Carmen Ginghina1,2, Monica Chivulescu1, Andreea Calin1,2, Gabriela Raileanu1, Eduard Apetrei1,2
1 “Prof. Dr. C. C. Iliescu” Emergency Institute of Cardiovascular Diseases, Bucharest, Romania
2 “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania
Abstract & aims: Although mortality is the most important clinical endpoint in heart failure (HF) clinical trials, it is now recognized that preventing HF hospitalization is important for patients and healthcare systems. In the Digitalis Investigation Group (DIG) trial, digoxin reduced hospitalization due to heart failure (HF) and improved outcomes in highrisk subgroups of HF patients. In our study, we investigated the contemporary use of digoxin in clinical practice based on current knowledge. Methods and results – We retrospectively studied the medical files of 300 patients (58% men, 65±12 years) admitted for both systolic and diastolic HF of different etiologies, in NYHA functional class IIIV. Having in mind the original design of the DIG trial and the recommendations of the current guidelines, we focused on the subgroup of patients with heart failure and reduced left ventricular ejection fraction (LVEF) (REFHF) (LVEF less than 45%) in sinus rhythm. Only 26 patients (31.7% of patients in this subgroup) received digoxin. On the other hand, in the subgroup of patients with atrial fibrillation 89 patients (60.13% of patients in this subgroup) were treated with digoxin. A higher heart rate at admission and a lower LVEF were predictors of digoxin choice in atrila fibrillation subgroup. Comparing patients treated with digoxin to nondigoxin patients, we concluded that the more severe the HF (in terms of clinical, biological and echocardiographic parameters), the more likely will be for the patient to receive digoxin. Markers of severity were advanced functional NYHA class, clinical signs of elevated LV filling pressures, tachycardia, lower sodium levels and depressed LV function as assessed by LVEF. Conclusion – This study highlighted the fact that in current clinical practice digoxin is a therapy of last resort and this drug is chosen in patients with more advanced HF.
Keywords: digoxin, heart failure, atrial fibrillation, ejection fraction
Scopul lucrării: Deşi mortalitatea este obiectivul primar în studiile clinice de insuficienţă cardiacă (IC), este recunoscut faptul că prevenirea spitalizărilor pentru IC este la fel de importantă pentru pacienţi şi pentru sistemele de sănătate. În studiul DIG (Digitalis Investigation Group), digoxinul a redus spitalizările pentru IC şi a îmbunătăţit prognosticul la pacienţii cu IC cu risc crescut. În studiul nostru, am investigat folosirea contemporană a digoxinului în practica clinică bazată pe nivelul actual de cunoaştere. Material şi metodă: Am studiat retrospectiv dosarele a 300 de pacienţi (58% bărbaţi, 65±12 ani) internaţi pentru IC sistolică sau diastolică de diferite etiologii, în clasa funcţională NYHA IIIV. Rezultate: Având în vedere designul original al studiului DIG şi recomandările ghidurilor actuale, ne-am focalizat pe subgrupul de pacienţi cu IC şi fracţie de ejecţie a ventriculului stâng (FEVS) redusă (FEVS sub 45%) în ritm sinusal. Doar 26 de pacienţi (31,7% din acest subgrup) au primit digoxin. Pe de altă parte, în subgrupul de pacienţi cu fibrilaţie atrială, 89 de pacienţi (61,13% din acest subgrup) au fost trataţi cu digoxin. O frecvenţă cardiacă mai rapidă şi o fracţie de ejecţie mai mică la internare au fost predictori pentru instituirea tratamentului cu digoxin la pacienţii cu fibrilaţie atrială. Comparând pacienţii aflaţi pe digoxin cu cei fără tratament cu digoxin, am concluzionat că probabilitatea de a primi tratament cu digoxin creşte o dată cu creşterea severităţii tabloului de insuficienţă cardiacă (din punct de vedere clinic, biologic şi ecocardiografic). Markerii de severitate au fost clasa funcţională NYHA mai avansată, semnele clinice de presiuni de umplere ale ventriculului stâng (VS) crescute, tahicardia, nivelele reduse ale sodiului seric şi disfuncţia VS. Concluzie: Acest studiu arată că, în practica clinică actuală, digoxinul este o terapie de ultimă linie şi că acest medicament este utilizat la pacienţii cu forme avansate de IC.
Cuvinte cheie: digoxin, insuficienţă cardiacă, fibrilaţie atrială, fracţie de ejecţie
INTRODUCTION
Two decades have passed since the publication of DIG (Digitalis Investigation Group) trial, the largest rando mized clinical trial (RCT) of digoxin efficacy in heart failure (HF). Over recent years, digoxin has not been seen as a valuable treatment for patients with heart failure because it did not prove a reduction in morta lity1,2. Guidelines of HF recommend digoxin as a last resort treatment which may be considered for symp tomatic patients with systolic HF in sinus rhythm on top of all the other recommended drugs (betablocker, angiotensinconvertingenzyme (ACE) inhibitor or an giotensin receptor blocker (ARB) and a mineralocorti coid receptor antagonist (MRA) or ARB, ivabradine) in order to reduce hospitalisations for HF35. In patients with atrial fibrillation and HF, digoxin may be useful, but betablockers are still the first line treatment in reduced ejection fraction HF (REFHF) and a rateli miting calcium channel blocker (CCB) is considered before digoxin in preserved ejection fraction HF (PEF HF). This leaves digoxin as an option only for patients whose ventricular rate is not controlled with a beta blocker or a CCB alone4,5. The gap in evidence comes from the fact that digoxin has not been studied in con junction with a betablocker and ivabradine, the two other drug classes that are recommended for heart rate reduction in HF. The DIG trial, PROVED (Prospective Randomized Study of Ventricular Function and Efficacy of Digoxin) trial and RADIACE (Randomized Assessment of Digoxin on Inhibitors of the Angiotensin Converting Enzyme) trial concluded that hospitalizations for and exacerbation of systolic HF in sinus rhythm were significantly reduced with digoxin treatment when added to a diuretic and ACE inhibitor1. The aim of our study was to assess the contemporary use of digoxin in clinical practice in patients with HF of various etiologies, based on current knowledge, in a tertiary center of cardiology.
METHODS
Study design
We conducted a retrospective, crosssectional, unicentric study in a tertiary hospital in Bucharest, Romania. We studied the hospital records of 426 patients admitted for HF in one of the four cardiology departments of the Institute between January 2014 and February 2015. We included patients with HF diagnosed according to the European Society of Cardiology (ESC) definition with New York Heart Association class II–IV on admission. Patients who were hospitalized for an acute worsening of chronic HF were included. We excluded patients admitted for acute HF (cardiogenic shock, pulmonary edema) in the presence of an acute coronary syndrome.
Data collection and definitions
Demographic and clinical data were collected for all patients. The major cause of HF was considered to be the cardiovascular disease that first led to the HF syndrome. The diagnosis of ischemic heart disease was made on the basis of the patient’s history of significant coronary artery disease revealed by coronary angiography or on the basis of chest pain in addition to at least one positive non invasive stress test. The diagnosis of valvular heart disease was made on the basis of significant valvular disease defined as moderate or severe left valvular stenosis or regurgitation. Arterial hypertension was considered to be the main cause of HF with preserved ejection fraction in the presence of a history of hypertension associated with ecocardio graphically defined left ventricle hypertrophy and signs of elevated left ventricular filling pressures.
We also paid special attention to comorbidities. Arterial hypertension was defined on the basis of clinical history or by the use of antihypertensive medication at admission. Diabetes was defined by a plasma fasting glucose (FPG) greater than 126 mg/dl, a HbA1c grea ter than 6.5% or the use of glucoselowering agents or insulin. Ischemic or hemorrhagic stroke were certified by a cerebral computed tomography performed previously. Chronic obstructive pulmonary disease (COPD) was defined by abnormal pulmonary function tests or current treatment with an inhaled longacting bron chodilatator and/or an inhaled corticosteroid. Liver dysfunction was defined by elevated transaminases. Chronic kidney disease was defined by a creatinine clearance calculated by MDRD formula lower than 60 ml/min/m2.
Ventricular filling pressures were clinically assessed and the hemodynamic profiles were either pulmonary and/or systemic venous congestion with normal perfusion in decompensated HF or clinically wellcompen sated profile with a previous diagnosis of HF. Heart rate was deducted from the 12 lead ECGs. On the same admission ECG, the presence of sinus rhythm or atrial fibrillation was noted. Blood pressure values were collected from clinical charts. We took into account blood test parameters collected from the first blood test at admission. The only echocardiographic parameter that was registered in all patients was left ventricular ejection fraction, but we also defined left atrium dilatation by a left atrium volume greater than 34 ml/m2, a right atrium dilatation by a right atrium area greater than 18 cm2 and a right ventricle dysfunction by a TAPSE of less than 1.6 cm in patients in whom these data was also available.
Statistical analysis
Statistical analysis was performed using Stata Software for Windows 12. Univariate analysis comparison of the patients characteristics was performed using chisqua re-test for discrete variables and Student`s test for continuous variables. A P <0.05 was considered statistically significant all hypothesis tests were two sided
RESULTS
After we reviewed a number of 426 patient records, we excluded patients admitted for acute HF (cardi ogenic shock, pulmonary edema) in the presence of an acute coronary syndrome and we included in this study 300 patients hospitalized with chronic or chronic decompensated heart failure.
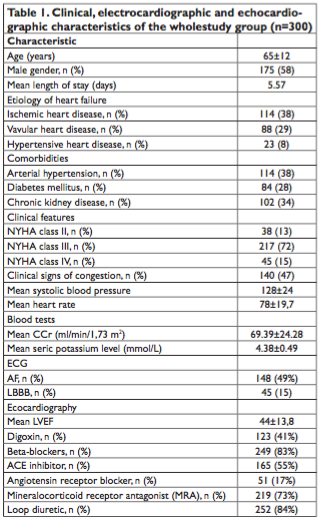
Clinical, electrocardiographic and echocardiographic characteristics of the patients included in the study are presented in Table 1. Among the 300 patients included in the study, 175 (58.33%) were men and the mean age was 65.16+/ 12.75 years. Mean hospital stay was 5.57 days. The main cause of HF was ischemic heart disease in 114 (38%) patients, valvular heart disease in 88 (29%) patients and hypertensive heart disease in 23 (7.6%) patients. Arterial hypertension, chronic kidney disease and diabetes were important comorbidities. One third (28%) of pa tients had diabetes, 34% had chronic kidney disease and 38% were hypertensive. Most of the patients had severe HF, either New York Heart Association (NYHA) class III (72.3%) or NYHA IV (15%). Almost half of the patients had signs of pulmonary and/or systemic congestion at admission (46.7%). Mean systolic blood pressure was 128 mmHg and mean heart rate was 78 beats per minute. Half of the patients (50.7%) were in sinus rhythm and had no history of atrial fibrillation and the other half (49.3%) had either permanent, long standing persistent, persistent or paroxysmal atrial fibrillation. In addition, 15% of patients had a QRS morphology of left bundle branch block (LBBB) on the ECG. Mean left ventricle ejection fraction was 44%. Regarding phar macological treatment, 41% of all patients received di goxin. The majority of patients received betablocker (83%) and loop diuretic (84%) treatment. More than half (55%) received an ACE inhibitor and 17% were treated with an angiotensine receptor blocker (ARB). 73% of patients were prescribed a mineralocorticoid receptor antagonist (MRA) (Table 1).
In this study we first compared the group of patients taking digoxin with the group of patients not taking digoxin (Table 2). We noticed important features regarding digoxin use in clinical practice. There was a significant association between a severe clinical syndrome of HF and digoxin treatment: 57% of patients in NYHA IV received digoxin, 38% of patients in NYHA III recei ved digoxin and an even smaller percent of patients in NYHA II were treated with digoxin (Figure 1).
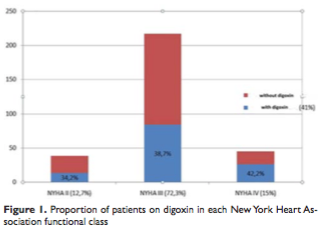
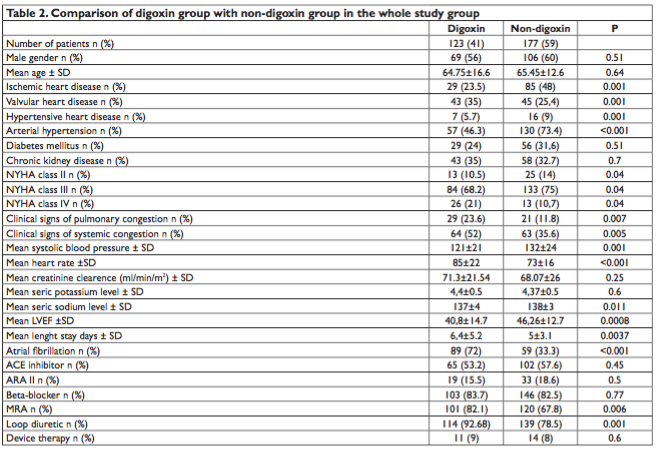
Most of the patients treated with digoxin were in NYHA III functional class because this group was the most representative in our study population. Patients treated with digoxin were more frequently admitted for worsening HF and needed more frequently treatment for their congestion (loop diuretic or/and mineralo corticoid receptor antagonist). Systolic and diastolic hypotension and rapid ventricular rate were more frequently associated with the use of digoxin. Absence of ischemic heart disease and presence of valvular heart disease were predictors for digoxin use. Patients with atrial fibrillation and more severely dilation of left and right atrium were more frequently treated with digoxin. The mean left ventricular ejection fraction and TAPSE were lower and the mean length stay was lon ger in patients treated with digoxin.
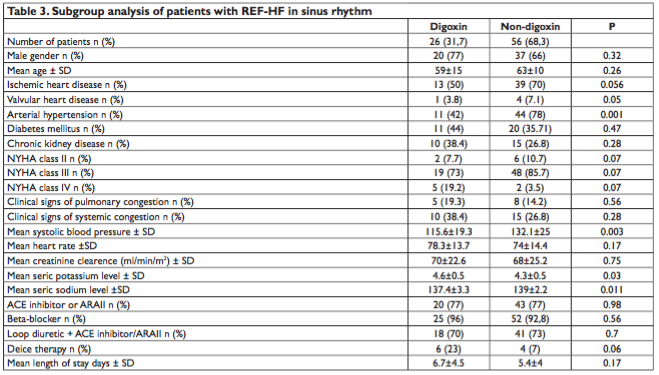
We focused on the subgroup of patients with reduced ejection fraction HF (REFHF) in sinus rhythm (Table 3). We considered REFHF to be defined by a left ventricular ejection fraction of 45% or less. Digoxin was given to only 26 patients (31.7%) of the 82 patients that were included in this subgroup analysis. When we compared the digoxin group with nondigoxin group, we didn’t see any significant differences regarding gender, age, or the presence of chronic kidney disease or diabetes. Patients treated with digoxin were less frequently hypertensive than patients in the nondigoxin group (P=0.001).The clinical features,heart rate, BNP (brain natriuretic peptide) levels, cre atinine clearance, the choice of other pharmacological agents and mean length of stay were similar between groups. The only significant difference between digoxin and non digoxin groups were systolic blood pressure at admission patients in the digoxin group had significantly lower values (115.6 vs 132.1) (P=0.038; P=0.011), seric potassium level which was more elevated in the digoxin group (4.6 vs 4.33) (P=0.03) and seric sodium level which was significantly lower in the digoxin group compared with the nondigoxin group (137.4 vs 139) (P=0.011).
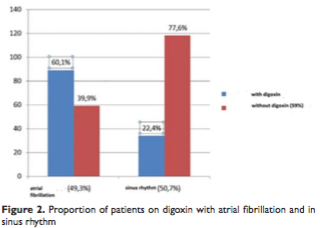
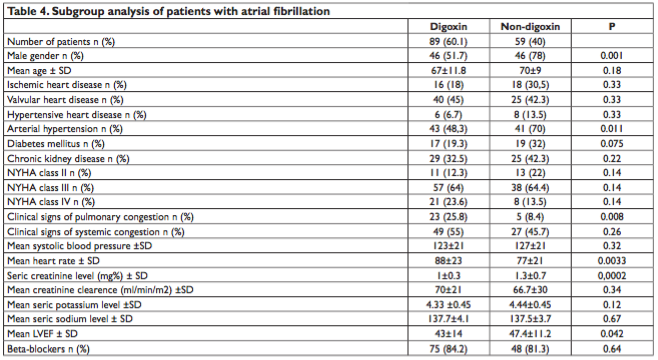
Conversely, when we analyzed the subgroup of patients with atrial fibrillation (Table 4) (148 patients) most of these patients were treated with digoxin (60%) (Figure 2). We compared the characteristics of digoxin patients with the nondigoxin patients in atrial fibrillation group. The two subgroups were very similar regarding age, severity of HF, presence of chronic kidney disease or diabetes, blood pressure values, BNP levels and seric potassium and sodium levels. The proportion of men was greater than the proportion of women in both groups, but 46 patients in nondigoxin group (78%) were men comparing with only 46 patients in digoxin group (52%) (P=0.001). Patients with atrial fibrillation who were not treated with digoxin were more frequently hypertensive comparing with those treated with digoxin (13.5% vs 6.7%) (P=0.011). Clinical signs of left ventricular elevated filling pressures (25.8% vs 8.4%) (P=0.008), a more rapid heart rate (88±23 vs 77±21) (P=0.0033), a lower seric creatinine level (1±0.3 vs 1.3±0.7) (P=0.0002) and a more severe left ventricular systolic dysfunction (43±14 vs 44.4± 11.2) (P=0.042) were more prevalent in digoxin trea ted patients.
DISCUSSION
In this retrospective study including 300 HF patients admitted to a tertiary cardiology center, we investigated the use of digoxin in current clinical practice. Considering the two main indications of digoxin (ven tricular rate control in atrial fibrillation and reduction of HF hospitalizations in patients with REFHF in sinus rhythm), we observed prescription of digoxin in these two clinical settings and also in the whole group of patients.
The composite morbimortality outcome of cardiovascular death or hospitalization for HF is the most commonly used endpoint in HF trials. Digoxin did not show a reduction in all cause mortality in clinical trials, but HF interventions are unlikely to reduce noncar diovascular death. The primary effect of digoxin was on HF hospitalization without any significant effect on cardiovascular death2. Consequently, digoxin is likely to modify HF hospitalization, an important prognostic factor. Although patients present with systemic or pulmonary “clinical congestion”, defined as rales, ele vated jugular venous pressure, and edema, this state is often preceded or followed after initial therapy by “hemodynamic congestion”, defined as high LV diasto lic pressures without overt clinical signs.
It has been postulated that hemodynamic congestion may contribute to the progression of HF because it may result in wall stress as well as in reninangiotensinaldoste rone system (RAAS) activation. Consistent with this paradigm is the wellestablished clinical observation that each hospitalization for AHF heralds a substantial worsening of the longterm prognosis, an effect that appears additive with recurrent hospitalizations7.
We tried to find out how often digoxin is prescribed in patients that are likely to benefit from it. Of 82 patients with REFHF in sinus rhythm that could have taken digoxin in order to reduce hospitalizations of HF only 26 patients received digoxin while the other 56 patients did not. Only one patient took digoxin instead of a betablocker while the other 25 patients received digoxin together with a betablocker. 52 of non digoxin patients received a betablocker and their heart rate was similar to the heart rate of patients taking both digoxin and a betablocker. Heart rate seemed to be the factor that limited the initiation of digoxin on top of a betablocker, although the mean heart rate of nondigoxin group was 74 beats per minute, above the threshold of 70 beats targeted in HF. Potassium levels were lower in nondigoxin group but still in the normal range. A lower systolic and diastolic blood pressure did not prevent the use of beta blockers in the digoxin group where almost all patients (25 patients) received both drugs (digoxin and a betablocker). Although seric creatinine was greater, creatinine clearance was lower in patients taking digoxin and they were also slightly older, these variables were not significantly di fferent in the two groups (digoxin vs nondigoxin).
Digoxin was more likely to be prescribed in the other clinical scenario, as a ventricular rate control agent in atrial fibrillation. The majority of patients in this study were men (58%) and the proportion of men in atrial fibrillation group was also greater than the proportion of women (62%). In the atrial fibrillation subgroup, the majority of nondigoxin patients were men (77%) which could be explained by the high prevalence of ischemic heart disease in this nondigoxin group, a disease known to be more prevalent in men. Digoxin group showed a more rapid ventricular response at admission which is certainly the reason why many of these patients were prescribed digoxin at dis charge. Creatinine levels were significantly lower in the digoxin group allowing clinicians to include this drug in their prescription. Digoxin was more suitable for lower ejection fraction. In IPRESERVE, the prevalence of AF by ECG in HFPEF patients was similar to patients with HFREF in previous studies. HFPEF patients with AF had a significantly worse outcome than those without AF and this increased risk of fatal and nonfatal CV events was independent of other factors associated with a worse prognosis. One of the gaps in evidence is that it is not yet clear if digoxin changes the outcome of patients with atrial fibrillation associated with both preserved ejection fraction HF and reduced ejection fraction HF9. Although it has long been assumed that the increase in the LVEF with digoxin is due an inotropic action of the drug, the findings that other drugs that lowered ventricular rates improved LVEF (like ivabradine in SHIFT study) raise the possibility that some of digoxin’s effect may be related to heart rate reduction2.
The finding that there was a association between the severity of HF syndrome and the use of digoxin led us to conclude that the more severe the HF syndrome is, the more likely it will be for the patient to receive digoxin. Patients on digoxin had indeed more severely elevated filling pressure assessed both clini cally (pulmonary and/or systemic congestion, need of diuretics) and echocardiographically (dilated atria). As the analysis of the Romanian Heart Failure Registry concluded, 1year mortality is substantially higher in pati ents with acute HF compared to chronic HF patients (22.4% vs 6%). Notably, a proportion of 35.8% of patients with acute HF dies or are rehospitalized during 1year follow up6. Digoxin might be important especially in highrisk subgroups of HF patients defined as NYHA IIIIV, LVEF under 25% because it proved outcome improvement in this setting1. Systolic and diastolic blood pressure were lower in the group that received digoxin, while hypertension was a frequent comorbidity encountered in nondigoxin patients. More rapid heart rates associated with lower blood pressure was a condition that led more frequently to digoxin pre scription. Heart rate is a prognostic factor and a therapeutic target in patients with chronic heart failure. Therefore, digoxin is an important therapeutic tool in heart failure patients8. Atrial fibrillation was definitely associated with digoxin treatment: 72% of patients which received digoxin had atrial fibrillation, while only 33% of nondigoxin patients had atrial fibrillation. Seric levels of sodium were lower in digoxin group proba ble as a marker of a more severe stage of heart failu re. Interestingly, creatinine levels and potassium levels were not different between the two groups (digoxin/ nondigoxin) probably because of the small number of patients with advanced renal disease in the study. Mean left ventricular ejection fraction was lower in patients taking digoxin, again as a marker of prognostic significance in these patients. Length of stay was also longer in patients taking digoxin which suggests that they needed a longer period of hospitalization in or der to resolve the clinical congestion before discharge. Ischemic heart disease was more frequently seen in nondigoxin patients while valvular heart disease was more frequently seen in digoxin group. This is probably related to the concern that myocardial ischemia in itself may cause inhibition of sodium pump, rendering myocardial tissue more sensitive to the arrhythmoge nic effects of digitalis, even at lower seric drug con centrations. This is why digoxin should be used in very low doses or not used at all in patients with acute coronary syndromes or significant ischemia10.
STUDY LIMITATIONS
Our study is limited by its single center nature and its design protocol as it is a crosssectional, retrospective study. We could not establish whether digoxin or any other drug was introduced during the index hospita lization period or if patients were on chronic digoxin therapy. We cannot exclude overlapping of many causes of HF in the same patient. Moreover, in advanced stages of HF, it is difficult to state what the cause which first contributed to the clinical syndrome of HF was. Although HF is related to a primary abnormality in myocardial function, further impairments in myocardial function and progressive hypertrophy, dilatation, or both can occur in the absence of additional direct injury to the heart.
Serum digoxin concentrations were available only for a minority of patients. There is a strong associa tion between serum concentration and the safety of digoxin, but we did not notice any case of digitalis toxicity in our study group.
Some important treatments recommended in po tentially all patients with systolic HF like ivabradine, isosorbide dinitrate/hydralazine and newer treatments like neprilysin/angiotensin receptor inhibitors were not noted in the study because of their infrequent use.
Non surgical device treatment of heart failure with reduced ejection fraction implantable cardioverter defibrillators and cardiac resynchornization therapy was also seldom used and therefore this was not analyzed in our study.
CONCLUSION
In conclusion, in our study population of HF patients treated in a tertiary cardiology clinic, digoxin was ma inly prescribed to control heart rate in patients with atrial fibrillation and to a lesser extent in order to de crease the number of hospitalizations in patients with REFHF in sinus rhythm.
This study highlighted the fact that digoxin is a last resort treatment which is chosen in more severe HF patients. Markers of severity in our study were advan ced functional NYHA class, clinical signs of elevated filling pressures, tachycardia, lower sodium levels and reduced left ventricular ejection fraction.
Although pharmacological and nonpharmacological HF therapy tends to increase over the time, in clinical practice these are still underutilized resources, including digoxin.
Conflict of interest: none declared. References:
1. Gheorghiade M, Patel K, Filippatos G, Anker S D, et al. Effect of oral digoxin in highrisk heart failure patients: a prespecified subgroup analysis of the DIG trial. European Journal of Heart Failure 2013, 15, 551–559
2. Castagno D, Petrie M C, Claggett B, McMurray J. Should we SHIFT our thinking about digoxin? Observations on ivabradine and heart rate reduction in heart failure. European Heart Journal 2012 33, 1137–1141
3. Antman E M. Cardiovascular Therapeutics A Companion to Braunwald’s Heart Disease, 4th Edition. Elsevier Saunders 2013
4. McMurray J J V, Adamopoulos S, Anker S D, et al. Ghidul ESC de diagnostic şi tratament al insuficienţei cardiace acute şi cronice 2012 Grupul de Lucru pentru Diagnosticul şi Tratamentul Insuficienţei Cardiace Acute şi Cronice 2012 al Societăţii Europene de Cardiologie. Elaborat în colaborare cu Asociaţia pentru Insuficienţă Cardiacă (HFA) a ESC. Autori/Membri ai Grupului de Lucru. Romanian Journal of Cardiology Vol. 23, No. 3, 2013
5. Ginghină C. Mic Tratat de Cardiologie. Editura Academiei Române 2010
6. Chioncel O., TatuChiţoiu G, Christodorescu R, Coman I. M., Delea nu D, Vinereanu D, Macarie C, et al. Characteristics of patients with heart failure from Romania enrolled in ESCHF LongTerm (ESC HFLT) Registry. Romanian Journal of Cardiology. Vol. 25, No. 4, 2015
7. Bonow R O, Mann D L ,Zipes D P, Libby P. Braunwalds Heart Disease A Textbook of Cardiovascular Medicine. 9th Edition. Elsevier Saun ders. 2012
8. Dobre D, S. Borer J. S. , Fox K et al. Heart rate: a prognostic factor and therapeutic target in chronic heart failure. The distinct roles of drugs with heart ratelowering properties. European Journal of Heart Fai lure (2014) 16, 76–85
9. Zile M. R., Komajda M., Mckelvie R. et al. Atrial fibrillation is associated with increased risk of fatal and nonfatal cardiovascular events in patients with heart failure and preserved ejection fraction: findings from the IPRESERVE trial. European Journal of Heart Failure Supple ments. Volume 7, Issue Supplement S1, page 161, June 2008
10. Gheroghiade M., Adams Jr K. F., Colucci W.S. Digoxin in the Manage ment of Cardiovascular Disorders. Circulation 2004; 109: 29592964.
 This work is licensed under a
This work is licensed under a