Vlad Vintila1,2, Vladimir Bratu2, Dragos Vinereanu1,2
1 „Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania
2 Department of Cardiology, Emergency University Hospital, Bucharest, Romania
Abstract: Gastrointestinal bleeding is the most frequent complication of dual antiplatelet therapy. We present the case of a 69-year-old patient who, 5 days after primary percutaneous coronary intervention, develops lower gastrointestinal bleeding with an important drop in hemoglobin that required discontinuation of dual antiplatelet therapy. He was diagnosed with colonic adenocarcinoma for which he underwent surgery one month after the acute coronary syndrome (due to high perioperative risk). The cancer was classified as T4bN2bM1a (stage IVa) and required adjuvant chemotherapy. After 6 rounds of chemotherapy the patient has good tolerance and is under strict clinical, echocardiographic and biohumoral surveillance. He is planned for an oncological follow-up after 6 months of chemotherapy. Gastrointestinal bleeding carries a poor prognosis after myocardial infarction and due to systolic disfunction and cardiac risk factors the patient is at high risk of developing chemotherapy-induced cardiotoxicity.
Keywords: gastrointestinal bleeding, antiplatelet therapy, myocardial infarction
INTRODUCTION
Gastrointestinal bleeding is the most frequent complication of dual antiplatelet therapy1. The management of these patients is a delicate one because of the need to carefully balance both the bleeding and thrombotic risks, an equilibrium that is frequently hard to achieve when faced with a malignant tumor.
CASE PRESENTATION
We present the case of a 69-year-old male, NM, that presented to the ER of the Bucharest University and Emergency Hospital with constrictive chest pain accompanied by shortness of breath and diaphoresis, with recent onset of about two hours. His medical history revealed that the patient had ESC/ESH stage III very high-risk hypertension, type 2 diabetes mellitus and he was a smoker for which he was taking Cande-sartan, Metformin and Gliclazide. The ER ECG strip showed sinus rhythm, QRS axis at + 10º, Q waves in V1 and V2 and ST elevation in V2-V5. The physical exam was fairly unremarkable, his BP was 147/68 mmHg, his heart rate was 85 bpm, his res-piratory rate was slightly elevated and his spontaneous SaO2 was 96%.
The diagnosis of Killip I anterior STEMI at 2 hours from onset was established and emergent coronary angiography was deemed necessary. A loading dose of double antiplatelet agents was given (250 mg acetylsalicylic acid and 180 mg ticagrelor). Coronary angiography revealed acute occlusion of the proximal LAD and a proximal critical stenosis of the ramus intermedius (Figure 1). Initially primary PCI of the LAD with a 3.5 x 24 mm DES was done followed by PCI of the ramus intermedius with a 3.5 x 14 mm DES with a good final result (Figure 2).
Immediately after the procedure he had a favorable course with resolution of anginal symptoms and no clinical signs of acute heart failure. His cardiac echo showed severe left ventricular systolic disfunction with a calculated LVEF of 27% and grade II ischaemic mitral regurgitation. His blood tests showed hypercholesterolemia with a LDL value of 173 mg/dl and a HbA1c value of 5.6 (adequately treated diabetes mellitus by means of oral antidiabetic drugs).
Standard treatment for STEMI patients was given: acetylsalicylic acid, ticagrelor, metoprolol succinate, candesartan (the patient had a history of persistent cough induced by ACE inhibitors), spironolactone, pantoprazole on top of metformin and gliclazide.
Despite the initial favorable course, 5 days after ad-mission the patient developed bloody stools with a significant Hb drop of 3.3 g/dl (down to a value of 10.2 g/dl). Emergency endoscopy could not identify the source of bleeding so, despite the high risk brought on by the recent myocardial infarction, a colonoscopy was deemed necessary. An ulcerated tumor with active bleeding was identified 20 cm from the anal orifice and a biopsy was done; the macroscopic appearance suggested colonic adenocarcinoma (Figure 3). Imaging workup was completed with a CT of the chest and abdomen that revealed, besides the tumoral mass, thickening of the pericolonic fat and multiple local adenopathies.
Considering the important drop in hemoglobin and the active bleeding at the tumor site we decided to stop dual antiplatelet therapy and continue with ticagrelor alone which led to symptom resolution. Regarding the therapeutic approach of the tumor we decided after consulting with the oncologist, surgeon and anesthesiologist to postpone any intervention up to a month considering the high risk regarding anesthesia and surgery in this particular patient.
His one-month follow up results (lack of symptoms, discrete rise in LVEF to a value of 35% and NTproBNP levels of 512 pg/ml) allowed us to refer the patient for surgery. During the surgical procedure local extension of the tumor with invasion of 3 ileal loops was noticed. Extensive local resection was needed followed by excision of the lymph nodes. The surgery was concluded with an ileostomy.
Pathology exam showed a moderately differentiated adenocarcinoma, without genetic criteria of microsatellite instability and the absence of KRAs gene mutation. TNM diagnosis was T4bN2bM1a and thus a stage IVa prognostic class was attributed. Dual antiplatelet therapy was restarted in the postsurgical setting.
Considering the advanced stage of the cancer, ad-juvant chemotherapy was needed. The patient was at high risk of developing chemotherapy induced cardio-toxicity, so it was decided to start a protocol consisting of oxaliplatin, 5-fluorouracil, folinic acid (FOLFOX 4 regimen) and cetuximab – an EGF inhibitor.
After 6 rounds of chemotherapy the patient has good clinical status, without overt signs of heart failure, without an additional drop in LVEF and steady values of biomarkers. He will undergo an oncological workup after 6 months of chemotherapy in order to decide the ensuing therapeutic approach.
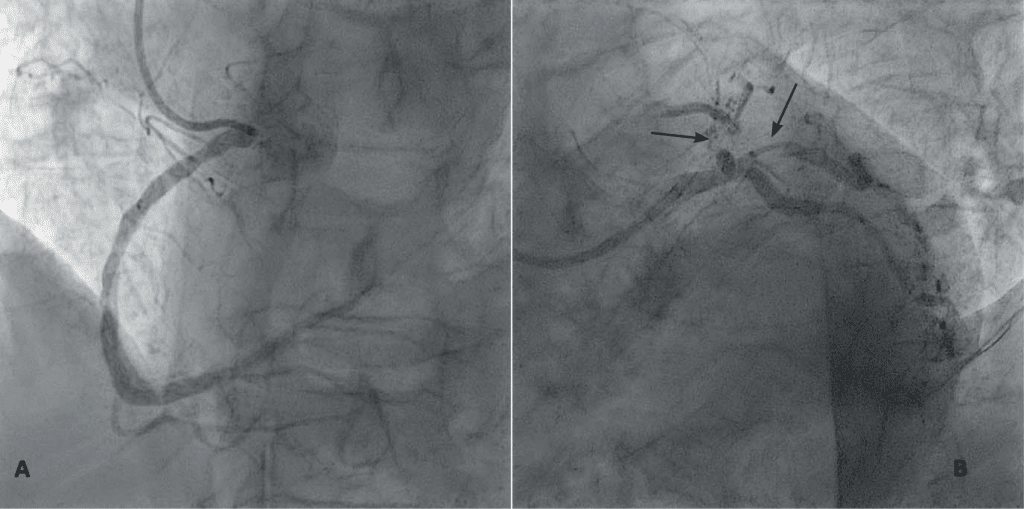
Figure 1. Coronary angiography. A. LAO cranial view; diffuse atherosclerotic disease of the right coronary artery . B. Acute thrombotic occlusion of the proximal left anterior descendign artery and a critical stenosis of the proximal ramus intermedius (arrows).
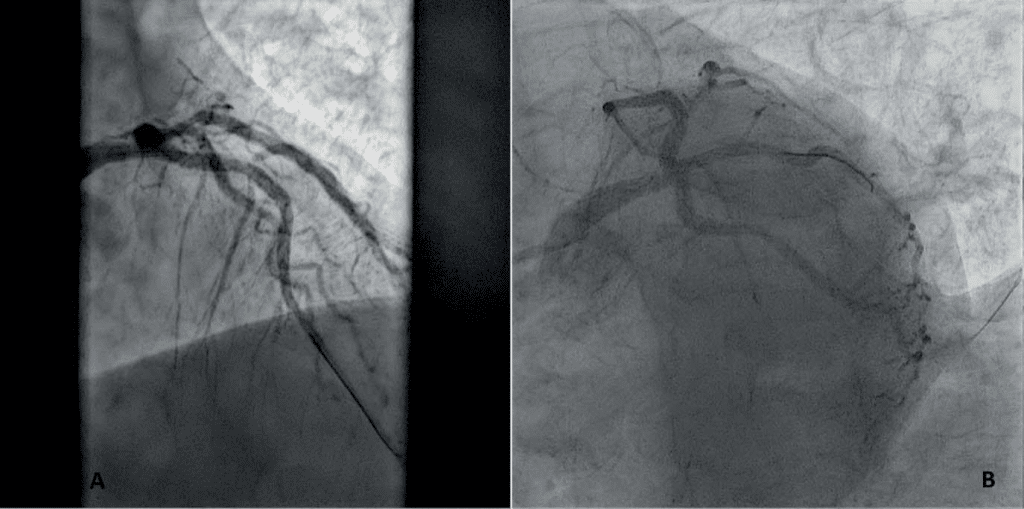
Figure 2. A. Final result of primary PCI of the left anterior descending artery – AP cranial view; the stent deployed in the proximal segment and TIMI 3 distal flow are visible. B. Final result of PCI of the ramus intermedius – LAO caudal view; the stent deployed in the proximal segment and TIMI 3 distal flow are visible.
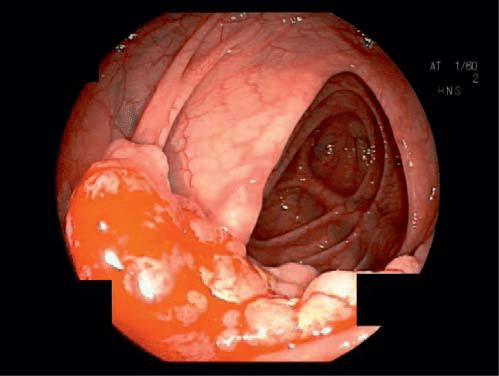
Figure 3. Ulcerated tumor with active bleeding stigmata located 20 cm from the anal orifice. (with permission of Dr. L. Negreanu – Gastroenterology Clinic, Bucharest Unversity Emergency Hospital).
DISCUSSIONS
Digestive bleeding entails an unfavorable prognosis in the case of patients with a recent acute coronary syndrome. Balancing the bleeding and thrombotic risk in this patient was hard to achieve because of the temporal proximity of the two events. Particular to this case, the finding of a malignant colonic tumor that requires adjuvant chemotherapy exposes the patient to additional risks of chemotherapy induced cardiotoxicity. The patient has moderate systolic disfunction and multiple risk factors that predate the moment of chemotherapy. The management of such patients re-quires strict clinical follow-up done by repeated echocardiography and repeated determination of biomarker levels (NTproBNP and troponin) to identify early any myocardial injury induced by chemotherapy.
Conflict of interest: none declared.
References
1. Agewall S, Cattaneo M, Collet JP, Andreotti F, Lip GY, Verheugt FW, Huber K, Grove EL, Morais J, Husted S, Wassmann S, Rosano G, Atar D, Pathak A, Kjeldsen K, Storey RF. Expert position paper on the use of proton pump inhibitors in patients with cardiovascular disease and antithrombotic therapy. Eur Heart J 2013;34:1708–1713, 1713a-1713b.
 This work is licensed under a
This work is licensed under a