Cristina Vacarescu1, Lucian Petrescu1,2, Cristian Mornos1,2, Emilia-Violeta Goanta3, Simina Crisan1,2, Miruna Ocos2, Mihai-Andrei Lazar2, Oana Patru2, Ramona-Alina Cozlac2, Dragos Cozma1,2
1 Institute of Cardiovascular Disease, Timisoara, Romania
2 “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania
3 Department of Cardiology, Emergency County Hospital, Craiova, Romania
Abstract: Objectives – to assess the outcome of direct current cardioversion (DCCV) in patients (pts) with symp-tomatic persistent atrial fibrillation (PAF) and LA dilatation. Methods – We analyzed 84 pts (49 male) aged 64.6±9.8 y.o, with PAF <1 year, EHRA class >2 and LAVI >40 ml/m2. Echocardiographic parameters included: ejection fraction (EF), LA diameter (LAD), LA area (LAA) and LA volume (LAV – planimetry 4 chamber view). For each pt we calculated LAVI (left atrium volume index). All pts received proper anticoagulation and antiarrhythmic treatment. The management included a full control of blood pressure before cardioversion during the 3 weeks of prior anticoagulation. Pts with maximum of 3 conversion/year were admitted. Results – Arterial hypertension was diagnosed in 80% of pts, while 13% had coronary artery disease. All pts received proper anticoagulation (36 pts on dabigatran, 5 pts on apixaban, 43 pts on acenocumarol with INR values in therapeutic limits) and antiarrhythmic treatment: amiodarone (57 pts), propafenone (4 pts), flecainide (13 pts), sotalol (3 pt), amiodarone+fl ecainide (7 pts). All 84 pts underwent uncomplicated DCCV (1 to 3 external electrical shocks with energy between 150 and 200 J). Parameters: LAD 4.6±0.6 cm; LAA 30.1±4.8 cm2 (range 20-46 cm2); LAV was 114.5±29.5 ml (range 60-220 ml); EF 48.4±7.8 %. Calculated LAVI was 52.37±8.9 ml/m2. The mean CHA2DS2-VASc score was 3.02±1.28. DCCV was successful in restoring sinus rhythm (SR) in 79 pts (94%). The mean total follow-up was 22±9 months, while 25 pts (30%) needed reconversion after 9±4 months. Another 13 pts (15%) were left in permanent AF at the end of the follow-up period. Conclusion – Electrocardioversion of symptomatic PAF in LA dilatation showed a positive outcome, even if multiple DCCV and adapted strategy in all pts is needed.
Keywords: atrial fibrillation cardioversion, severe left atrium dilatation, novel oral anticoagulants
INTRODUCTION
Atrial fibrillation (AF) is the most common arrhythmia in adults, with a rising incidence in the past decades due to increased life expectancy and improved diagno-ses ability. Western European studies report a preva-lence ranging from 2.0% to 4.7% of the population1, and by the end of 2030 it is estimated that in Europe will be 14-17 milion of people with AF2.
AFFIRM, the largest randomized controlled trial which compared rate versus rhythm control strate-gies, concluded that is no clear advantage in restoring sinus rhythm3, nevertheless sustained forms of AF may be associated with increased cardiovascular mortality and remain an aditional target for therapy, particularly in symptomatic patients1. At this moment, the 2016 ESC Guidelines for the management of atrial fibrillati-on recommends a rhythm control therapy to improve symptoms in AF patients who remain symptomatic on adequate rate control therapy, but studies to assess if a modern rhythm control strategy leads to a reducti-on in major cardiac adverse events (MACE) are still in progress4.
Assessing factors and predictors of SR maintenance after cardioversion, may be useful for a better identi-fication of patients who would benefit the most from a rhythm control strategy. Atrial remodelling plays an important role in AF reccurence, and lower left atrium index volume (LAVI) represents a strong and indepen-dent predictor of SR maintenance after performing a cardioversion5. However many other factors such as time in AF, older age, LV function, significant mitral valve disease, rheumatic heart disease are involved in maintaining SR, and a clinical base judgement should be aproach individualised for each patient6.
Despite a failure to decrease mortality, SR restau-ration is associated with improvements in symptoms and quality of life, and diminished frequency of AF sho-uld be considered an acceptable outcome rather than only accepting as a succes absolute AF supression7.
PATIENTS AND METHODS
We analyzed a retrospective cohort study of patients hospitalized for atrial fi brillation (PAF) in whom SR was obtain by direct current cardioversion (DCCV). The criteria for patient selection included: hospitaliza-tion for PAF (duration <1 year), EHRA class >2, LAVI >40 ml/m2. Exclusion criteria were defined as: severe valvular disease (severe valvular stenosis and/or re-gurgitation), more than 3 previous DCCV/year, serum creatinine level >2.5 mg/mL and severe co-morbidity (neoplasia, renal or hepatic failure, severe pulmonary disease, etc).
All patients received proper anticoagulation (direct oral anticoagulants or acenocumarol with INR values in therapeutic range) and antiarrhythmic treatment. In case of unsuccessful DCCV different antiarrhythmic strategies were tried. The management included a full control of blood pressure before cardioversion during the 3 weeks of prior anticoagulation.
Transthoracic echocardiography was performed in all patients before DCCV, and this data was conside-red the baseline echocardiography. A GE VIVID 7/9 ultrasonographic system (Vivid 7, GE Health Medical, Milwaukee, WI, USA) was used for ultrasound ima-ges acquisition, with ECG simultaneously recording for each patient. The echocardiographic examination was performed with patients in the left lateral decu-bitus position, using standard views and techniques8. Standard echocardiographic measurements included interventricular septum (IVS), left ventricular end-di-astolic diameter (LVEDD) and volume (LVEDV), and ejection fraction (LVEF) (Simpson’s method). All LA measurements were performed at end-systole just before mitral valve opening and maximal atrium size was considered for evaluation8. LA diameter (LAd) was measured by M-mode in the parasternal long-axis view, LA surface area (LAV) and LA volume (LAV) were measured in the apical 4-chamber view.
Data regarding clinical evolution, SR maintenan-ce and major cardiac events (MACE) incidence were obtained by retrospective analyze of patients follow-up visits in the clinic. Participants were followed for 22±9 months from the date of cardioversion. Major cardiac-vascular events were defined as stroke, syste-mic or pulmonary embolism, myocardial infarction, major bleeding and death.
STATISTICAL ANALYSIS
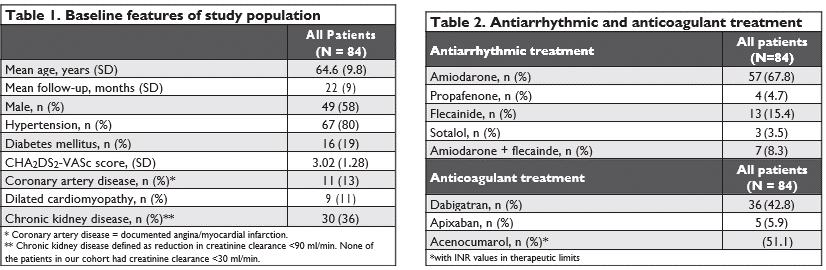
In Table 1 we present the baseline clinical and demo-graphic features of population as means or percentage (± standard deviation). In Table 3 we analyzed baseline echocardiographic parameters presented as means (± standard deviation) and range. All analyses were per-formed using OpenEpi (A Collaborative, Open-Sour-ce Project in Epidemiologic Computing The OpenEpi Collection of Epidemiologic Calculators, Version 3.01 — Released April 4 and revised April 6, 2013). Continuous variables were compared between groups using unpaired t test (variables with normal distribution) or Mann-Whitney U test (non-normally distributed varia-bles). A p value <0.05 was considered significant.
RESULTS
This study included 84 patients (49 male, aged 64.6±9.8 y.o). The demographic and clinical characteristics are presented in Table 1, antiarrhythmic and anticoagulant treatment are presented in Table 2.
Uncomplicated direct current cardioversion, using 1 to 3 external electrical shocks with energy betwe-en 150 and 200 J, was performed in all patients. In case of unsuccessful DCCV, different antiarrhythmic strategies were tried and another attempt of cardi-oversion was made during the same hospitalization. In the amiodarone group 9 patients failed to convert to SR after first attempt of DCCV: for 3 of them we added flecainide, 2 were switched from amiodarone to sotalol and 4 pts were switched from amiodarone to flecainide.
DCCV was successful in restoring sinus rhythm in 79 pts (94 %), for 5 pts AF was considered permanent. The mean total follow-up was 22±9 months, while 25 pts (30%) needed reconversion after 9±4 months. Another 13 pts (15%) were left in permanent AF at the end of the follow-up period. There were no ma-jor cardiac events, no embolic events, major bleeding events, or deaths during the follow up period.
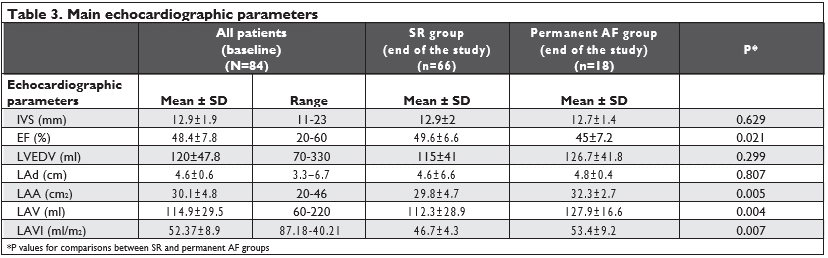
The main echocardiographic parameters of all pa-tiens at baseline are presented in Table 3, togheter with the echocardiographic characteristics for the 2 groups: SR group and permanent AF group at the end of the follow up period.
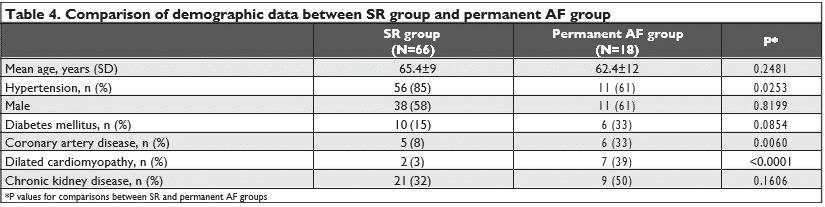
All pts had moderate to severe LA dilatation with LAVI >40 ml/m2, (LAVI mean±SD: 52.37 ± 8.9 ml/m2, LAVI range 87.18-40.21 ml/m2). LA area and volume, LA volume index and EF were echocardiographical pa-rameters with statistical signifi cance (p<0.05). In the permanent AF group we found a higher incidence of hypertension, coronary artery disease and dilated cardiomyopathy. We obtain no significant statistical diffe-rence between the SR group and the permanent AF group regarding age or sex distribution.
DISCUSSION
In the present patient cohort with moderate to severe LA dilatation and symptomatic persistent AF, electri-cal cardioversion was safe and feasable with a good outcome for a high number of pts. LAVI represents a strong predictor of SR maintanance after DCCV, and we also find a significant statistical difference between the 2 groups: SR pts and permanent AF pts, but note that both groups of pts had severe LA dilatation, with LAVI >40 ml/m2. Recent studies suggest that novel ecocardiographic parameters such as atrial emptying fraction, right atrial volume or different index com-binig diastolic and sistolic Tissue Doppler parameters can be use to predict AF recurrence after DCCV9,10,11. With all this, the best ecocardiographical and clinical predictor of SR maintanance is yet to be validated.
Due to the retrospective study design, one of the major limitations was the inability of assessing reliable data regarding more complex ecochardiographic pa-rameters such as diastolic function, strain parameters.
Clinical score as HATCH (where the acronym stan-ds for hypertension, age >75 years, transient ischaemic attack or stroke, chronic obstructive pulmonary disea-se, and heart failure) is useful in predicting short-term success of DCCV at early stages for patients with AF, for whom the use of a rhythm-control strategy is plan-ned12, but literature data is sparse regarding DCCV in pts with persistent AF and severe LA dilatation.
An adapted antiarrhythmic treatment strategy can play a key role in achieving SR or SR maintenance after DCCV, as is also suggested by a recent data-mining project of the Flecainide Short-Long trial which states that a strategy of flecainide pretreatment for 48 h pri-or to planned electrical cardioversion may be a useful planning of a strategy of long-term rhythm control13.
Earlier studies showed that a rhythm control stra-tegy has no clear advantges on long term mortality compared to a rate control approach, but the situati-on is changing in the last years due to tehnical advance in interventional therapy for this arrhythmia and also the progression in better defining and diagnosing the high risks associated with AF, such as asymptomatic brain embolisations and AF-related brain hypoperfu-sion14. CABANA and EAST-AFNET4 are two under-goind, randomized, open label trials which asses the benefits of an interventional rhythm control strategy in preventing complication of AF15,16. A recent study published in January 2017 which included 6.545 parti-cipants with AF without heart failure (HF) at baseline, analysed the signifi cant clinical predictors of incident HF and its prognostic effect on long-term outcomes and concluded that HF among patients with AF is common, is more likely to be HF with preserved ejec-tion fraction, and is associated with poor long-term outcomes17, so the question if is there a need to treat AF aggressively still remains a subject of debate.
CONCLUSION
Electrocardioversion of symptomatic persistent atrial fibrillation in severe left atrium dilatation showed a positive outcome, even if multiple electrocardioversi-on and adapted strategy in all patients is needed.
Conflict of interest: None declared.
Authors’ contributions: Concept/design: Cristina Vacarescu (CV), Lucian Petrescu (LP), Cristian Mor-nos (CM), Emilia-Violeta Goanta (EMG), Simina Crisan (SC), Miruna Ocos (MO), Mihai-Andrei Lazar (MAL), Oana Patru (OP), Ramona-Alina Cozlac (RAC), Dra-gos Cozma (DC). Critical revision of article: Dragos Cozma (DC), Lucian Petrescu (LP), Cristian Mornos (CM), Simina Crisan (SC).
Abbreviations
DCCV – Direct Current Cardioversion
EF – Ejection Fraction
HR – Heart Failure
INR – International Normalized Ratio
IVS – Interventricular Septum
LA – Left Atrium
LAA – Left Atrial Area
Lad – Left Atrium Diameter
LAV – Left Atrial Volume
LAVI – Left Atrial Volume Index
LV – Left Ventricule
LVEDD – Left Ventricular End-Diastolic Diameter LVEDV – Left Ventricular End-Diastolic Volume MACE – Major Cardiac Events
PAF – Persistent Atrial Fibrillation RA – right atrium SR – Sinus Rhythm
References
1. Shukla A, Curtis AB. Avoiding permanent atrial fibrillation: treat-ment approaches to prevent disease progression. Vasc Health Risk Manag. 2014;10:1-12. doi: 10.2147/VHRM.S49334
2. Zoni-Berisso M, Lercari F, Carazza T, Domenicucci S. Epidemiology of atrial fibrillation: European perspective. Clin Epidemiol. 2014 Jun 16;6:213-20. doi: 10.2147/CLEP.S47385
3. Corley SD, Epstein AE, DiMarco JP, et al; AFFIRM Investigators. Relationships between sinus rhythm, treatment, and survival in the Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) Study. Circulation. 2004; 109(12):1509-1513.
4. Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, Cas-tella M, Diener HC, Heidbuchel H, Hendriks J, Hindricks G, Ma-nolis AS, Oldgren J, Popescu BA, Schotten U, Van Putte B, Vardas P, Agewall S, Camm J, Baron Esquivias G, Budts W, Carerj S, Cassel-man F, Coca A, De Caterina R, Deftereos S, Dobrev D, Ferro JM, Filippatos G, Fitzsimons D, Gorenek B, Guenoun M, Hohnlo-ser SH, Kolh P, Lip GY, Manolis A, McMurray J, Ponikowski P, Ro-senhek R, Ruschitzka F, Savelieva I, Sharma S, Suwalski P, Tamargo JL, Taylor CJ, Van Gelder IC, Voors AA, Windecker S, Zamorano JL, Zeppenfeld K. 2016 ESC Guidelines for the management of atrial fi brillation developed in collaboration with EACTS. Europace. 2016 Nov;18(11):1609-1678. Epub 2016 Aug 27
5. Akdemir B, Altekin RE, Küçük M, Yanikoglu A, Karakaş MS, Aktaş A, Demir I, Ermiş C. The significance of the left atrial volume in-dex in cardioversion success and its relationship with recurrence in patients with non-valvular atrial fibrillation subjected to electri-cal cardioversion: a study on diagnostic accuracy. Anadolu Kardiyol Derg. 2013 Feb;13(1):18-25. doi: 10.5152/akd.2013.003
6. Abu-El-Haija B, Giudici MC. Predictors of long-term maintenance of normal sinus rhythm after successful electrical cardioversion. Clin Cardiol. 2014 Jun;37(6):381-5. doi: 10.1002/clc.22276. Epub 2014 Apr 3.
7. Morin DP, Bernard ML, Madias C, Rogers PA, Thihalolipavan S, Es-tes NA 3rd. The State of the Art: Atrial Fibrillation Epidemiology, Prevention, and Treatment. Mayo Clin Proc. 2016 Nov 5. pii: S0025-6196(16)30538-9. doi: 10.1016/j.mayocp.2016.08.022
8. Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the american society of echocardiography and the European association of cardiovascular imaging. Eur Heart J Cardiovasc Imaging 2015; 16:233-71.
9. Luong CL, Thompson DJ, Gin KG, Jue J, Nair P, Lee PK, Tsang MY, Barnes ME, Colley P, Tsang TS. Usefulness of the Atrial Emptying Fraction to Predict Maintenance of Sinus Rhythm After Direct Cur-rent Cardioversion for Atrial Fibrillation. Am J Cardiol. 2016 Nov 1;118(9):1345-1349. doi: 10.1016/j.amjcard.2016.07.066. Epub 2016 Aug 13
10. Luong C, Thompson DJ, Bennett M, Gin K, Jue J, Barnes ME, Col-ley P, Tsang TS. Right atrial volume is superior to left atrial volume for prediction of atrial fibrillation recurrence after direct current cardioversion. Can J Cardiol. 2015 Jan;31(1):29-35. doi: 10.1016/j. cjca.2014.10.009. Epub 2014 Oct 12.
11. Ari H, Ari S, Sarigül OY, Coşar S, Doganay K, Emlek N, Tütüncü A, Kivanç E, Çamci S, Aktaş I, Karakuş A, Zengin I, Bozat T, Melek M. A Novel Index Combining Diastolic and Systolic Tissue Doppler Parameters for Prediction of Atrial Fibrillation Recurrence. Echocar-diography. 2016 Jul;33(7):1009-15. doi: 10.1111/echo.13212. Epub 2016 Mar 20.
12. Emren SV, Kocabaş U, Duygu H, Levent F, Şimşek EÇ, Yapan Emren Z, Tülüce S – The role of HATCH score in predicting the success rate of sinus rhythm following electrical cardioversion of atrial fibrillation. Kardiol Pol. 2016;74(9):978-84. doi: 10.5603/KP.a2016.0044. Epub 2016 Apr 4.
13. Oto E, Okutucu S, Katircioglu-Öztürk D, Güvenir HA, Karaa-gaoglu E, Borggrefe M, Breithardt G, Goette A, Ravens U, Steinbeck G, Wegscheider K, Oto A, Kirchhof P. Predictors of sinus rhythm after electrical cardioversion of atrial fibrillation: results from a data mining project on the Flec-SL trial data set. Europace. 2016 Jul 4. pii: euw144.
14. Kautzner J. [Is there a need to treat atrial fibrillation aggressively?]. Vnitr Lek. 2015 May;61(5):417-20.
15. ClinicalTrials.gov. Catheter Ablation vs Anti-arrhythmic Drug The-rapy for Atrial Fibrillation Trial (CABANA). https://clinicaltrials.gov/ ct2/show/NCT00911508
16. ClinicalTrials.gov. Early Treatment of Atrial Fibrillation for Stroke Prevention Trial (EAST). http://www.easttrial.org
17. Pandey A, Kim S, Moore C, Thomas L, Gersh B, Allen LA, Kowey PR, Mahaffey KW, Hylek E, Peterson ED, Piccini JP, Fonarow GC; ORBIT-AF Investigators and Patients. Predictors and Prognos-tic Implications of Incident Heart Failure in Patients With Preva-lent Atrial Fibrillation, JACC Heart Fail. 2017 Jan;5(1):44-52. doi: 10.1016/j.jchf.2016.09.016.
 This work is licensed under a
This work is licensed under a