Carmen Elena Pleșoianu1, Magda Bădescu2, Cătălina Arsenescu Georgescu3,4
Article received on the 17th June 2012. Article accepted on the 6th August 2012.
1 „Grigore T. Popa” University of Medicine and Pharmacy Iasi, Faculty of Medicine
2 „Grigore T. Popa” University of Medicine and Pharmacy Iasi, Faculty of Medicine, Pathophysiology Department
3 „Grigore T. Popa” University of Medicine and Pharmacy Iasi, Faculty of Medicine, Cardiology Department
4 Institute of Cardiovascular Diseases “Prof. Dr. George I. M. Georgescu“ Iasi, Romania
Dr. Carmen Elena Pleșoianu, „Grigore T. Popa” University of Medicine and Pharmacy Iași, 16 University Street, 700115 Iasi, Romania.
Tel: 0742126934, E-mail: carmenplesoianu@gmail.com
Abstract: Background – Ischemic heart disease is responsible for most serious morbidity and mortality in diabetic patients who have a 2 to 4 fold increase in the risk of coronary artery disease compared to non diabetic patients. Objective – To evaluate the particular features of ischemic heart disease in men with type 2 diabetes mellitus. Materials and methods – A retrospective, case-control study created by comparative analysis of anamnestical, paraclinical and coronarographycal data of 224 men angiographycally investigated for ischemic heart disease that were divided according to the presence of diabetes into 2 groups with similar age distribution. Results – We objectified a high prevalence of ischemic heart disease in diabetic patients aged 60-69 (39.28%). The diabetic population more commonly presented obesity, hypertension, hypetriglyceridemia and low HDL cholesterol (43.75% versus 30.36%, 75% versus 66.06%, 62.50% versus 49.11% and 55.36% versus 50.89%, respectively). Diabetic men had more frequently three vessel disease (37.5% versus 34.82%), in-stent restenosis after angyoplasty and indication of coronary artery bypass grafting. Conclusions – In men with type 2 diabetes mellitus, the atherosclerosis risk factors (obesity, hypertension and atherogenic dyslipidemia) were better expressed and the coronary artery disease was more severe with complications after angyoplasty and required more often surgical myocardial revascularization.
Keywords: ischemic heart disease, diabetes mellitus, coronarography
Rezumat: Introducere – Boala cardiacă ischemică este responsabilă pentru o mare parte a morbidităţii grave şi mortalităţii pacienţilor diabetici, care au risc de 2 – 4 ori mai mare pentru dezvoltarea unei boli coronariene comparativ cu pacienții fără diabet. Obiectiv – Evidenţierea particularităţilor cardiopatiei ischemice la bărbații cu diabet zaharat tip 2. Material şi metodă – Studiu retrospectiv, caz-martor, realizat prin analiza comparativă a datelor anamnestice, paraclinice şi coronarografice a 224 bărbați investigați angiografic pentru cardiopatie ischemică divizați în funcţie de prezenţa diabetului în 2 loturi cu distribuţie similară pe grupe de vârstă. Rezultate – Am obiectivat o prevalenţă crescută a cardiopatiei ischemice la pacienții diabetici din grupa de vârstă 60-69 ani (39,28%). La populaţia diabetică au fost mai frecvent observate obezitatea, hipertensiunea arterială, hipetrigliceridemia şi HDL colesterolul scăzut (43,75% versus 30,36%, 75% versus 66,06%, 62,50% versus 49,11% şi respectiv 55,36% versus 50,89%). Pacienții cu diabet au prezentat mai frecvent afectare tricoronariană (37,5% versus 34,82%), restenoză intrastent postangioplastie și indicație de bypass aortocoronarian. Concluzii – La bărbații diabetici, anumiți factori de risc ai aterosclerozei – obezitatea, hipertensiunea arterială și dislipidemia aterogenă au fost mai bine exprimaţi iar afectarea coronariană a fost mai severă, cu complicații postangioplastie și indicație mai frecventă de revascularizare miocardică chirurgicală.
INTRODUCTION
Diabetes mellitus (DM) has become a major public health and economic problem. It is considered that the prevalence of diabetes worldwide, estimated at 2.8% (171 million) in 2000 will increase to 4.4% (366 million) in 20301. In this context, cardiovascular disease, the major cause of morbi / mortality among diabetic patients requires a comprehensive management with an aggressive strategy of risk factors control.
OBJECTIVE
To identify the characteristics of coronary heart disease in men with type 2 diabetes mellitus.
MATERIALS AND METHODS
To achieve our goal we performed a retrospective, case – control study, analyzing clinical and laboratory data of patients with ischemic heart disease (IHD) with and without type 2 DM. The data were extracted from the observational sheets from the archives of the Institute of Cardiovascular Diseases „Prof. Dr. George IM Georgescu” (IBCV) Iasi.
The clinical spectrum of IHD included silent myocardial ischemia, various forms of angina pectoris (stable, unstable) and myocardial infarction. Glycemic status was evaluated according to American Diabetes Association criteria (ADA) 2003 as follows: normal glucose regulation was defined by the values of fasting plasma glucose (FPG) <5.6 mmol/L (100 mg/dl) and the diagnosis of diabetes was determined by two values of FPG ≥7.0 mmol/L (126 mg/dl) (venous plasma glucose).
The inclusion criteria for the first group were: male gender, presence of diabetes mellitus, diagnosis of IHD, hospitalization and angiographic investigation in IBCV Iasi during the period of January 1 to December 31, 2008.
The inclusion criteria for the second group (control group) were: male gender, normal glucose control, diagnosis of IHD, angiographic investigation in IBCV Iasi in 2008, age distribution similar to the first group (we have chosen randomly from the non diabetic men, angiographically investigated for IHD in 2008 similar numbers of patients for each age group identified in the diabetic group).
For both groups, the presence of severe aortic stenosis represented exclusion criteria.
Statistical analysis with comparisons of the diabetic patients with matched controls was performed in Microsoft EXCEL program using t test (t-test assuming unequal variances for two samples) and coefficient of variation (CV). Statistic significance threshold was considered p = 0.05. According to the CV, a significance test that asses the representativeness of the mean, the mean was highly representative (CV ≤17%), moderate representative (CV = 17-35%), weakly representative (CV = 35-50%) or unrepresentative (CV >50%).
RESULTS
112 diabetic men without severe aortic stenosis were investigated for IHD in IBCV in the year 2008.
The mean age of the diabetic group was 61.32 years (CV 14.38%).
The age distribution of patients objectified a high prevalence of invasive coronary investigation in diabetic men from the age group of 60-69 years (39.28%) (Figure 1).
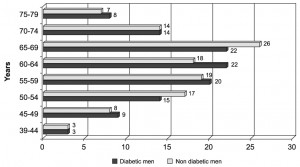
Figure 1. Distribution of the 2 groups according to age.
The majority of patients were from the urban area (84.82% in the first group and 72.32% in the second one).
There were no statistically significant differences in the duration of hospitalization in the 2 groups (the mean duration of hospitalization was 7 days).
The incidence of stroke was similar in the 2 groups (7.14% in the diabetic group versus 6.25% in the non diabetic group).
Cardiovascular heredity, smoking and chronic ethanol consumption were more frequent in the control group compared with the diabetic one (56.89% versus 55.17%, 66.07% versus 58.92% and 21.42% versus 7.14%, respectively).
All diabetic patients had type 2 DM. 18.75% of them had a positive family history of diabetes. There were 17 cases of newly diagnosed DM. The duration of diabetes varied largely (0-30 years) with a mean duration of 6.41 years. Insulin therapy was used in 20% of cases.
Glycated hemoglobin was measured in 66 patients and had a mean value of 8.31%. Diabetes mellitus was generally poorly controlled. 54.55% of the patients had a glycated hemoglobin >8%, 30.3% presented a glycated hemoglobin of 6.5-8% and 15.15% a glycated hemoglobin <6.5%. Only 6.25% had a fasting plasma glucose <108 mg/dl.
Patients were classified according to the body mass index (BMI) as follows: BMI = 18.5 to 24.99 kg/m2 – normal weight, BMI = 25 to 29.99 kg/m2 – overweight, BMI = 30 to 34.99 kg/m2 – grade I obesity, BMI = 35 to 39.99 kg/m2 – grade II obesity, BMI >40 kg/m2 – grade III obesity.
We objectified statistically significant differences (p = 0.00004) in terms of weight status between the 2 groups. Normal weight status was 2 times more frequent in the control group compared with diabetic patients. The average body mass index was 29.46 kg/m2 (CV 13.63%) in the diabetic group and 27.46 kg/m2 (CV 12.52%) in matched controls. The diabetic men were superior in number in all 3 groups of obesity (Figure 2).
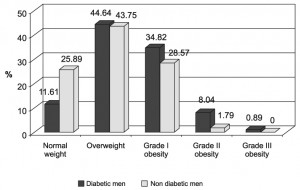
Figure 2. Distribution of the 2 groups according to weight status.
Depending upon the value of blood pressure, patients were divided in the following categories: normotensive – systolic blood pressure (SBP) <139 mmHg (men without DM) / <130 mmHg (diabetic men) and/or diastolic BP (DBP) <89 mmHg (men without diabetes) / 80 mmHg (diabetic men), grade 1 hypertension – SBP = 140-159 mmHg and/or DBP = 90-99 mmHg, grade 2 hypertension – SBP = 160-179 mmHg and/or DBP = 100-109 mmHg and grade 3 hypertension – SBP ≥180 mmHg and/or DBP ≥110 mmHg.
We noted statistically significant differences in the tensional status between the 2 groups (p = 0.013) (Figure 3).
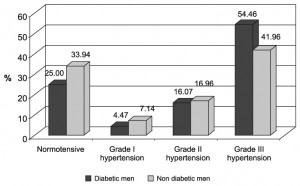
Figure 3. Distribution of the 2 groups according to blood pressure.
Normal blood pressure was more common in men without diabetes (33.94% versus 25%). The majority of diabetic men had high grade hypertension (54.46% versus 41.96%).
Orthostatic hypotension was 3 times more common in the diabetic group (8.92% versus 2.67% in matched controls).
We objectified statistically significant differences (p = 0.028) in the values of resting heart rate between the 2 groups. 10.71% of diabetic men compared with 5.35% of matched controls had a resting heart rate >90 beats/minute while a resting heart rate <70 beats/minute was encountered in 42.85% of diabetics compared with 60.71% of non diabetic patients.
The lipid status was evaluated by the values of triglycerides (TG), total cholesterol (Col T), LDL cholesterol (LDL c) and HDL cholesterol (HDL c). The lipid profile of diabetic patients was characterized by elevated TG (62.50% versus 49.11%) (p = 0.034) (Figure 4). The mean value of TG was 178 mg% in the diabetic group compared with 160 mg% in the control group.
Diabetic men more frequently presented low HDL cholesterol (55.36% versus 50.89%) but without reaching statistical significance threshold (p = 0.29). No statistically significant differences were registered between total cholesterol (p = 0.24) and LDL cholesterol (p = 0.08). The mean value of total cholesterol was 174 mg% (CV 27.07%) in the diabetic group and 178 mg% (CV 21.67%) in the control group, and the LDL cholesterol had a mean value of 98.5 mg % in the first group (CV 39.34%) and 105.21 mg% in the second one (CV 29.98%).
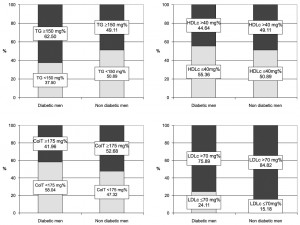
Figure 4. Distribution of the 2 groups according to lipid pattern.
There were statistically significant differences (p = 0.039) in the values of serum creatinine between the 2 groups. The mean value of creatinine was 1.18 mg% in diabetic patients and 1.09 mg% in matched controls. 12.5% of diabetic patients compared with 7.14% of matched controls presented a serum creatinine >1.5 mg /dl. 19.67% of diabetic patients presented proteinuria and 38,8% glycosuria.
Kinetic disorders were recorded in similar percentages in both groups (52.52% in the diabetic group and 52.23% in the non diabetic group). We objectified statistically significant differences between the thickness of interventricular septum (IVS) (p = 0.03) and left ventricular posterior wall (LVPW) (p = 0.0012). Average thickness of the IVS was 13.08 mm (CV 15.19%) in the diabetic group compared with 12.35 mm (CV 15.55%) in the control group and the LVPW was 12.42 mm (CV 13.61%) in the first group compared with 11.69 mm (CV 14.6%) in the second one.
Men without diabetes that were angiographycally investigated for IHD more frequently presented the diagnosis of myocardial infarction (MI) – acute (AMI – 11.61% versus 9.82%) or in their medical history (56.25% versus 45.54%) (Figure 5).
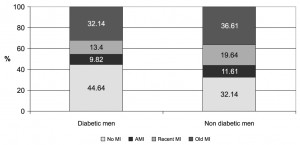
Figure 5. Distribution of the 2 groups according to the presence of myocardial infarction.
Among patients with myocardial infarction thrombolysis was performed in 6 diabetic patients and 18 patients without diabetes.
The analysis of angiographic data showed that diabetic men had more frequent multivessel disease compared with non diabetics (three vessel disease 37.50% versus 34.82%) (Figure 6). The incidence of IHD without coronary lesions was very low in both groups.
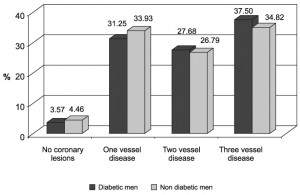
Figure 6. Distribution of the 2 groups according to the coronary lesions.
The left main coronary artery was more commonly affected in people without diabetes (8.92% versus 5.35% in diabetic patients).
The majority of patients with one vessel disease presented left descending artery lesions (51.43% in the diabetic group and 47.37% in the control group), followed by stenosis of right coronary artery (25.71% and 39.47%, respectively) and left circumflex artery (22.86% and 13.16%, respectively).
For the two vessel disease, the most common association was in both groups the lesions on left descending and right coronary artery (54.84% in diabetic patients and 46.67% in matched controls).
Percutaneous coronary angioplasty with stenting was performed in equal percentages in the 2 groups (60.71%) but the use of pharmacologically active stents was predominant in the diabetic group (22.05% versus 10.29%).
Acute stent thrombosis was diagnosed in 2 diabetics and caused the death of the patients.
12.5% of diabetic patients compared with 4.46% of patients without diabetes required intervention for in-stent restenosis.
More diabetic men presented surgical myocardial revascularization indication (27.67% versus 25% of patients without diabetes).
DISCUSSIONS
Diabetic patients accumulate more atherogenic risk factors than patients without diabetes, including hypertension, obesity and lipid abnormalities and the coronary risk increases proportionally with the intensity of these factors2.
Hypertension is present at diagnosis in many patients with type 2 diabetes3. Most convincing evidence for the importance of hypertension in diabetes comes from the United Kingdom Prospective Diabetes Study in which at nine years follow-up each 10 mmHg reduction in mean systolic blood pressure was associated with a 12% decrease in the risk of developing a cardiovascular complication, the lowest risk occurring at a systolic blood pressure below 120 mmHg4. Our study confirms the high prevalence of hypertension in diabetic patients. Only one quarter of diabetic patients were normotensive in our study while the majority had high grade hypertension.
Obesity is also an independent risk factor for cardiovascular disease5. Eighty percent of patients with type 2 DM are either obese or overweight and obesity independently predicts cardiovascular disease and coronary atherosclerosis6. Our study objectified statistically significant differences between weight status in the 2 groups with a marked prevalence of obesity in diabetic patients.
- There are some differences in the lipid profile in diabetic patients compared with those without diabetes that may explain the accelerated development of atherosclerosis. Lipid abnormalities characteristic of type 2 diabetes include elevated triglycerides, low levels of HDL cholesterol and elevated concentrations of small and dense LDL cholesterol particles7. In addition, for any concentration of plasma lipoproteins, patients with diabetes have more severe coronary artery disease compared with patients without diabetes. This increased risk may be due in part to qualitative differences of lipoprotein fractions (small and dense LDL cholesterol) that are more susceptible to oxidation and penetrate more easily the intima of the vessel8. In our study we objectified statistically significant differences in the levels of triglycerides between the 2 groups. The mean values of total cholesterol and LDL cholesterol were higher in men without diabetes but without statistical significance (p = 0.24 respectively 0.078). For technical reasons we could not qualitatively evaluate the LDL particles and similar total LDL cholesterol concentrations cannot exclude the presence of high concentrations of small dense particles. Unlike data on lipid profile in diabetic women that we obtained in a previous study9, there were no statistically significant differences in the level of HDL cholesterol that had a mean value of 42 mg/dl in both groups. We noted a modest percentage of achievement of lipid therapeutic target values10 in the diabetic population 58.04% for total cholesterol, 24.11% for LDL cholesterol, 44.64% for HDL cholesterol and 37.5% for triglycerides.
A particularity of our study is that more non diabetic patients angiographycally investigated for IHD in 2008 in our center had a history of myocardial infarction compared with diabetic patients. A possible explanation is the higher addressability of diabetic patients who are referred for exploration due to the frequent presence of multiple risk factors, the better medical education that allows presentation for investigation before the instauration of a clinical major cardiovascular event but also the fact that patients with type 2 diabetes have a high rate of asymptomatic coronary disease11. However, even though 55.36% of diabetic patients compared with 67.86% of matched controls had a major cardiovascular event, angiographic data revealed no statistically significant differences between the number of coronary lesions in the 2 groups (p = 0.28), an argument that diabetes mellitus is a coronary heart disease equivalent12. Moreover, we noted a tendency of diabetic patients to have three vessel disease. Our data are consistent with the literature on the susceptibility of diabetic patients to develop multivessel disease13,14.
Although procedural success rates are similar in patients with and without diabetes receiving elective percutaneous coronary intervention with stent15,16, diabetic patients have higher rates of short and long term complications. Diabetic patients have higher rates of restenosis and coronary artery disease progression compared with patients without diabetes17-19 requiring repeat revascularization even though restenosis was reduced by the use of drug eluting stents instead of bare metal stents in diabetic patients with stable or unstable coronary disease with similar risk of death or MI20. The use of drug eluting stents compared with bare metal stents has drastically reduced the rate of restenosis in diabetic patients. Furthermore, DM is an independent predictor of acute stent thrombosis21. In our study acute stent thrombosis was present only in the diabetic group with a fatal outcome and the rate of repeat revascularization for in stent restenosis was greater in diabetics compared to matched controls. In addition, due to the characteristics of the coronary lesions, more diabetic patients compared to controls were reffered for surgical myocardial revasculaization.
CONCLUSIONS
There are statistically significant differences between certain risk factors for coronary heart disease in men with type 2 diabetes mellitus compared with non diabetic patients. Men with diabetes are more frequently hypertensive, obese, have higher triglycerides levels and left ventricular hypertrophy.
Diabetic men present more frequently coronary multivessel disease that require surgical myocardial revascularization techniques and develop more commonly complications when percutaneous angioplasty with stenting is performed.
The diabetic patients with coronary heart disease require a cardio diabetological approach with a better control of diabetes and aggressive strategy against all cardiovascular risk factors.
Conflict of interests: none declared.
References
1. Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004; 27: 1047–53.
2. Grundy SM, Benjamin IJ, Burke GL, et al. Diabetes and Cardiovascular Disease: A Statement for Healthcare Professionals From the American Heart Association. Circulation 1999; 100: 1134-46.
3. Chobanian AV, Bakris GL, Black HR, Cushman WC. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report. JAMA 2003; 289: 2560-71.
4. Adler AI, Stratton IM, Neil HA, et al. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ 2000; 321: 412-9.
5. Poirier P, Giles TD, Bray GA, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity and Metabolism. Circulation 2006; 113: 898-918.
6. Bogers RP, Bemelmans WJ, Hoogenveen RT, et al. Association of overweight with increased risk of coronary heart disease partly independent of blood pressure and cholesterol levels: a meta-analysis of 21 cohort studies including more than 300 000 persons. Arch Intern Med 2007; 167: 1720-8.
7. Beckman JA, Creager MA, Libby P. Diabetes and atherosclerosis. Epidemiology, pathophysiology and management. JAMA 2002; 287: 2570-81.
8. Berry C., Tardif J.C., Bourassa M.G. Coronary Heart Disease in Patients With Diabetes Part I: Recent Advances in Prevention and Noninvasive Management. J. Am. Coll. Cardiol 2007; 49: 631-42.
9. Boldea C, Bădescu M, Arsenescu Georgescu C. Characteristics of coronary artery disease in women with type 2 diabetes mellitus. Romanian Journal of Cardiology 2011; 26: 14-20.
10. Reiner Ž, Catapano AL, De Backer G et al. ESC/EAS Guidelines for the management of dyslipidaemias: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur Heart J 2011; 32: 1769-1818.
11. Anand DV, Lim E, Lahiri A, Bax JJ. The role of non-invasive imaging in the risk stratification of asymptomatic diabetic subjects. Eur Heart J 2006; 27: 905-12.
12. Graham I, Atar D, Borch-Johnsen K, et al. European guidelines on cardiovascular disease prevention in clinical practice. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Eur J Cardiovasc Prev Rehabil 2007; 14 Suppl 2: S1-113.
13. Fox CS, Coady S, Sorlie PD, et al. Trends in cardiovascular complications of diabetes. JAMA 2004; 292: 2495-9.
14. Scognamiglio R, Negut C, Ramondo A, et al. Detection of coronary artery disease in asymptomatic patients with type 2 diabetes mellitus. J Am Coll Cardiol 2006; 47: 65-71.
15. Suero JA, Marso SP, Jones PG, et al. Procedural outcomes and long-term survival among patients undergoing percutaneous coronary intervention of a chronic total occlusion in native coronary arteries: a 20-year experience. J Am Coll Cardiol 2001; 38: 409-14.
16. Mathew V, Gersh BJ, Williams BA, et al. Outcomes in patients with diabetes mellitus undergoing percutaneous coronary intervention in the current era: a report from the Prevention of REStenosis with Tranilast and its Outcomes (PRESTO) trial. Circulation 2004; 109: 476-80.
17. Mehran R, Dangas GD, Kobayashi Y, et al. Short- and long-term results after multivessel stenting in diabetic patients. J Am Coll Cardiol 2004; 43: 1348-54.
18. West NE, Ruygrok PN, Disco CM, et al. Clinical and angiographic predictors of restenosis after stent deployment in diabetic patients. Circulation 2004; 109: 867-73.
19. Berry C., Tardif J.C., Bourassa M.G. Coronary Heart Disease in Patients With Diabetes: Part II: Recent Advances in Coronary Revascularization J. Am. Coll. Cardiol. 2007; 49: 643-656.
20. Stenestrand U, James S, Lindbäck J, et al, for the SCAAR/SWEDEHEART study group Safety and efficacy of drug-eluting versus bare metal stents in patients with diabetes mellitus: long-term follow-up in the Swedish Coronary Angiography and Angioplasty Registry (SCAAR) Eur Heart J 2010; 31(2): 177-86.
21. Iakovou I, Schmidt T, Bonizzoni E, et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA 2005; 293: 2126-30.
 This work is licensed under a
This work is licensed under a