Benhalla Hanane1, Noureddine Malika2, Habbal Rachida3
1 Universitary hospital of Casablanca, Morocco
2 Professor, Universitary Hospital of Casablanca, Morocco
3 Professor, Universitary Hospital of Casablanca, Morocco
Contact address:
Benhalla Hanane, Doctor
Universitary Hospital of Casablanca, Morocco
Contact phone: 00212661885875. E-mail: hanane.benhalla@yahoo.fr
Address: 23 Lotissement Lamia, Bourgogne Casablanca, Morocco.
Abstract: We report a case of myocardial infarction in the course of Behcet’s disease in a 25 year old man with no coronary risk factor. The diagnosis of Behcet’s disease was selected to deep venous thrombosis of the lower limb, bipolar ulceration, posterior uveitis, and a positive pathergy test. This is of prior myocardial infarction complicated by a ventricular fibrillation reduced by external shock. Coronary angiography showed a threatening lesion of the anterior interventricular coronary. In the literature, twenty cases of myocardial infarction have been reported in Behçet’s disease. The pathophysiology, accountability diagnostic and treatment are still difficult to explain.
Keywords: Behcet disease, myocardial infraction, coronary angiography
Introduction
Behcet disease is a disease prevalent around the Mediterranean and Japan. First case described in 1937 by H. Behcet with a triad: oral and genital ulceration, skin and ocular manifestations. Familial cases are rare less than 5%, with a male predominance 7.10 for symptomatic forms, the vascular disease is found in 7-29% of cases essentially thrombophlebitis, whereas arterial involvement is rare. Rare heart attacks are reported, myocardial infarction is a exceptional form of revelation of the disease we present a case.
Case report
A young man of 28 years without cardiovascular risk factor, admitted for myocardial infarction in the second day complicated by heart failure and hemodynamic instability.
Clinically on admission: TA 90/50 mmHg, heart rate of 130 bpm, diffuse crackles in the pulmonary areas, scalable genital aphtosis.
The ECG is a QS appearance and extended anterior ischemia (Figure 1). The immediate outcome was marked by the occurrence of ventricular fibrillation reduced by external electric shock.
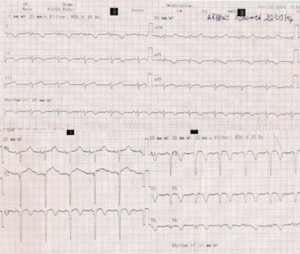
Figure 1. ECG showing a myocardial infarction with ST segment elevation in the anterior territory witn the presence of Q wave of necrosis.
Biology
Troponins to 25 times normal, Anemia: HB 7.4 g/dl, leukocytosis at 19000 Normal kidney function, serology HIV, Hepatitis B and C negative. Positive inflammation results (CRP 26 mg/l, high fibrinogen)
At the echocardiography
A very dilated left ventricle, ejection fraction at 25% with a global hypokinesia and apical akinesia with an adherent thrombus (Figure 2), a moderate ischemic mitral regurgitation. The patient underwent medical treatment with diuretics for heart failure, with a platelet antiaregant based clopidogrel and aspirin with an effective anti coagulation by heparins of low molecular weight-based enoxaparin and nitrates for the residual angina presented by the patient. Diagnosis of Behcet’s disease was suspected in cardiac involvement in a young patient in the presence of genital and oral ulceration, besides the finding of deep vein thrombosis of the lower limb during the hospitalization: a pathergy test came back positive, and at the ophtalmplogical control an uveitis was found, so the diagnosis of cardiac involvement in relation with the Behcet disease was comfirmed.
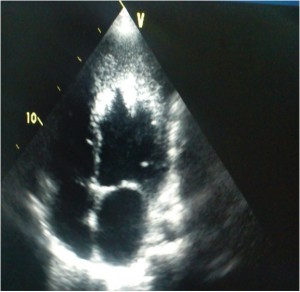
Figure 2. Echo cardiographic Image showing a dilated left ventricle with an adherent apical thrombus.
Anti phospholipid antibodies were negatives such as the coagulation factors: protein S, protein C, ATIII.
Coronary angiography performed on the second day of hospitalization revealed a tight stenosis of the left anterior coronary artery with implantation of a drug-eluting stent (Figure 3).
In collaboration with internists first bolus of Endoxan following by corticosteroid was received by the patient, 15 days away from the acute phase of his myocardial infarction because of the risk of cardiac rupture and possible curb after his heart failure. After the third dose of Endoxan, the patient was slightly improved with the medical treatment (inhibitor of angiotensin converting enzyme-blocker-Clopidogrel-aspirin-Acenocoumarol) but with persistence of severe left ventricular dysfunction and apical thrombus.

Figure 3. Image showing a tight angiographic appearance thrombotic coronary stenosis Inter ventricular anterior.
Discussion
Behcet’s disease is a systemic inflammatory disease of unknown origin. It occurs mainly in young adults with mucocutaneous, ocular, neurological and vascular signs. The usual treatment is symptomatic, appealing to anti-inflammatory drugs, including colchicine, immunosuppressive and / or biotherapy. It is a chronic relapsing and which it is impossible to predict the course. As such, any physician to take care of a patient followed for Behcet’s disease should be particularly vigilant in case of unusual symptoms.
The main emergency situations to consider are:
- ophthalmologic complications (at stake visual prognosis);
- vascular complications (estimated 20% mortality);
- venous complications (80% of cases) or artery (20% of cases);
- neurological complications (meningoencephalitis and cerebral venous thrombosis);
- digestive perforations.
The pathogenesis of coronary artery disease in Behçet’s disease is explained by thrombosis coronary. The thrombogenic risk of Behçet’s disease is currently known. His pathological substratum is leukocytoclastic vasculitis may cause stenosis, thrombosis or false aneurysms1. A thrombotic coronary arteritis has been demonstrated in some autopsy cases2,3. Orem et al. showed that in these patients the levels of lipoprotein Lp (a) is often high predisposing to develop thromboembolism complications4. The coagulation disorders have been implicated with the increase of fibrinogen, decreased fibrinolytic activity, lack of local activation of fibrinolysis.
Spasm has been implicated especially as the coronary arteries were previously injured (leukocytoclastic vasculitis). In the majority of cases the use of colchicine, corticosteroids and immunosuppressants was needed for other clinical manifestations of the disease. With a therapeutic-based calcium channel blockers to prevent coronary spasm5.
Gullu et al.6 showed silent ischemia detected by systematic thallium scintigraphy in 25% of patients investigated with Behcet’s scalable. This percentage is greater than in the control group (2.6%) so the primary prevention of complications of coronary artery disease in
Behcet’s still discussed.
Conclusion
Cardiac involvement in behcet disease remains underdiagnosed in the absence of cardiac signs and remains a poor prognosis for the patient, a test of myocardial ischemia should probably be associated with other cardiac systematic explorations.
Acknowledgments: None.
Disclosures: The authors declare that there is no conflict of interest.
References:
1. Huong DLT, Wechsler B, Kahn JC, Benhamou E, F Cajfinger, Godeau P and all. Myocardial infarction in Behçet’s disease. Arch. Evil. Heart. 1987 (11): 1663-7.
2. BayraktarY, Balkanci F, Kansu E, Dundar S, Uzunalimoglu B, Kayhan B, et al. Cavernous transformation of the portal vein: a common
manifestation of Behçet’s disease. Am J Gastroenterol.1998, 90: 1476-9.
3. Laklanpal S, Tani K, Lie JT, Katoh K, Ishigatsubo Y, Ohokubo T. and all: Pathologic features of Behçet’s syndrome: a review of Japanese
autopsy registry data. Hum Pathol. 1985 90: 1476-9.
4. Orem A, Dager O, O Memis, Bahadir S, O Ovali, Cimsit G. and all ,aLp (a) lipoprotein levels as a predictor of risk for thrombogenic events in
patients with Behçet’s disease. Ann Rheum Dis. 1995, 54: 726-9.
5. Brottier L, Barbier R, Bonnett J, Bricaud H. and all Myocardial infarction: unrecognized complication of Behcet’s disease. Sem Hosp Paris.
1987, 63: 2469-75.
6. Gullu IH, Benekli million Mudderisoglu H, Oto A, Kansu E, Kabakci G, et al. Silent myocardial ischemia in Behçet ‘disease. J Rheumatol. 1996, 23: 323-7.
 This work is licensed under a
This work is licensed under a