Oana Năstase1, Roxana Enache2, Bogdan A. Popescu1,2, Carmen Ginghină1,2, Ruxandra Jurcuţ1,2
1 “Prof. Dr. C.C. Iliescu” Institute of Emergency for Cardiovascular Diseases
2 University of Medicine and Pharmacy “Carol Davila”, Bucharest
Contact address:
Ruxandra Jurcuț, University of Medicine and Pharmacy “Carol Davila”, “Prof Dr C.C. Iliescu” Institute of Emergency for Cardiovascular Diseases, Sos Fundeni No. 258, 022322 Bucharest. E-mail rjurcut@gmail.com
This is the case of a 29 years-old, pregnant woman who presented in our center for cardiologic evaluation at 28 weeks of pregnancy, being known since infancy with a complex cardiac malformation. The patient was asymptomatic until two weeks before presentation, when she started to describe dyspnea at important efforts, coincidental with progression of pregnancy.
At transthoracic echocardiography significant left ventricular hypertrophy (concentric wall thickness of 16 mm) was found, which appeared secondary to severe aortic stenosis. The continuous wave Doppler analysis of transaortic flow (Figure 1), showed a peak velocity of 4.7 m/s and a mean gradient of 56 mm Hg. There was subvalvular obstruction realized by an incomplete diaphragm (Figure 2). The orifice area at the level of the diaphragm was estimated by 3D transthoracic echocardiography planimetry at 1.8 cm2 (Figure 3). The patient had associated valvular stenosis probably secondary to jet-lesion, estimated by planimetry as moderate (aortic valve area of 1.4 cm2) (Figure 4) and mild aortic regurgitation. An interventricular basal septal aneurysm with a small left to right shunt was also seen (Figure 5). There was persistent ductus arteriosus with left-right shunt seen both from the parasternal short axis view and from the suprasternal view (Figure 6 and Figure 7). The suprasternal view revealed the coexistence of aortic coarctation with a peak Doppler gradient of 31 mmHg, indicating mild obstruction (Figure 8).
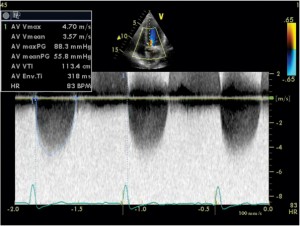
Figure 1. Transthoracic echocardiography, apical five chamber view, continuous wave Doppler examination of transaortic flow: peak flow velocity of 4.7 m/s.
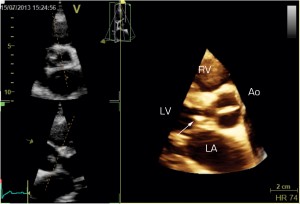
Figure 2. Three-dimensional transthoracic echocardiography parasternal long axis view focus on left ventricular outflow tract: the subaortic valve diaphragm (white arrow). LV = left ventricle, LA = left atrium, RV = right ventricle, Ao = aorta
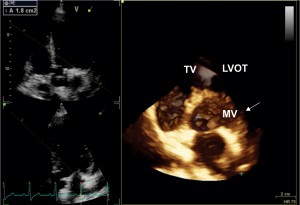
Figure 3. Three-dimensional transthoracic echocardiography apical five-chamber view, reconstruction of the left ventricular outflow tract, view from the left ventricle. A circular diaphragm (white arrow) can be seen in left ventricular outflow tract, creating a stenosis with ananatomical aria at 1.8 cm2.

Figure 4. Three-dimensional transthoracic echocardiography – focus on the aortic valve: moderate valvular aortic stenosis – planimetric anatomic area of 1.4 cm2.
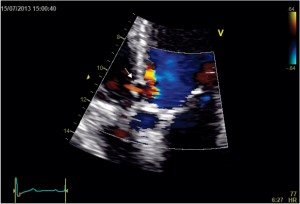
Figure 5. Transthoracic echocardiography, apical five chamber view, focus on aortic valve: interventricular septum basal aneurysm with a small left-right shunt (white arrow) at this level seen at color Doppler.
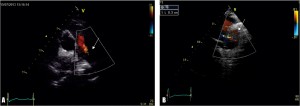
Figure 6. Transthoracic echocardiography, short axis view at great vessels (A) and suprasternal view (B), color Doppler examination: patent ductus arteriosus with a diameter of 5 mm (white arrow).
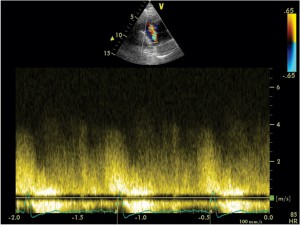
Figure 7. Transthoracic echocardiography, parasternal short axis view, continuous wave Doppler examination of the patent ductus arteriosus shows continuous flow with maximal aorto-pulmonary gradient of 100 mmHg.

Figure 8. Transthoracic echocardiography, suprasternal view: aortic coarctation seen in 2D (A),with a peak systolic gradientof 31 mmHg at continuous wave Doppler examination (B).
Patients with subvalvular aortic stenosis may tolerate pregnancy well as long as they remain relatively asymptomatic and have a normal BP response during exercise1. Obstetric complications may be increased in patients with severe AS (hypertension-related disorders, premature labour)1. Regular follow-up during pregnancy is required by an experienced team. In severe AS, monthly or bimonthly cardiac evaluations including echocardiography are advised to determine symptom status, progression of stenosis, or other complications. In severe aortic stenosis, particularly with symptoms during the second half of pregnancy, caesarean delivery should be preferred with endotracheal intubation and general anesthesia. The patient had an uneventful pregnancy evolution and gave birth to a healthy baby at 38-weeks of pregnancy by caesarean section.
Conflict of interest: none declared.
References
1. Regitz-Zagrosek V, Blomstrom Lundqvist C, Borghi C et al. ESC Committee for Practice Guidelines. ESC Guidelines on the management of cardiovascular diseases during pregnancy: the Task Force on the Management of Cardiovascular Diseases during Pregnancy of the European Society of Cardiology. Eur Heart J. 2011; 32(24):3147-97
 This work is licensed under a
This work is licensed under a