Raluca G. Saru1,3, Philippine Kies2, Lucia J.M. Kroft3
Article received on the 10st of August 2012. Article accepted on the 27th of August 2012.
1 Emergency University Hospital Bucharest, Department of Radiology, Romania
2 Leiden University Medical Centre, Department of Cardiology, the Netherlands
3 Leiden University Medical Centre, Department of Radiology, the Netherlands
Emergency University Hospital, Radiology Department. 169, Splaiul Independentei. 050098 Bucharest, Romania
E-mail: raluca.saru@gmail.com
Abstract: We report a case of a 54-year-old male known with coronary fistula. Previous invasive coronary angiography had not been conclusive regarding the relationship with surrounding structures. Coronary computed tomography angiography (CTA) was performed with prospective ECG-triggering and volumetric single heart beat acquisition on a 320-slice multidetector computed tomography scanner (Toshiba Aquilion ONE). During acquisition, the heart rate was below 60 beats per minute. The effective dose absorbed by the patient for the coronary CTA was approximately 3mSv. Coronary CTA visualized the fistula with its surrounding structures. Origin of the fistula was from the left anterior descending artery with insertion into the pulmonary artery. CTA played a role in delineating the anatomy of the fistula and its relationship to the adjacent structures.This case is to demonstrate that coronary CTA provides excellent visualization of the three-dimensional anatomy that can be advantageous in evaluating small morphologic structures such as coronary artery fistula.
Keywords: coronary fistula, computed tomography, coronary CT angiography
CASE STUDY
We report a case of a 54-year-old male who was reffered at Leiden University Medical Centre.
The patient was discovered with a holosystolic murmur in 1976, with high frequency and maximum intensity in the second intercostal space, that was supposed to be due to an open ductus Botalli. At invasive angiography a small fistula from left anterior descending artery (LAD) was found. The patient was routinely reevaluated in 2006 via catheterization. At invasive angiography the fistula was found but the relationships with the surrounding structures were unclear, suggesting a relationship with the left atrium (Figure 1); because the fistula was small it was no further treated.

Figure 1. Right anterior oblique projection coronary angiography shows the fistula arising from LAD.
In September 2011 he was reffered for diagnostic evaluation of aspecific noctermal palpitations at rest.
Physical examination and the electrocardiogram (ECG)
were normal. Echocardiography showed normal left ventricular dimensions and function normal and right ventricular dimensions at upper border with normal function, stable since 1999. The holter – ECG showed early atrial beats and isolated premature ventricular contractions.
Coronary computed tomography angiography (CTA) was performed for fistula evaluation. The images were acquired with a 320-slice multidetector computed tomography (MDCT) scanner Aquilion ONE, (Toshiba Medical Systems, Otawara, Japan) with prospectively ECG – triggered, axial volumetric data acquisition. The patient was administered intravenously 70 ml of iodinated contrast agent at a rate of 6 ml s−1, followed by 20 ml of mixture saline and contrast (1:1) at a rate of 6 ml s−1 and then by 30 ml saline at the rate of 3 ml s−1.The bolus tracking sensor was positioned in the left ventricle and the acquisition started when the signal in the left ventricle reached a predefined threshold of 180 Hounsfield units (HU). The volumetric acquisition was achieved prospectively, ECG-gated, in a single gantry rotation within a fraction of a heart beat. The scanning parameters were: gantry rotation time 350 ms, detector collimation 0.5×320 mm, tube voltage 100 kV, tube current 560 mA.
One hour before the scanning he had been administered 25 mg of betablocer orally to reduce and stabilize the heart rate. During scanning the heart rate less was than 60 beats per minute. The dose length product (DLP) for the coronary CTA was 219 mGy×cm equivalent with the effective dose absorbed by the patient of approximately 3 mSv, by using the conversion factor k = 0,014. Data were prospectively reconstructed at 70 – 80% of the cardiac R-R cycle with a slice thickness of 0.5 mm. For reconstruction we used FC-03 kernel and noise reductions tools: BOOST 3D for raw data and quantum denoising software + (QDS+) for image data.
Images were analysed on a dedicated workstation Vitrea Fx. The fistula from LAD to pulmonary artery was well visualised. (Figures 2, 3, 4).
Because the fistula had no significant hemodynamic consequence and the complains disepeared three weeks after the admission, the decision was not to treat it.
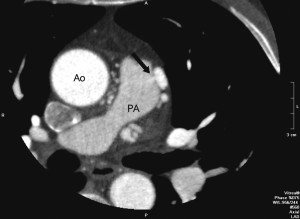
Figure 2. Coronary CTA. Cross-sectional image. Arrow points at fistula communication between to the pulmonary artery.
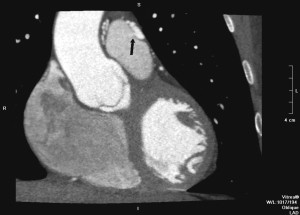
Figure 3. CT coronary angiography. Reconstructed coronal image. Arrow indicate fistula communication between LAD and the pulmonary artery. Note the fistula surrounding the pulmonary artery (PA). Ao, aorta.

Figure 4. CT coronary angiography. Three-dimensional reconstructed image. Arrows indicate fistula communication between LAD and the pulmonary artery.
Discussions
This case demonstrates that coronary – CTA provides excellent three dimensional visualization of the coronary anatomy that can be advantageous in evaluating small structures such as coronary artery anomalies e.g. coronary arteries fistula (CAF).
CAF account for 0,08 to 0,4% of all congenital heart diseases1. CAF are communications between the coronary arteries and a cardiac chamber or a thoracic vessel. If they are small, the usually do not cause symptoms. If size reaches three times the size of the normal caliber of the coronary artery, it may cause coronary artery steal phenomenon, which may lead to ischemia of the segment of the myocardium perfused by the coronary artery2. Congenital CAF, are thought to arise as a result of incomplete embryonic development; normally the coronary arteries communicate with the great vessels and chambers of the heart via sinusoids and during development these sinusoids transform into a normally calibrated capillary network. It has been postulated that incomplete closure of these sinusoids can result in CAF3. Prevalent clinical presentations of CAF are dyspnea and angina pectoris4.
This case is to demonstrate that MDCT provides excellent visualization of the three-dimensional anatomy that can be advantageous in evaluating small morphologic structures such as coronary artery fistula.
Acknowledgement: The authors would like to thank Joost Roelofs – specialized CT technician at LUMC, for supplying technical information about the scanning procedure.
Conflict of interest: none declared.
Bibliography
1. De Doelder MS, Hillers JA. Combination of imaging modalities in a coronary artery fistula. Netherlands Heart Journal. 2008 Sep; 16(9): 313-4.
2. Gupta M. Coronary artery fistula. Available from: URL: http://emedicine.medscape.com/article/895749-overview
3. Early SA, Meany TB, Fenlon HM, Hurley J. Coronary artery fistula; coronary computed topography – The diagnostic modality of choice. Journal of Cardiothoracic Surgery. 2008 Jul 5;3:41.
4. Salah AM Said, Current characteristics of congenital coronary artery fistulas in adults: A decade of global experience; World Journal of Cardiology 2011 Aug26; 3(8): 267-277.
 This work is licensed under a
This work is licensed under a