomatic with dyspnea and fatigue with a low threshold of effort in the last 4 months and intermittent claudication of lower limbs manifested by buttocks pain after about 200-300 m of walking, relatively stationary in the past 8 years.
As regards her pathological history, we keep in mind the diagnosis in 2003 of a right breast cancer of the invasive ductal carcinoma type, for which she received chemotherapy with 5-Fluorouracil (12 sessions), Cyclophosphamide (12 sessions) and Epirubicin (1 session), narrow-field radiotherapy (25 sessions) and a Madden type surgical intervention was performed. In 2013, the patient is diagnosed with contralateral breast cancer of similar pathological type, for which a chemotherapy with 6 sessions of Epirubicin, 5-Fluorouracil and Cyclophosphamide was initiated again.
We keep in mind out of her personal physiological history the spontaneous occurrence of menopause at 45 years and a history of 5 pregnancies, including one miscarriage. Regarding the patient’s lifestyle peculiarities, we mention that she is a former smoker (15 packs/year 12 years ago) and she made performance sports (athletics and rowing) until the age of 20 years. The patient associated a cardiovascular and neoplastic family history.
The cardiovascular history begins in September 2013 when, at the thoracic-abdominal-pelvic CT scan performed for staging of breast cancer, important vascular calcifications are observed at the level of the infrarenal aorta, arranged circumferentially and complete occlusion of the terminal aorta (Figure 1). However, at that time there were no further cardiovascular investigations performed and the patient began a monthly chemotherapy with a regimen that also included Epirubicin, a preparation belonging to the anthracycline class. After 6 months, the patient began to develop symptoms of heart failure and a first cardiologic assessment was requested, which revealed on echocardiography the presence of a moderate LV systolic dysfunction (left ventricular ejection fraction 40%), mitral regurgitation grade III and a fine blade of pericardial fluid, which is why chemotherapy was stopped. The peripheral arterial Doppler examination confirmed the presence of the aortoiliac occlusive disease with refilling of the common iliac arteries by collaterals, but also highlighted the fact that there was no hemodynamically significant distal vascular stenosis.

Figure 1. Abdominal-pelvic computed tomography with dye. We observe the presence of parietal aortic calcifications arrange circumferentially, the absence of contrast uptake in the terminal aorta lumen (black arrow) and significant dilation of lumbar arteries (white arrow).
The general physical examination on current admission reveals an underweight patient (height: 1.57 m, weight: 45 kg, body mass index (BMI) 18.02 kg/m2). The cardiovascular examination identified the presence of purling and apical systolic murmur grade IV/VI irradiated in the axilla and left parasternal systolic murmur grade III/VI. Peripheral pulse is absent in the femoral, popliteal, pedis and posterior tibial artery bilateral and hardly perceptible in the right radial and ulnar artery, without identifying audible vascular murmurs. We notice the presence of a reduced systolic blood pressure of 20 mmHg in the right upper limb compared to the contralateral limb.
Biologically, the patient presented on admission an ingravescence of the kidney disease on the background of intense diuretic therapy followed at home, improved in dynamics up to basal value of creatinine clearance of 50 ml/min. Moreover, the inflammatory samples showed elevated values (ESR 59 mm/h, C-reactive protein (CRP) 4 mg/dl). Determination of the B-type natriuretic peptide (BNP) showed a value of 3000 pg/ml.
The chest radiography reveals the bulging of the right lower arch and double contour appearance at this level, together with the flattening of the left middle arch, and the microvolt electrocardiogram reveals diffusely flattened T waves at the level of limb derivatives.
The transthoracic echocardiography revealed a dilated LV (diastolic diameter 58 mm, systolic diameter 48 mm, indexed values 42 mm/m2, respectively 34 mm/m2) with severe global systolic dysfunction (ejection fraction 24% by the biplane Simpson method) with diffuse global hypokinesia of the walls; LV diastolic dysfunction of restrictive type (E/A ratio = 3.2) with increased LV filling pressures (E/E’ ratio = 20). The patient associated a severe mitral regurgitation with eccentric jet to the AS free wall by mixed (restrictive and degenerative) mechanism. The right ventricle was slightly dilated (36 mm) with global dysfunction (tricuspid annular systolic excursion (TAPSE) 9 mm, free wall systolic velocity 7.2 cm/sec). We note the presence of pericardial fluid disposed circumferentially in small amount (6 mm posterior to the left ventricle and 9 mm lateral to the right ventricle) (Figure 2). We point out the progression of the LV systolic dysfunction compared to the previous evaluation performed 3 months prior, when LVEF was 40%.

Figure 2. Transthoracic echocardiography, color Doppler examination. The parasternal sections on the long axis (a) and apical 4 chambers (B). Dilation of the Left Ventricle (LV) is observed (48 mm in systole) , dilation of the Left Atrium (LA) (44/56 mm) and the presence of a severe mitral regurgitation with eccentric jet oriented to the postero-lateral wall of LA (white arrow). In the pericardium, small amount of liquid (black arrow). LA, left atrium; LV, left ventricle; RV, right ventricle; RA, right atrium; Ao, ascending aorta.
To exclude a possible ischemic etiology of the LV dysfunction and for objectivation of the vascular lesions we considered necessary to assess it by coronary angiography associated with aortography. After repeated unsuccessful attempts of cannulation of the right coronary artery, on injection of the left coronary artery we observed that the patient has a coronary anomaly of the type of unique coronary artery, with the origin in the ramus corresponding to the right coronary artery at the level of the anterior interventricular artery in segment 2 (Figure 3).
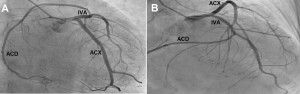
Figure 3. Coronary angiography. A. The incidence of caudal RAO. The incidence of cranial PA. The right coronary artery (RCA) originates in the second segment of the anterior interventricular artery (AIA). The circumflex artery (CXA) is free.
Injection into the right brachiocephalic trunk revealed a tight stenosis in the proximal segment of the right subclavian artery (Figure 4). Aortography revealed an infrarenal aorta with a low transverse diameter, with occlusion of the terminal aorta and refilling of the bilateral common iliac arteries through a highly developed collateral circulation, predominantly originating in the lumbar arteries and inferior mesenteric artery (Figure 5). After analyzing the data, it was considered that the most plausible etiology for these vascular lesions remains the atherosclerotic vascular substrate associated with the presence of favorable local conditions, such as the history of radiotherapy at the level of the right chest and the imaging features of hypoplastic aortoiliac syndrome.

Figure 4. Angiography of brachicephalic trunk. It reveals the presence of proximal tight stenosis of the right subclavian artery (arrow). RSA, right subclavian artery; VA, right vertebral artery; CAA, right common carotid artery.
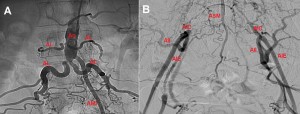
Figure 5. Angiography of terminal aorta. The terminal aorta is occluded, the common iliac arteries (CIA) are distal refilled bilaterally, the external iliac arteries (EIA) and internal iliac arteries (IIA) by collaterals developed from the lumbar arteries (LA), inferior mesenteric artery (IMA) and anterior sacral artery (ASA).
It is believed that the patient is suffering from a toxic biventricular cardiomyopathy secondary to the chemotherapy with Epirubicin, a preparation belonging to the anthracycline class. The other substances used, cyclophosphamide and 5-Fluorocuracil, although they were administered in large total dosses, are more frequently associated with acute cardiotoxic effects that usually stop after a relatively short time after administration of the drugs1-3.
With regard to the therapeutic approach, the European guide on Perioperative Cardiological Evaluation in Non-Cardiac Surgery recommends for patients with unstable heart disease the adoption of a multidisciplinary approach. In this case, after consulting the surgeon and anesthetist it was decided that the surgical risks are unacceptable in the context of severe LV dysfunction and severe mitral regurgitation.
For the vascular lesions, in the absence of acute or critical chronic ischemia, we opted for a conservative therapy focused on exercise and pharmacotherapy with statins, antiaggregant and peripheral vasodilator. A possible surgical revascularization might be associated with an unfavorable risk/benefit ratio, given the fact that the patient’s clinical condition was relatively stationary in the absence of specific treatment.
Particularities of this case consist in the presence of a wide spectrum of cardiotoxic manifestations of anticancer treatment, the possible combination of two vascular congenital malformations in different territories (coronary, respectively aortoiliac) and the discrepancy between the severe vascular damage and the paucisymptomatic state of the patient.
Discussion
According to the data published by WHO, cardiovascular and neoplastic diseases are the top two causes of death in Europe, being responsible together for about 70% of all deaths4. Frequent association of these two major groups of diseases caused the emergence of a new interdisciplinary field that can be defined as cardio-oncology.
Their frequent coexistence is due to their high prevalence, the sharing of common risk factors and especially to the cardiotoxic effects associated with chemotherapy and radiotherapy.
The most common form of cardiotoxicity in patients who have received anti-cancer treatment is the anthracycline-induced cardiomyopathy. Patients treated with anthracyclines have a 5 times higher risk of developing heart failure compared to patients treated with other classes of anti-cancer drugs5. Anthracycline-induced cardiomyopathy is classified based on the time of onset in the acute form, a chronic form of early-onset and late-onset chronic form. The acute form is relatively rare, it occurs in <1% of patients in the first 2 weeks after administration of treatment, it is reversible, dose-independent and it can manifest itself by the occurrence of coronary syndromes, arrhythmias, pericarditis or a transient diffuse contractile dysfunction6-9.
The early-onset chronic form occurs during the first year after treatment, with a peak incidence within the first 3 months, it is characterized by irreversible and progressive impairment of the cardiac function through the destruction of cardiomyocytes by oxygen free radicals released at myocardial level following the action of anthracyclines. The late-onset chronic form occurs through a similar mechanism, affecting up to 5% of patients and it may begin even 30 years after completing the anthracycline therapy6-9.
In the previously presented patient we find the characteristics of early-onset chronic cardiotoxicity, to the occurrence of which several favoring factors contributed, such as: the association with radiotherapy or cyclophosphamide and an increased total dose of epirubicin.
Radiotherapy generates fibrotic changes on most cardiac structures entering in the field of radiation, including: pericardium, myocardium, valves, coronary arteries and conduction system10,11. Pericarditis is the typical form of expression, which usually accumulates too slowly to produce cardiac tamponade, but in time it may progress to the constrictive form even without a history of effusion. Radiotherapy-induced cardiomyopathy is different from that produced by anthracyclines by predominantly affecting the diastolic function. Valvular damage is characterized by thickening, fibrosis and calcification of cusps or chordae, the aortic valve being more frequently incriminated10-12.
The patient associated a coronary anomaly of the type of single coronary artery, a rare cardiac malformation with an incidence of 0.008-0.067% in large angiographic registries13-15. It is considered a benign anomaly, which has not been shown to have a favoring effect on atherosclerosis. The origin of the right coronary artery in the anterior interventricular antery is a rare version, J. Wilson et al. quantifying only 36 similar cases in the literature in an analysis conducted in 200915.
Two substrates were discusses as etiology for the vascular lesions diagnoses angiographically: atherosclerosis or arteritis of large vessels. The classical risk factors pleaded for atherosclerosis, such as the smoking history and the presence of chronic kidney disease. In addition, some authors in the literature allege that tumors, through their ability to release proinflammatory cytokines in circulation, favor the development of atherosclerosis. This hypothesis is supported by clinical studies that have identified an increased calcium score and a significantly higher intima-media ratio in patients with breast cancer16,17. Moreover, chemotherapy was associated with a significant worsening of lipid profile and increase of the intima/media ratio in a recent study18. A few favorable local conditions were added to these factors of systemic action. For example, the right thoracic radiotherapy history played most likely an important contribution to the emergence of the proximal tight stenosis of the right subclavian artery. Furthermore, we found in this patient’s case multiple characteristics of the aortoiliac hypoplasia syndrome. This syndrome is described in approximately 10% of patients revascularized surgically or interventionally for aortoiliac occlusive disease, the majority being of feminine gender, smokers and non-diabetic19,20. It is defined by the existence of a low sized infrarenal aorta, with a transverse diameter under 1 cm above the terminal bifurcation21. This narrow diameter leads to the occurrence of a turbulent local blood flow and creates hemodynamic conditions favorable to the development of atherosclerosis at this level.
Within the framework of the differential diagnosis algorithm, we evaluated the possible existence of an arteritis of large vessels, the Takayashu disease being a plausible option. Excluding this version was performed after obtaining an insufficient number of points on checking the Sharma diagnostic criteria, which have a sensitivity above 95% in establishing the diagnosis of Takayashu disease22.
We consider the patient’s ability to develop a collateral circulation as being impressive; it enabled her to overcome the terminal aortic occlusion event without any clinical progress at any given moment, to a Fontaine class more severe than grade II. It is possible that the neoplastic field of the patient may have contributed to this situation to some extent, if we consider the ability of tumors to secrete angiogenic factors involved in tumor growth, factors which, in this case, might have acted remotely stimulating the development of collateral circulation.
Conclusions
Cardiotoxic effects of chemotherapy and radiotherapy may limit the quality of life and survival of cancer patients. Regular follow-up of patients may ensure early diagnosis and rapid initiation of cardiovascular treatment, thus having a significant impact on prognosis. The progresses achieved in anticancer therapy led, by prolonging survival, to an increase expression of cardiotoxic effects that may have latency periods of decades.
Conflict of interest: none declared.
References
1. Chanan-Khan A et al, Prevention and management of cardiotoxicity from antineoplastic therapyJ Support Oncol. 2004 May-Jun;2(3):251-6
2. Schimmel K, et al. Cardiotoxicity of cytotoxic drugsCancer Treat Rev. 2004 Apr;30(2):181-91
3. Poldermans D, et al. Guidelines for pre-operative cardiac riskassessment and perioperative cardiacmanagement in non-cardiac surgery. European Heart Journal 2009; 30:2769-2812
4. The European health report 2012: charting the way to well-being, WHO Regional Office for Europe, http://www.euro.who.int/__data/assets/pdf_file/0004/197113/EHR2012-Eng.pdf
5. Smith L, et al. Cardiotoxicity of anthracycline agents for the treatment of cancer: systematic review and meta-analysis of randomised controlled trials.BMC Cancer. 2010 Jun 29;10:337.
6. Ades F, et al., Cardiotoxicity of systemic agents used in breast cancer, The Breast (2014)1-12
7. Adão R, et al.Cardiotoxicity associatedwithcancertherapy:Pathophysiologyand prevention.RevPortCardiol.2013;32(5):395—409
8. Berardi R, et al. State of the art for cardiotoxicity due to chemotherapy and to targetedtherapies: A literature review. Critical Reviews in Oncology/Hematology 88 (2013)75–86
9. Todaro M, et al. Cardioncology: State of the heart. International Journal of Cardiology 168 (2013) 680–687
10. Carver J, et al. American Society of Clinical Oncology Clinical EvidenceReview on the Ongoing Care of Adult Cancer Survivors:Cardiac and Pulmonary Late EffectsJ Clin Oncol 25:3991-4008
11. Vasiliadis I, et al. Cardiotoxicity and Cancer Therapy Angiology2014, Vol. 65(5) 369-371
12. Lee M, et al. Cardiovascular Complications of Radiotherapy. Am J Cardiol 2013;112:1688e1696
13. Yamanaka O, Hobbs R. Coronary artery anomalies in 126,595 patients undergoingcoronary arteriography. Cathet Cardiovasc Diagn 1990;21:28–40
14. DesmetW, Vanhaecke J, Vrolix M, et al. Isolated single coronary artery: a review of50,000 consecutive coronary angiographies. Eur Heart J 1992;13:1637–40
15. Wilson J, et al. Anomalous right coronary artery originating from the left anterior descending artery:Case report and review of the literature.International Journal of Cardiology 137 (2009) 195–198
16. Mast M, et al. Preradiotherapy calcium scores of the coronary arteries in a cohort of women with early-stage breast cancer: a comparison with a cohort of healthy women. Int J Radiat Oncol Biol Phys. 2012 Jul 1;83(3):853-8
17. Melichar B, et al. Carotid intima-media thickness and laboratory parameters of atherosclerosis risk in patients with breast cancer. Anticancer Res. 2012 Sep;32(9):4077-84
18. Kalabova H, et al. Intima-media thickness, myocardial perfusion and laboratory risk factors of atherosclerosis in patients with breast cancer treated with anthracycline-based chemotherapy.Med Oncol. 2011 Dec;28(4):1281-7
19. DeLaurentis D et al. Atherosclerosis and the hypoplastic aortoiliac system. Surgery. 1978 Jan;83(1):27-37.
20. Walton B, et al. Percutaneous intervention for the treatment of hypoplastic aortoiliac syndrome.Catheter Cardiovasc Interv. 2003 Nov; 60(3):329-34.
21. Cronenwett J, et al. Aortoiliac occlusive disease in women.Surgery. 1980 Dec;88(6):775-84.
22. Sharma B, et al. Diagnostic criteria for Takayasu arteritis.Int J Cardiol. 1996 Aug; 54 Suppl:S141-7.
 This work is licensed under a
This work is licensed under a