C. Călin1,2, Cecilia Pătru2, D. Deleanu2, Victoria Ulmeanu3, Carmen Ginghină1,2
Article received on 28th September 2012. Article accepted on 16th October 2012.
1 “Carol Davila” University of Medicine and Pharmacy, Bucharest
2 “Prof. Dr. C.C. Iliescu” Institute of Emergency for Cardiovascular Diseases, Bucharest
3 Ovidius University, Faculty of Medicine, Constanţa, County Hospital
Dr. Cosmin Călin, “Prof. Dr. C.C. Iliescu” Institute of Emergency for Cardiovascular Diseases, 258 Fundeni Street, Bucharest.
E-mail: ccalin74@gmail.com
Abstract: Objective – We aimed to study the contribution of several clinical and angiographic factors on left ventricular aneurysm formation in a population of patients with myocardial infarction admitted to a tertiary cardiology center. Methods – We conducted a retrospective study including all consecutive patients presenting with a documented history of ST elevation myocardial infarction between 30 days and 1 year of evolution: 70 patients with a left ventricular aneurysm and 146 patients without a left ventricular aneurysm. We comparatively analysed clinical, angiographic and therapeutic characteristics of these two groups of patients. Results – There were no significant differences between groups regarding age and gender (p>0.08 for both). In patients with left ventricular aneurysm we found an increased number of obese patients (44% versus 29%, p=0.02) and a reduced frequency of smoking patients (41% versus 60%, p=0.006). Between these two groups there were no significant differencies regarding the degree and distribution of coronary lesions but in patients with a history of anterior myocardial infarction the presence of left ventricular aneurysm was significantly correlated to the presence of left anterior descendent artery occlusion (p=0.001). A significantly smaller number of patients with a left ventricular aneurysm were subject to a primary percutaneous coronary intervention (p=0.02). Conclusion – Obesity, non-smoking status, the presence of left anterior descendent artery occlusion and lack of primary percutaneous coronary intervention were all independent correlates of left ventricular aneurysm formation after an acute myocardial infarction.
Keywords: left ventricular aneurysm, myocardial infarction, cardiovascular risk factors, coronary angiography
Rezumat: Obiectiv – Ne-am propus să analizăm impactul factorilor clinici şi angiografici asupra apariţiei anevrismului de ventricul stâng într-o populaţie de pacienţi cu infarct miocardic, investigaţi într-un centru terţiar de cardiologie. Metodologie – Am efectuat un studiu retrospectiv în care au fost incluşi consecutiv pacienţii cu diagnosticul de infarct miocardic cu supradenivelare de ST, aflaţi într-un interval de 1 lună până la 1 an de la momentul infarctului miocardic acut: 70 de pacienţi cu anevrism de ventricul stâng şi 146 de pacienţi fără anevrism de ventricul stâng. Între cele două grupuri s-au analizat comparativ datele clinice, paraclinice şi cele legate de abordarea terapeutică. Rezultate – Între cele două grupuri studiate, nu au existat diferenţe semnificative de vârstă sau sex (p>0,08 pentru ambele). La pacienţii cu anevrism de ventricul stâng, s-a observat o prevalenţă mai mare a obezităţii (44% faţă de 29%, p=0,02) şi mai scăzută a fumatului (41% faţă de 60%, p=0,006). Între cele două grupuri nu au existat diferenţe semnificative referitoare la extensia şi distribuţia leziunilor coronariene, însă în cadrul pacienţilor cu infarct miocardic anterior prezenţa anevrismului s-a corelat semnificativ cu prezenţa ocluziei arterei descendente anterioare (p=0,001). Un procent semnificativ mai mare de pacienţi din lotul celor fără anevrism de ventricul stâng au fost trataţi prin angioplastie coronariană per primam (p=0,02). Concluzii – Obezitatea, statusul de nefumător, prezenţa ocluziei arterei descendente anterioare şi lipsa efectuării angioplastiei coronariene per primam s-au corelat independent cu prezenţa anevrismului de ventricul stâng postinfarct miocardic.
Cuvinte cheie: anevrism de ventricul stâng, infarct miocardic, factori de risc cardiovascular, angiografie coronariană
Background
Left ventricular aneurysm (LVA) is a late complication of myocardial infarction defined by the presence of a distinct protrusive, thin and diskinetic area of the LV wall1. The incidence of LVA depends on the incidence of transmural myocardial infarction in the studied population and the rigorous follow up and subsequent evaluation of patients who have suffered an acute myocardial infarction. The widespread use of echocardiography increased the incidence of LVA, while the extensive use of reperfusion therapy has led to a decrease in the incidence of this complication. The presence of LVA is associated with an increased risk of thromboembolic and arrhythmic events and worsening heart failure1-3. Data regarding the factors associated with the presence of LVA in patients with myocardial infarction are scarce and controversial, coming from studies published over 10 years ago, under different conditions of patient evaluation and therapy4-8. In order to study the impact of clinical factors and those related to the distribution and type of coronary lesions on LVA formation, we aimed to analyse a series of clinical and angiographic parameters in a population of consecutive patients in their first year after an acute ST-segment elevation myocardial infarction (STEMI), investigated according to current recommendations in a tertiary cardiology center.
Methods
We performed a retrospective case-control study, in which we included all patients discharged from the Cardiology Clinic of “Prof. Dr. CC Iliescu” Institute of Emergency for Cardiovascular Diseases with a diagnosis of STEMI between 1st of January 2008 – 1st of July 2010. Patients for whom clinical, echocardiographic and angiographic data were not available or uncertain as well as patients in whom the acute myocardial infarction was not documented were all excluded from the current study. We also excluded patients who were within less than 30 days or more than 1 year after the acute myocardial infarction. We analysed clinical parameters (related to conventional cardiovacular risk factors – smoking, dyslipidemia, obesity, diabetes and functional status at admission), echocardiographic parameters (geometry and function of the LV, the presence and extent of LVA, left atrial size, the presence and degree of mitral regurgitation) and angiographic parameters (number, distribution and extent of coronary lesions). Data related to treatment at the time of acute myocardial infarction and in the first month after the acute episode were also studied. The diagnosis of LVA was established in all patients using transthoracic echocardiography and it was defined as a well-demarcated area of LV wall with systolic and diastolic paradoxical motion9. Angiographic coronary stenosis >50% were considered as significant angiographic lesions.
Statistical analysis
Continuous variables are presented as mean ± standard deviation, while categorical variables are presented as percentages. Student t test was used to compare average values in case of normal dispersion of sample values. In order to highlight the influence of a specific factor ANOVA parametric tests of dispersion analysis were used. Comparison of the two dependent samples was performed using parametric t test or a nonparametric equivalent, Wilcoxon signed rank. Comparisons and associations between studied parameters were analyzed using linear regression analysis and correlation coefficients were calculated using the Pearson method. To study the contribution of multiple factors to the occurrence of an event or the magnitude of effect, multivariate analysis was used: multiple linear regression for continuous variables and logistic regression for dichotomous variables. A two-sided P-value of 0.05 was considered statistically significant. All statistical analyses were performed using SPSS 13.0 software for Windows (SPSS, Inc., Chicago, Illinois).
Results
Study participants
The study group included 216 consecutive patients discharged with a diagnosis of STEMI, in a range between 30 days and 1 year after the documented acute episode, aged between 33 and 85 years (167 men, mean age 60.3 ± 10.4 years). Of these patients, 112 had a history of anterior myocardial infarction, 78 patients had an inferior myocardial infarction and 26 patients had two documented episodes of myocardial infarction (either a history of both anterior and inferior myocardial infarction or reinfarction in a certain territory). Seventy out of the 216 patients included in the study (age 62.1 ± 9.3 years, 58 men) were diagnosed with LVA (group 1) and the remaining 146 patients (age 59.4 ± 10.8 years, 109 men) without LVA formed group 2. There were no significant differences in age or gender (p = 0.08 and p = 0.2, respectively) between the two groups.
The aneurysm location was anterior in 61 patients with LVA, 7 patients had inferior LVA and 2 patients had both inferior and anterior aneurysms. In the group of patients without LVA, 61 patients had a history of anterior myocardial infarction, 71 patients had inferior myocardial infarction and 14 patients had a history of two episodes of acute myocardial infarction (3 patients with reinfarction in the anterior territory, 7 patients reinfarction in the inferior territory and 4 patients had both anterior and inferior myocardial infarction). Thus, of the 112 consecutive patients who had a history of one episode of acute anterior myocardial infarction, 46% were diagnosed with LVA at the present evaluation, compared with only 9% of patients with a history of inferior myocardial infarction, confirming that the anterior location of myocardial infarction is associated with a higher risk of LVA formation.
In patients with LVA, NYHA class at admission was increased compared to patients without LVA (2.0±1.1 versus 1.6±1.0, p=0.003). There was no significant differences between the two groups regarding the presence of angina pectoris at admission, 40% of patients with LVA and 52% of patients without LVA presenting this symptom (p = 0.1).
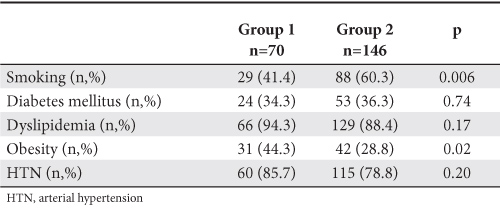
Cardiovascular risk factors
Regarding the prevalence of traditional cardiovascular risk factors in both study groups, the results are shown in Table 1. There is a significantly lower prevalence of smoking and a higher pervalence of obesity in patients with LVA, without significant differences in the frequency of diabetes mellitus, dyslipidemia and arterial hypertension.
Table 1. Prevalence of cardiovascular risk factors in the study population
Echocardiographic parameters
The analysis of echocardiographic characteristics of the two groups revealed the impact of the presence of LVA on LV structure and function, causing the significant change in both LV dimensions and ejection fraction. Left ventricular diameters were significantly increased and estimated LV ejection fraction was significantly lower in patients with LVA than in those without LVA (p <0.001 for all). A higher percentage of patients with ventricular aneurysm showed global LV systolic dysfunction expressed as LV ejection fraction <50% (79% compared to 53% of patients without LV aneurysm, p <0.001). The degree of LV dilatation in patients with LVA was significantly correlated to functional status of these patients, as assessed by NYHA functional class (r = 0.36, p = 0.003 for diastolic LV diameter and r = 0.29, p = 0.019 for systolic LV diameter). Left ventricular ejection fraction was not significantly correlated with NYHA class in patients with LVA (p = 0.06). The degree of mitral regurgitation was significantly higher in patients with LVA, 56% of them showing moderate and severe regurgitation compared with 39% of patients without LVA (p = 0.02).
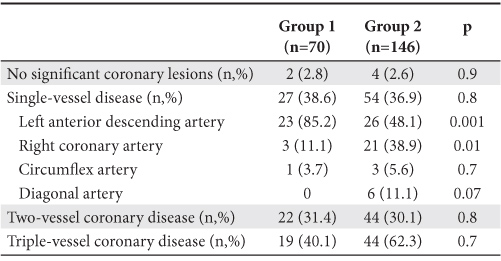
Angiographic parameters
Average time interval from the moment of the acute myocardial infarction to coronary angiography was not significantly different between the two groups (72 ± 65 days in group 1 compared to 56±52 days in group 2, p=0.1). There were no statistically significant differences in terms of number and extent of angiographically significant coronary lesions between the group of patients with LVA and those without LVA (Table 2). In patients with LVA and single-vessel lesion, the left anterior descending artery was the most frequently affected artery, an expected result given the high proportion of patients with anterior myocardial infarction in this group.
Table 2. Distribution of coronary lesions in the two study groups
Management of acute myocardial infarction
We retrospectively analyzed data regarding the reperfusion therapy of the acute myocardial infarction and the management applied in the first month after the onset of myocardial infarction, data available for 68 patients with LVA and 137 patients without LVA. With regard to thrombolytic therapy, there were no significant differences between groups, a similar percentage of patients with and without LVA receiving fibrinolytic therapy (31% versus 32%, p = 0.9). A significantly lower percentage of patients in the group who subsequently developed LVA were treated by primary percutaneous coronary intervention (PCI) (7% versus 20% in patients without LVA, p=0.016). In the first month after the acute event, a similar number of patients in both groups were subject to a PCI addressed to the infarct related coronary artery lesion (4 patients in the group with LVA and 9 patients in the group without LVA, p=0.8) and 6 patients (2 with LVA) required surgical intervention for myocardial revascularization.
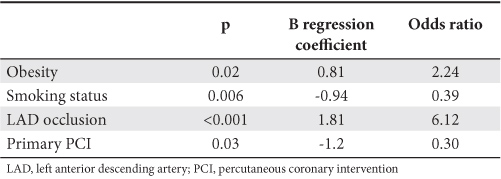
Left ventricular aneurysm correlates
In the whole study group, obesity, non-smoking status, the presence of left anterior descending artery occlusion and the absence of primary PCI were independently correlated with the presence of LVA. Left anterior descending artery occlusion was the most important correlate of LVA formation in patients with a history of myocardial infarction, as shown in Table 3.
Table 3. Correlates of the presence of LVA in patients with a history of myocardial infarction (multiple regression analysis)
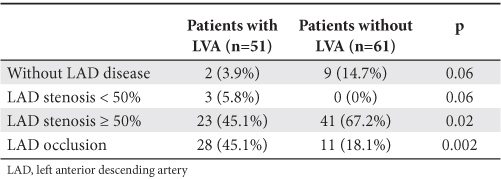
Subgroup analysis of patients with anterior myocardial infarction
Given that patients with inferior myocardial infarction were underrepresented in the group of patients with LVA, we performed a separate comparative analysis in the subgroup of patients with a single episode of anterior myocardial infarction (112 patients, 51 with LVA). Between patients with LVA and those without LVA there
were no significant differences regarding gender (p = 0.07) but patients with LVA were older (62.1 ± 9.8 vs 57.4 ± 10.3 years, p = 0.016) and more frequently obese (43.1% vs 24.6%, p = 0.04). Although patients without LVA were more frequently smokers, this difference did not reach statistical significance (p = 0.08). There were no significant differences between groups regarding the frequency of diabetes mellitus and dyslipidemia. Between patients with LVA and those without LVA there were no significant differences in the distribution of angiographically significant coronary lesions, single vessel, two vessel and triple vessel coronary disease being found in similar proportions in the two groups of patients. On the other hand, left anterior descending artery occlusion was more frequently found in patients with LVA (44% vs. 19%, p=0.001). A higher proportion of patients without LVA had an open infarct related artery at the time of coronary angiography (Table 4).
Table 4. The degree of left anterior descending artery disease in patients with a history of anterior myocardial infarction
Regarding the management of the acute myocardial infarction, a significantly higher proportion of patients with anterior LVA did not receive pharmacological or interventional reperfusion therapy (68.6% vs. 36.1% in patients without LVA, p = 0.001 ). Among patients with anterior LVA, 20% received thrombolysis and 10% were subject to a primary PCI (compared to 36% and 21% in the group without LVA, p = 0.04 and p = 0.08, respectively). Age (p=0.02), obesity (p=0.02), presence of left anterior descending artery occlusion (p=0.03) and lack of reperfusion therapy (p= 0.006) were all independently correlated with the presence of LV aneurysm in patients with anterior myocardial infarction in the multiple regression analysis.
Discussion
In the present study we analyzed a group of 216 consecutive patients admitted to a tertiary cardiology center with the diagnosis of STEMI in the range of 1 month to 1 year after the acute myocardial infarction. Of these, 32% had a left ventricular aneurysm diagnosed by echocardiography, in most cases with an anterior location (87% of cases). This result is comparable with literature data showing a rate of approximately 80-90% of the apical-anterior location in patients with LVA1. The high prevalence of apical aneurysm is explained by the low probability of developing collateral circulation at this level in the absence of homo- and hetero-coronary anastomoses (in most cases the LV apex is vascularized only by terminal branches of the left anterior descending artery)10.
The high incidence of LVA in patients with a history of myocardial infarction in our study could be explained by the fact that the study was conducted in a tertiary cardiology center and only patients who were subject to a coronary angiography were included, thus, the population being a highly selected one. Shen et al8, in a study published in 1992 reported a prevalence of 39% of LVA in patients with a history of anterior myocardial infarction undergoing coronary angiography.
There was no significant difference in terms of age between patients with and without LVA, a fact noted by other authors in similar studies4,5,8. We have not found a gender predisposition for the development of LVA in our study. Contrary to our results, Tikiz et al. reported a predisposition of the female patients for the development of LVA7, but these results were not confirmed by other authors5,8.
The current study shows that there are no significant differences between patients with and without LVA regarding the presence of diabetes mellitus, dyslipidemia and arterial hypertension. The impact of arterial hypertension on the risk of LVA formation is controversial. Although there are authors who suggest that arterial hypertension may predispose to LVA formation in patients with myocardial infarction11, this was not confirmed by other authors5,7,8. Increased blood pressure in the acute phase of myocardial infarction may contribute to infarction expansion and increased risk of LVA formation. On the other hand, a long-term history of arterial hypertension is often associated with LV hypertrophy and an increased thickness of LV walls might be protective against the development of a ventricular aneurysm. In our study, data regarding the blood pressure values in the acute phase of myocardial infarction or the degree of left ventricular hypertrophy were not available.
Our results show a significantly lower prevalence of smoking and an increased prevalence of obesity in patients with LVA. Although the role of smoking as a risk factor for acute myocardial infarction and sudden death is already established12, several studies have shown that smoking status is a predictor of short-term favorable prognosis after acute myocardial infarction13-15, with a trend to a lower long-term mortality16 in smokers. It was also demonstrated that infarct related coronary artery patency is more common in smokers after thrombolysis for acute STEMI, with a better coronary flow, suggesting a higher rate of reperfusion in these pa-
tients. Our data fall on this line, showing an association between smoking status and the absence of LVA. These results could be partially explained by the fact that there is data showing that smoking is associated with the development of collateral coronary circulation17. The presence of a greater proportion of obese patients in the LVA group may also be related to coronary collateral circulation development, which is hampered by the presence of obesity and metabolic syndrome, as demonstrated in clinical studies18.
Comparing the echocardiographic characteristics of the two groups, we observed the impact of LVA on the structure and function of the left ventricle, with an increase of LV dimensions and a decrease of LV ejection fraction. This is an expected result and in agreement with literature data. In a study of Mariotti et al6, including a smaller number of patients with anterior myocardial infarction, a significant increase in LV end diastolic volume and a significant decrease in LV ejection fraction were also found in patients with LVA. In the present study, the increase in LV dimensions was significantly correlated with NYHA functional class, confirming the relationship between LV dilatation and heart failure in patients with LVA.
Although some authors have shown that the presence
of LVA is more often associated with single-vessel coronary disease5,7 while other studies reported a more frequent association with triple-vessel disease19-21, our results show no significant difference between groups in terms of coronary lesions extension. Separate analysis of patients with anterior myocardial infarction showed that the presence of left anterior descending artery occlusion is significantly correlated with the presence
of LVA. Moreover, left anterior descending artery occlusion is an independent determinant of the presence of LVA both in patients with anterior myocardial infarction and in the whole study group. Similar to our results, Forman et al5 showed a statistically significant correlation between the presence of LVA and the occlusion of left anterior descending artery associated with poor collateral circulation in a small group of patients with anterior myocardial infarction. These data highlight the importance of residual coronary flow to the infarct zone to prevent aneurysm formation in patients with an open infarct related artery.
The retrospective analysis of data regarding the reperfusion therapy did not show a significant difference between patients with and without LVA regarding fibrinolysis therapy, this result being similar to available data.7 On the other hand, we found a significantly higher prevalence of primary PCI use in patients without subsequent LVA. In our study population only a small proportion of patients (16%) were treated by primary PCI, since the present study included patients treated for STEMI between 2008-2010. This is similar to data published by the investigators of RO-STEMI registry in 2011, 15% of all patients included between 2007-2009 being subject to a primary PCI22.
The benefit of primary PCI, including the reduction of LV remodeling, was already demonstrated in many studies, but no other dedicated studies confirm its role in preventing LVA formation in patients with myocardial infarction.
Study limitations
The main limitation of our study derives from its retrospective nature, which allowed the evaluation of a small number of available parameters. There was no data regarding the presence of angina pectoris before the occurrence of the acute myocardial infarction, this factor being already demonstrated as an important correlate of LVA formation7. The low representation of patients with inferior myocardial infarction in the group of patients with LVA did not allow a separate analysis of these patients.
Although only patients investigated by a coronary angiography were included in our study, data regarding the objective grading of collateral coronary circulation was available in a limited number of patients.
Since patients included in the present study were not subject to a consistent follow up, lack of these data did not allow the analysis of the predictive role of clinical, echocardiographic and angiographic parameters.
Conclusions
Left ventricular aneurysm was diagnosed in one third of patients admitted in a tertiary cardiology center with a diagnosis of STEMI in the first year of evolution. The presence of LV aneurysm has a negative impact on functional status, LV structure and function, the increase in LV dimensions being correlated to a poor functional status in patients with LVA.
In patients with a history of myocardial infarction the presence of obesity was significantly associated with the presence of LVA, while smoking might be a protective factor against LVA formation.
The extent and distribution of coronary lesions were similar in patients with LVA and those without LVA. In patients with anterior myocardial infarction the occlusion of the left descending artery was significantly correlated with the presence of ventricular aneurysm.
Obesity, non-smoking status, the presence of left anterior descending artery occlusion and the absence of primary PCI were independently correlated with the presence of LVA in our study group.
Conflict of interests: none declared.
References
1. Morrow DA, Gersh BJ. Chronic Coronary Artery Disease. In Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine, 8th ed. 2007; 1397-1399.
2. Abildstrom SZ, Ottesen MM, Rask-Madsen C, Andersen PK, Rosthoj S, Torp-Pedersen C, Kober L. Sudden cardiovascular death following myocardial infarction: the importance of left ventricular systolic dysfunction and congestive heart failure. Int J Cardiol 2005;104:184-189.
3. Matei C, Apetrei E. Evoluţia anevrismului ventricular stâng cu şi fără tromboză. Revista Română de Cardiologie.1996;6(2):57.
4. Inoue T, Morooka S, Hayashi T, Takayanagi K, Sakai Y, Fujito T, Takabatake Y. Features of coronary artery lesions related to left ventricular aneurysm formation in anterior myocardial infarction. Angiology. 1993;44(8):593-8.
5. Forman MB, Collins HW, Kopelman HA, Vaughn WK, Perry JM, Virmani R, Friesinger GC. Determinants of left ventricular aneurysm formation after anterior myocardial infarction: a clinical and angiographic study. J Am Coll Cardiol. 1986;8(6):1256-62.
6. Mariotti R, Petronio AS, Robiglio L, Balbarini A, Mariani M. Left ventricular aneurysm: clinical and hemodynamic data. Clin Cardiol. 1990;13(12):845-50.
7. Tikiz H, Atak R, Balbay Y, Genç Y, Kütük E. Left ventricular aneurysm formation after anterior myocardial infarction: clinical and angiographic determinants in 809 patients. Int J Cardiol. 2002;82(1):7-14.
8. Shen WF, Tribouilloy C, Mirode A, Dufossé H, Lesbre JP. Left ventricular aneurysm and prognosis in patients with first acute transmural anterior myocardial infarction and isolated left anterior descending artery disease. Eur Heart J. 1992 Jan;13(1):39-44.
9. Apetrei E. Anevrismul ventricular. In Apetrei E. Ecocardiografie, Ed. Medicală Bucureşti, 1990:205-207.
10. Filipoiu F, Ginghină C. Noţiuni de anatomie clinică a cordului. În Ginghina C, sub redacţia, Mic tratat de cardiologie, Ed Academiei Romane, 2010; 15:35.
11. Schlichter J, Hellerstein HK, Katz LM. Aneurysm of the heart: a correlative study of 102 proved cases. Medicine 1954;33:43–86.
12. Kannel WB, McGee DL, Gastelli WP. Latest perspective on cigarette smoking and cardiovascular disease: the Framingham Study. J Cardiac Rehabil 1984;4:267-77.
13. Barbash GI, White HD, Modan M, et al, for the Investigation of the International Tissue Plasminogen Activator/Streptokinase Morbidily Trial. Significance of smoking in patients receiving lhrombolytic therapy for acute myocardial infarction: experience gleaned from the Investigation of the International Tissue Plasminogen Activator/Streptokinase Morbidily Trial. Circulation1993;87:53-8.
14. Mueller HS, Cohen LS, Braunwald E, et al, for the TIMI Investigators. Predictors of early morbidity and mortality after thrombolytic therapy for acute myocardial infarction: analysis of patient subgroup in the Thrombolysis in Myocardial InFarction (TIMI) Trial, Phase II. Circulation 1992;85:1254/o4.
15. Grines CL, Topol EJ, O’Neill WW, et al. Effect of cigarette smoking on outcome after thrombolytic therapy for myocardial infarction. Circulation 1995;91:298-303.
16. Ishihara M, Sato H, Tateishi H, et al. Clinical implications of cigarette smoking in acute myocardial infarction: Acute angiographic findings and long-term prognosis. Am Heart J 1997;134:955-60.
17. Koerselman J, de Jaegere PP, Verhaar MC, Grobbee DE, van der Graaf Y; SMART Study Group. Coronary collateral circulation: the effects of smoking and alcohol. Atherosclerosis. 2007;191(1):191-8.
18. Sasmaz H, Yilmaz MB. Coronary collaterals in obese patients: impact of metabolic syndrome. Angiology. 2009;60(2):164-8.
19. Cabin HS, Roberts WC. True left ventricular aneurysm and healed myocardial infarction. Clinical and necropsy observations including quantification of degrees of coronary arterial narrowing. Am J Cardiol. 1980 Nov;46(5):754-63.
20. Faxon DP, Ryan TJ, Davis KB, McCabe CH, Myers W, Lesperance J, Shaw R, Tong TG.Prognostic significance of angiographically documented left ventricular aneurysm from the Coronary Artery Surgery Study (CASS). Am J Cardiol. 1982 Jul;50(1):157-64.
21. Greere V, Iacob M, Pinte F, Ţintoiu I, Dumitrescu S, Bujor A, Grama L. Aspecte coronarografice și terapeutice în anevrismul de ventricul stang. Stetoscop – Revista de informare pentru medici 2005; 44:19-26.
22. Ţînţ D, Rădoi M, Petriş A, Datcu DM, Sinescu C, et al. Vârsta, factorii de risc cardiovascular, terapia şi mortalitatea intraspitalicească la pacienţii cu infarct miocardic acut cu supradenivelare de segment ST. Un subraport al Registrului Român pentru infarctul miocardic acut cu supradenivelare de segment ST (RO-STEMI). Romanian Journal of Cardiology. 2011;26:14-20.
 This work is licensed under a
This work is licensed under a