Alina Scridon1,2, R. C. Şerban2, A. Matei2, Ioana Smărăndiţa Lacău3, A. Elkahlout4, D. Dobreanu1,2
Article received on the 4th September 2012. Article accepted on the 9th October 2012.
1 University of Medicine and Pharmacy of Târgu Mureş, Physiology Department, Târgu Mureş, Romania
2 Târgu Mureş Emergency Clinical County Hospital, Cardiology Department, Târgu Mureş, Romania
3 Hiperdia Medical Center, Bucharest, Romania
4 Târgu Mureş Emergency Clinical County Hospital, Laboratory of Cardiac Catheterization, Târgu Mureş, Romania
Dr. Alina Scridon, University of Medicine and Pharmacy of Târgu Mureş, Department of Physiology; 38 Gheorghe Marinescu Street, 540000, Târgu Mureş, Romania. Fax: 004 02 65 21 04 07.
E-mail: alinascridon@yahoomail.com
Abstract: ST-segment abnormalities are most frequently encountered in the presence of coronary artery disease, but similar abnormalities can be triggered by various other conditions. We report a notable case of myocarditis mimicking acute myocardial infarction. A 21-years-old male, without any personal cardiac history or history of recent viral illness, presented with a 48h history of chest pain, in the absence of any ECG abnormalities. Twenty-four hours later, he was asymptomatic, but ST-elevation was observed on the ECG in DI and aVL leads and he presented elevated cardiac enzymes (troponin I 4.46 ng/mL). Inflammatory markers were within normal ranges. Coronary angiogram showed spasm of the first diagonal artery. The next day he presented ST-segment normalization and negative T-waves in DI and aVL leads, even higher levels of troponin I (5.35 ng/mL), while all other cardiac enzymes were already within normal ranges. Cardiac magnetic resonance imaging showed myocardial edema and a patchy distribution of delayed enhancement of the left ventricular lateral wall, allowing the diagnosis of acute myocarditis, likely related to a parvovirus B-19 infection.
Keywords: myocarditis, acute myocardial infarction, cardiac magnetic resonance imaging, parvovirus B-19.
Rezumat: Anomaliile segmentului ST sunt, în general, consecinţa unei suferinţe coronariene, dar pot fi întâlnite în multiple alte circumstanţe. Prezentăm un caz particular de miocardită care mimează infarctul miocardic acut. Un tânăr de 21 de ani, fără antecedente cardiace sau de infecţie virală recentă, se prezintă acuzând durere toracică de circa 48h, în absenţa oricăror modificări ECG. După 24h, pacientul este asimptomatic, dar prezintă supradenivelarea segmentului ST în DI şi aVL pe ECG şi markeri de necroză miocardică crescuţi (troponina I 4,46 ng/mL). Markerii inflamatori sunt în limita valorilor normale. Coronarografia evidenţiază spasm al primei artere diagonale. La 24h de la internare se observă normalizarea segmentului ST şi unde T negative în DI şi aVL şi niveluri mai ridicate de troponină I (5,35 ng/mL), în timp ce toţi ceilalţi markeri miocardici sunt deja în limite normale. Examenul RM cardiac evidenţiază arii de hipersemnal miocardic pe secvenţa T2 şi aspect de edem la nivelul peretelui lateral al ventriculului stâng, permiţând diagnosticul de miocardită acută, verosimil secundar unei infecţii cu parvovirus B-19.
Cuvinte cheie: miocardita, infarct miocardic acut, imagistica cardiacă prin rezonanţă magnetică, parvovirus B-19
Introduction
Due to non-specific symptoms and a lack of universally accepted and standardized diagnostic criteria, acute myocarditis remains one of the most challenging diagnoses in cardiology. It can present with a broad spectrum of symptoms, ranging from fatigue to fulminant congestive heart failure and sudden death, including acute ST-elevation myocardial infarction-like syndrome.1 We present a case of myocarditis in a young patient who presented with chest pain and ST-elevation in DI and aVL leads on the ECG, mimicking an acute myocardial infarction (MI).
Case report
A 21-year-old Caucasian male, without any personal cardiac history, presented to his family physician with a 2-day history of atypical chest pain. Clinical cardio-pulmonary examination was unremarkable and initial ECG showed no abnormalities, so the patient was immediately discharged with a recommendation of re-evaluation 24h later. At that time, the patient was asymp-
tomatic, but ST-elevation in DI and aVL leads was observed on the ECG, and the patient was directed to the emergency department of our hospital. His social history was negative for drug use. He denied any recent acute stress or travelling abroad and he presented no recent history of viral illness.
On arrival to our emergency department, the patient was asymptomatic, hemodynamically stable, afebrile, and had a benign physical exam. Arterial blood pressure was 120/80 mmHg and heart rate was 51 beats/minute.
Laboratory data revealed normal complete blood count, coagulation study, C-reactive protein, erythrocyte sedimentation rate and fibrinogen levels. An initial set of cardiac enzymes was positive for troponin I (4.46 ng/mL) and creatine kinase myocardial band (42 ng/mL). Liver function tests were abnormal for aspartate aminotransferase (85 UI/L) and lactate dehydrogenase (628 UI/L).
The ECG (Figure 1) showed ST-elevation in DI and aVL leads, negative T-waves in DII, DIII, aVF, and V4 to V6 leads, and ST-depression in DIII and aVR leads. The echocardiography showed slightly depressed left ventricular ejection fraction (51%), and hypokinetic apical and mid-ventricular regions of the lateral left ventricular wall. There was no evidence of pericardial thickening or effusion.
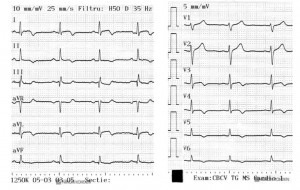
Figure 1. The ECG recorded in the emergency department showing ST-elevation in DI and aVL leads, suggesting acute lateral ST-elevation myocardial infarction, negative T waves in DII, DIII, aVF, and V4 to V6 leads, and ST depression in DIII and aVR leads.
Acute lateral MI was suspected, but coronary spasm, myocarditis or pericarditis could not be ruled out. Left heart catheterization was performed. Ventriculography revealed segmental wall motion abnormalities of the apical and mid-ventricular regions of the lateral wall of the left ventricle and slightly decreased left ventricular ejection fraction (50%). Coronary angiography showed normal left and right coronary arteries. The first diagonal artery presented spasm in the middle segment (Figure 2A) that ceded after intracoronary administration of nitroglycerine (Figure 2B).
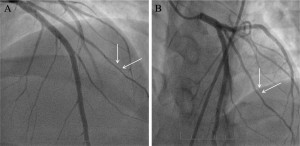
Figure 2. Coronary angiography. (A) Right-anterior-oblique cranial view of the left coronary artery showing patent left anterior descending artery and left circumflex artery and spasm of the middle segment of the first diagonal artery (arrows), (B) that ceded after intracoronary administration of nitroglycerine (arrows; postero-anterior cranial view).
On the following day, the ECG showed ST-segment normalization, negative T-waves in DI and aVL leads and positive T-waves in inferior leads (Figure 3). Peak troponin I was measured 48h after the last episode of chest pain (5.35 ng/mL), when all other cardiac enzymes were already within normal ranges.
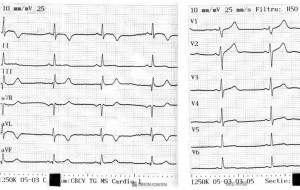
Figure 3. The ECG recorded the day after admission showing ST-normalization together with negative T-waves in DI and aVL leads, and positive T waves in inferior leads.
Cardiac magnetic resonance imaging (CMRI) was performed. Cine images revealed that the wall motion abnormalities had completely resolved. On delayed enhancement imaging there was diffuse patchy mid-myocardial and epicardial late gadolinium enhancement involving the left ventricular lateral wall (Figure 4, A and B). T2-weighted imaging revealed high-intensity signal in these areas, suggesting the presence of myocardial edema. Overall, these findings were strongly suggestive of myocarditis.
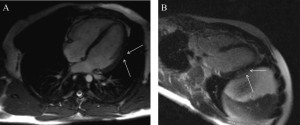
Figure 4A, B. Short-axis CMRI images showing diffuse patchy mid-myocardial and epicardial late gadolinium enhancement involving the left ventricular lateral wall.
After being started on angiotensin-converting enzyme inhibitors, the patient remained asymptomatic and by the moment of discharge he had no echocardiographic abnormalities.
Discussion
Differential diagnosis between acute MI and myocarditis can be very challenging. This case highlights the usefulness of CMRI in making a confirmatory diagnosis of acute myocarditis in a patient that presents with chest pain, ST-elevation on the ECG, positive cardiac enzymes and an echocardiogram suggestive of acute MI, in the absence of angiographically significant coronary artery disease.
In fact, around 10% of patients that present with signs and symptoms suggestive of coronary artery disease actually have normal or minimal coronary lesions on angiography.2 Although the most frequent suspicion in such cases is acute MI due to coronary spasm or spontaneously reperfused coronary occlusion, a definitive diagnosis is usually not formulated.3
Similar clinical features can also be found in patients that present with acute myocarditis. In such cases, several criteria have been proposed to make the diagnosis of myocarditis likely. According to Dec, in patients who present with chest pain, diffuse ECG abnormalities that extend beyond the distribution of a single coronary artery, no segmental wall motion abnormalities or global left ventricular hypokinesis on echocardiography or ventriculography, the diagnosis of myocarditis should be considered.4 However, in certain cases with focal myocarditis, the ECG pattern perfectly mimics ST-elevation acute MI.5
Beyond the common difficulties in diagnosing myocarditis, our patient presented with several misleading features: atypical chest pain, ST-elevation on ECG 24h after the last episode of chest pain, peak troponin I levels 48h after the last episode of chest pain, when all other markers of myocardial injury were already normal, absence of recent history of viral illness, normal values of all inflammatory markers, and segmental left ventricular wall motion abnormalities on echocardiography, in the absence of significant coronary artery disease. Moreover, coronary angiography revealed coronary vasospasm.
Although coronary spasm could explain a number of clinical features, the unusual evolution of ECG abnormalities and cardiac enzymes raised suspicions of myocarditis, which prompted us to look for infiltrative disease with CMRI.
This pattern, with severe vasospasm mimicking acute MI, is most commonly seen in patients with biopsy-proven parvovirus B19-induced myocarditis.6 Several factors, such as increased oxidative stress, endothelial dysfunction, or reduced nitric oxide bioavailability, may be involved in parvovirus B19-induced myocarditis-related vasospasm.7
To date, the only widely available method for the definitive diagnosis of myocarditis is endomyocardial biopsy, but with limited sensitivity and a non-negligible risk of death due to cardiac perforation.8 Recently, CMRI has been shown to be an effective technique that can non-invasively diagnose acute myocarditis based on a characteristic pattern of contrast enhancement.9 Contrarily to typical CMRI findings in patients with MI (i.e., subendocardial enhancement), myocarditis shows a pattern of contrast enhancement originating primarily from the epicardium and sparing the subendocardial layer.7,10
The CMRI in our patient was classic for myocarditis. Moreover, the location of myocardial lesions on CMRI also sustains parvovirus B-19 as etiologic agent in our patient.7 According to Marholdt et al., parvovirus B-19 infection is characteristically associated with delayed enhancement in the lateral wall of the left ventricle.7
Inefficient immune response against viral infection may explain the myocardial damage in parvovirus B-19 infection. This impaired immune response could also explain the absence of an inflammatory syndrome in our patient. The absence of recent history of viral illness made the diagnosis of myocarditis even more challenging. However, unlike for other pathogens, latent persistence of parvovirus B-19 genomes that may last for years without causing any clinical symptoms cannot be excluded.
Conflicts of interests: the authors declare that no conflict of interest exists.
References
1. Monney PA, Sekhri N, Burchell T, et al. Acute myocarditis presenting as acute coronary syndrome: role of early cardiac magnetic resonance in its diagnosis. Heart, 2010; 97:1312-18.
2. Iuliano L, Micheletta F, Napoli A, Catalano C. Myocardial infarction with normal coronary arteries: a case report and review of the literature. J Med Case Rep, 2009; 3:24.
3. Simion A, Huidu S, Stanca I, et al. Aspecte particulare de diagnostic în miocardite acute. Revista Română de Cardiologie, 2008; 23: A59.
4. Dec WG. Introduction to clinical myocarditis. In Myocarditis. From bench to bedside. Ed: Cooper LT. Totowa: New Jersey’ Humana Press Inc, 2003, 257-81.
5. Mottard N, Mewton N, Bonnefoy E, and col. Acute myocarditis mimicking lateral myocardial infarction. Anaesth Intensive Care, 2008; 36(5): 739-42.
6. Kühl U, Pauschinger M, Bock T, and col. Parvovirus B19 Infection Mi-
micking Acute Myocardial Infarction. Circulation, 2003; 108:945-50.
7. Mahrholdt H, Wagner A, Deluigi CC, and col. Presentation, patterns of myocardial damage, and clinical course of viral myocarditis. Circulation, 2006; 114: 1581-90.
8. Deckers JW, Hare JM, Baughman KL. Complications of transvenous right ventricular endomyocardial biopsy in adult patients with cardiomyopathy: a seven-year survey of 546 consecutive diagnostic procedures in a tertiary referral center. J Am Coll Cardiol, 1992; 19:43-7.
9. Oancea Irinel D, Sararu E, Tatu A, et al. Rolul examenului „late enhancement” prin rezonanță magnetică cardiacă în evaluarea modificărilor miocardice, cu implicații diagnostice și în tratament. Revista Română de Cardiologie, 2009; 24:A233.
10. Laissy JP, Messin B, Varenne O, and col. MRI of acute myocarditis: a comprehensive approach based on various imaging sequences. Chest, 2002; 122:1638-48.
 This work is licensed under a
This work is licensed under a