Catalin Usurelu1, Elvis Botu1, Daniel Blajan1
1 Department of Cardiology, Arges Emergency County Hospital, Romania
Abstract: Acute coronary syndromes comprise of a wide range of clinical presentations and various electrocardiographic patterns. Some of these electrocardiographic patterns define a subset of patients with extensive or proximal coronary artery disease and as such with a worse outcome. Early recognition of these patterns may change the course of therapy and require a faster invasive approach.
Keywords: acute coronary syndrome, anterior descending artery, de Winter
INTRODUCTION
Introduction of coronary angiography in common cardiology practice allowed the right correlation of the electrocardiographic appearance and anatomical localization of lesions, thus making possible the description of new electrocardiographic patterns in the wide spectrum of acute coronary syndromes.
CASE REPORT
We describe the case of a 46-year-old smoker male patient, with dyslipidemia, without prior cardiovascu-lar history who came to the emergency department for an ongoing thoracic pain with typical characters of angina at four hours from debut. The initial examination showed a hemodynamically stable patient with a blood pressure of 135/80 mmHg and a pulse of 78 bpm; the electrocardiogram shows sinus rhythm with 1 mm ST depression in leads V2-V5 (Figure 1). Myocardial necrosis markers were in normal range.
The echocardiographic evaluation shows a modera-te left ventricular dysfunction with an estimated global ejection fraction of 45% because of hypokinesia of the apex, the interventricular septum and the lateral wall in their apical third; we excluded an aortic dissection, there was no pericardial fluid and the estimated pulmonary pressures were in normal range.
The patient is transferred in the monitoring area and therapy with dual antiplatelet, statin and nitrate are started with prompt relieve of angina. Two hours after the initial episode the angina reappears, and the electrocardiogram shows 2 mm ST depression in leads V1-V6 associated with positive symmetric T waves and 1 mm ST elevation in lead aVR (Figure 2).
We decided emergency coronary angiography showing acute thrombotic occlusion of the left anterior descendent artery in the mid segment and non-significant plaques in the right and circumflex arteries (Figure 3). We performed emergency angioplasty of the left anterior descendent artery with initial thrombus aspiration and stent implantation with a final TIMI 3 distal flow. The evolution of the electrocardiogram afterwards shows negative T waves in leads V1-V5 (a common aspect in the evolution of an acute myocardial infarction patients) (Figure 4).
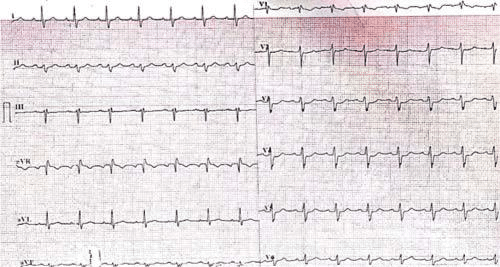
Figure 1. ECG: sinus rhythm with 1 mm ST depression in leads V2-V5.
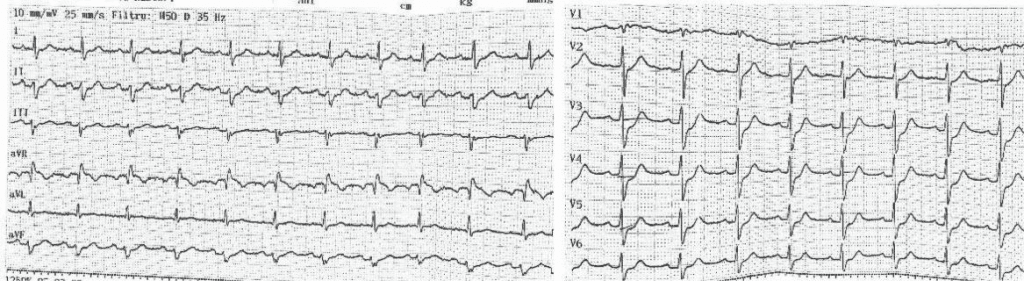
Figure 2. ECG shows 2 mm ST depression in leads V1-V6 associated with positive symmetric T waves and 1 mm ST elevation in lead aVR.
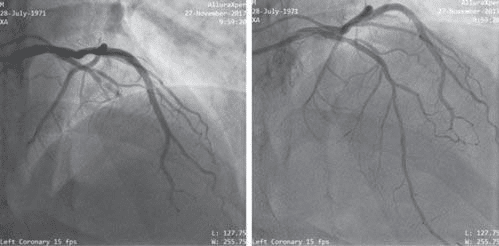
Figure 3. Coronary angiography: acute thrombotic occlusion of the left anterior descendent artery in the mid segment and non-significant plaques in the right and circumflex arteries.
DISCUSSION
The particularity of this case is the electrocardiographic aspect during angina, with ST depression and positive T waves in the leads corresponding to the territory of the left anterior descendent artery, later correlated with the angiographic findings.
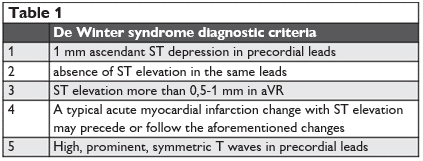
This electrocardiographic aspect can be considered as an intermediate between the usual changes we see in left anterior descendent subocclusion (ST slight elevation and T wave inversion in leads V2-V3 with aVR ST elevation – also described as the Wellens syndrome) and the changes that characterize acute left anterior descendent occlusion (hyper acute T waves in the anterior leads) and has been described in the literature as the De Winter syndrome1,2. The electrocardiographic evolution respects the diagnostic criteria of the De Winter syndrome, characterized by post infarction T wave inversion. It is important to mention that this aspect may precede or follow the typical changes that appear in myocardial infarction (ST elevation).
Thus, we want to underline the importance of this rare clinico-electrocardiographic syndrome first described in the literature by De Winter in 2008 (Table 1). We can see this electrocardiographic change in about 2% of the patients with acute left anterior descendent occlusion and some authors proposed this pattern as an equivalent of anterior ST elevation acute myocardial infarction. Thus it is of paramount importance the rapid recognition of these cases that require urgent coronary angiography and reperfusi-on therapy (some authors advocating even a role for thrombolysis in this cases when rapid reperfusion via angioplasty cannot be achieved in a timely manner). Along with ST elevation in the precordial leads and the Wellens syndrome (another named syndrome associated with critical lesion of the left anterior descendent)3 these electrocardiographic changes in the presence of angina are to be considered cardiological emergencies and treated as such.
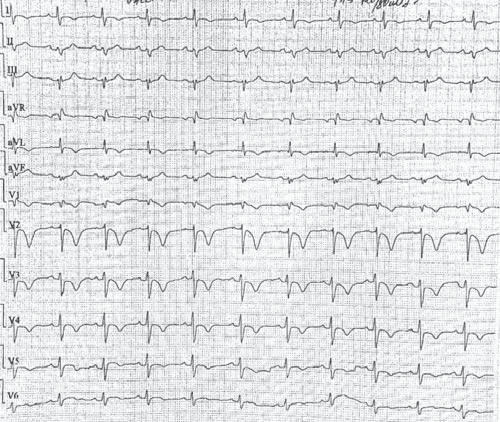
Figure 4. ECG afterwards shows negative T waves in leads V1-V5.
CONCLUSIONS
The de Winter syndrome is a rare electrocardiographic pattern that defines a particular high-risk group of acute coronary syndrome patients for whom early invasive assessment and prompt revascularization is the first therapeutic option and may even be lifesaving.
Conflict of interest: none declared.
Reference
1. Chioncel V, Avram A, Ion AC, Sinescu C. The de Winter T waves – an unusual presentation of left anterior descending artery occlusion. Rom J Card 26, 3, 2016.
2. De Winter R, Verouden N, Wellens H, Wilde A. A new ECG sign of proximal LAD occlusion. N Engl J Med 2008;359:2071–3.
3. Smith WS. de Winter’s T-waves evolve into Wellens’ waves. http:// hqmeded-ecg.blogspot.ro/2017/06/de-winters-t-waves-evolve-into-wellens.html.
 This work is licensed under a
This work is licensed under a