Lelia Strimbu1,2, Ioana Dregoesc1, Radu Hagiu1
1 “Prof. Dr. C. C. Iliescu” Emergency Institute for Cadiovascular Diseases, Bucharest, Romania
2 ”Carol Davila”University of Medicine and Pharmacy, Bucharest, Romania
Abstract: Mediastinum is a complex area with lots of organs interconnected anatomically and functionally. The most common causes of anterior mediastinal mass include the following: thymoma; teratoma; thyroid disease; and lymphoma. Masses of the middle mediastinum are typically congenital cysts, including foregut and pericardial cysts, while those that arise in the posterior mediastinum are often neurogenic tumors1. Almost 4/5 of mediastinal tumors are benign, but the most highly risk of malignancies is for thymic tumors (up to 50%). Gold standard for mediastial tumor diagnosis is computerized tomography (CT) with or without intravenous (i.v.) contrast substance. We present you a case of a young caucasian man, recently diagnosticated with myastenia gravis, that had a CT scan and discovered a mediastinal tumor, probably a thymoma. Surprisingly in operation, the tumor was invasive, with a high tendency of bleeding, and probably malignant. A paliative operation was carried out, a prosthetic bypass from left venous brahiocefalic trunk to superior vena cava (SVC). The patient had an uneventful recovery period and was discharged after 7 days. The pathology finding was atypical lipomatous tumor, a liposarcoma. Invasive mediastinal tumors have a very poor prognosis, but this tumor located in mediastinum is very rare, so unfortunely aren’t many data about it, and estimated survival for this patient.
Keywords: mediastinal tumor, liposarcoma, atypical lipomatous tumor.
Abstract: Mediastinul reprezintă o zonă complexă ce cuprinde mai multe organe interconectate anatomic şi funcţional. Cele mai frecvente tipuri de tumori mediastinale sunt următoarele: timomul, teratomul, guşa tiroidiană multinodulară, limfomul. Tumorile din mediastinul mediu sunt, de obicei, chisturi congenitale, dezvoltate din canalul alimentar anterior (sistemul digestiv superior) şi din ţesut pericardic, în timp ce tumorile din mediastinul posterior sunt frecvent neurogenice.
Aproape 4 din 5 tumori mediastinale sunt benigne, dar cele timice au cel mai crescut risc de transformare malignă (până la 50%). Examenul computer tomograf (CT) cu sau fără substanţă de contrast intravenos reprezintă standardul “de aur” pentru diagnosticul tumorilor mediastinale. Vă prezentăm cazul unui pacient tânăr, caucazian, diagnosticat recent cu miastenia gravis, la care s-a evidenţiat o formaţiune la nivelul mediastinului anterior în urma examenului CT. Principala suspiciune a fost de timom. Surprinzător, intraoperator, tumora era invazivă, cu tendinţă la sângerare, probabil malignă. S-a efectuat o intervenţie paliativă, un by-pass de la nivelul trunchiului venos brahiocefalic stâng la vena cavă superioară (VCS) cu o proteză vasculară. Pacientul a evoluat favorabil postoperator şi a fost externat la 7 zile de la interventie. Diagnosticul anatomo-patologic a fost de tumoră lipomatoasă atipică, liposarcom. Tumorile mediastinale atipice au un prognostic rezervat, dar această tumoră localizată în mediastin este foarte rară. Aşa că, din păcate, nu există date suficiente despre această patologie, şi nu se poate estima supravieţuirea acestui pacient.
Cuvinte cheie: tumoră mediastinală, liposarcom, tumoră lipomatoasă atipică
BACKGROUND
Mediastinum is a complex area with lots of organs interconnected anatomically and functionally. This area is limited anterior – by the sternum, posterior – the spinal column, laterally – the mediastinal pleura, inferiorlly – the diafragm, superior by a plan that crosses inferior to the clavicules.
Clinically we devided mediastinum in 4 compartments: by the plan that crosses between manubrium and sternal body in superior mediastinum (which contains proximal segment of tracheea, esofagus, the thymic gland, aortic arch, left and right brachiocefalic veins, nerves), and inferior mediastinum which is divided in 3: anterior (distal part of thymic gland, fat tissue, lymph nodes), medium (intrapericardial heart vessels, pericardium, the heart, tracheal byfurcation, pulmonary arteries and veins, lymph nodes), and posterior (esofagus, thoracic descending aorta, thoracic duct, sympathetic and parasympathetic nerves, lymph nodes).
Mediastinal tumors classification
The most common causes of anterior mediastinal mass include the following: thymoma; teratoma; thyroid disease; and lymphoma. Masses of the middle mediastinum are typically congenital cysts, including foregut and pericardial cysts, while those that arise in the posterior mediastinum are often neurogenic tumors1,2.
Symptoms
Patients with mediastinal tumors can have specific clinical findings, depending on organ compresion or invasion, but frequently is not specific. Up to 50% of mediastinal tumors are diagnosticated accidentaly on a chest radiography, or investigating other disease2.
Diagnosis
A standard chest radiography can show enlargement of mediastinal opacity1,3. This enlargement can have different caracteristics depending on the tumor, a profile chest radiography is mandatory so we can see in which mediastinal compartement is the tumor. „Gold” standard is CT scan and can provide essential informations (toughness, surrounding tissue invasion, density); i.v. contrast is necessary for tissue necrosis, diferentiating vascular structures from surounding tissues, different changes in vascular walls (invasion, compresion). Lymph nodes can easily be identified and analized. CT scan is also very useful for guiding future invasive investigations (video assisted thoracoscopy-VATS, thoracic puncture, byopsy). I 131 scintigraphy is indicated for intrathoracic thyroid tumor2,4,5.
Byopsy invasive tests are very usefull, but have limited indicationd due to their important risks. Some of them are: mediastinoscopy, transthoracic byopsy aspiration, ultrasound or CT guided fine needle byopsy, VATS)6.
Cystic tumors with neurogenic tumors are the most frequently mediastinal tumors (up to 70%), then endocrine tumors (thymic and thyroid tumors), mesodermal tumors (lipomas, fibromas, sarcomas). Almost 4/5 of mediastinal tumors are benign, but the most highly risk of malignancies is for thymic tumors (up to 50%). Most of mediastinal tumors have a slow growth rate. The tumors in anterior mediastinum frequently are thymic, up to 20% in the adults, and most of them are diagnosed accidentally. Rarely patients have also myasthenia gravis, low Gama globulins, medullary aplasia, especially for red line, and some other immune problems2,4,6.
CASE REPORT
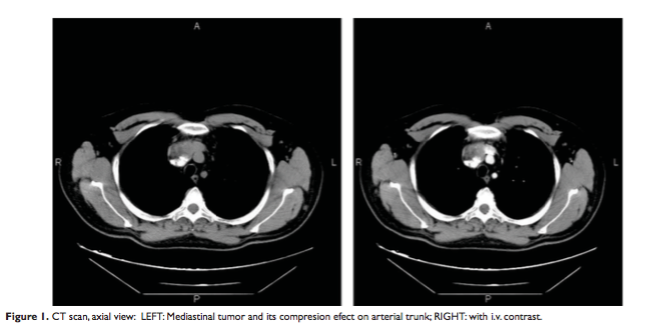
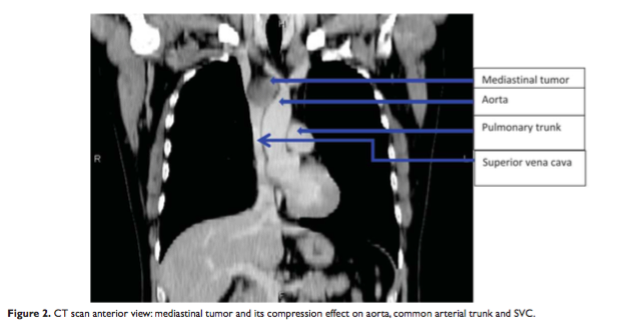
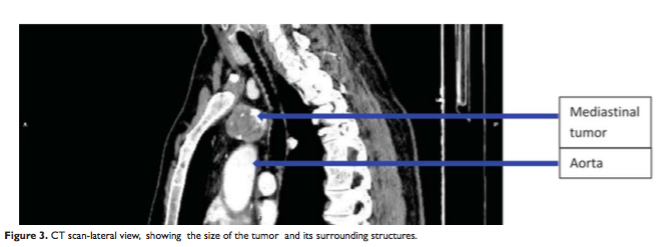
A 28-year old man, diagnosed recently with myasthenia gravis, had a CT scan and discovered a mediastinal tumor, probably a thymoma (Figure 1). The tumor was large (7/5 cm), located in the anterior and superior mediastinum, anterior of aorta and pulmonary trunk, but included innominate vein and was anterior to superior vena cava (SVC) (Figure 2). CT scan revealed non homogeneous nodular tumor at the anterosuperior mediastinum with compression effect on adjacent vascular structures, without invasiveness (Figure 3).
Also two small nodular lesions in the left upper lung lobe were found.
Physical examination was in normal parameters. There were no pathologic findings in echocardiography or radiography scan. Blood tests were normal. He was scheduled for operation.
The chest was opened through median sternotomy. Anterior of SVC, aorta and pulmonary trunk it was a large mass, of 7/5 cm wide, that included venous trunks at their confluence, and distal part of SVC. The tumor had a high consistency. A tumor fragment was excised and sent to Pathology. A serious tendency for bleeding was noticed, the tumor had important vascularization. Considering the age of the patient, the tendency for bleeding and the
malignant aspect of the tumor, we decided not to excise any more of it and to make a venous-venous by pass from left venous trunk to proximal SVC.
The venous by-pass was made with a vascular Gore-Tex prosthesis no 8. This was made in knowledge of the poor prognosis and natural history of the disease, considering the state of the tumor invading already vascular structures. Sternoraphy was made using Ti-Cron 5 sutures.
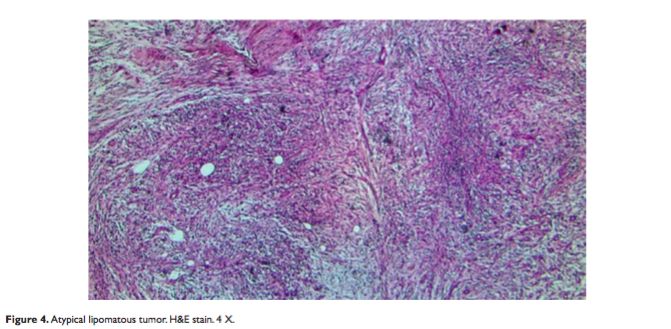
Light microscopy examination showed a tumor growth made of spindle cells with large, elongated, hyper chromatic nuclei, embedded in a myxoid and fibrillar collagen matrix.
A moderate inflammatory infiltrate was identified within the lesion. Note the presence of areas of bone differentiation (heterologous differentiation).
Immunohistochemistry study showed: S100 positive in tumoral cells, CD34 positive in vessels and stromal cells, SMA and Desmin positive in vascular walls, CD45 positive in inflammatory infiltrate, Ki-67 positive 1-3%.
CK7 and AE1/3 markers were negative. Histopathology and immunohistochemistry tests confirmed the diagnosis of differentiated liposarcoma (atypical lipomatous tumor).
Patient had an uneventful recovery, stayed 3 days in ICU (intensive care unit) and was discharged 7 days after surgical intervention. He was sent to Oncology Department for additional medical treatment.
CONCLUSION
Considering the low incidence of this type of tumor in mediastinum, less than 1%, the world wide experience with this rare, but seriously disease is limited3,4. Surgical excision of the tumor is the optimal treatment for a mediastinal liposarcoma, as in other sites. If the entire tumor cannot be excised, surgical debulking often results in symptomatic relief. Radiotherapy and chemotherapy may be added as adjuncts to surgical excision but liposarcoma seem to have low sensitivity2,5,6. Recurrence is common in deep-seated liposarcoma and it becomes detectable within the first 6 months in most cases, but it may be delayed for 5 or 10 years following the initial excision. Recurrence is directly related to the incomplete excision, tumor tissue left behind and invasiveness of the tumor in adjacent blood vessels, at the time of surgery. Therefore a close follow up is strongly recommended5-7.
Conflict of interest: none declared.
References
1. David H. Spodick, Chapter 50 Pericardial Diseases, Heart Disease: A Textbook of Cardiovascular Medicine, 6th ed, Eds: Eugene Braunwald, Douglas P. Zipes, Peter Libby, W.B. Saunders London, 2001, 1858-1859.
2. Beau V. Duwe, Daniel H. Sterman, Ali I. Musani, Tumors of the Mediastinum, Chest 128(4):2005, 2893-2905.
3. Kirklin, Barratt-Boyes, Nicholas T. Kouchoukos, Eugene H. Blackstone, Frank L. Hanley, James K. Kirklin, Chapter 18 – Cardiac tumor, Cardiac Surgery, Morphology, Diagnostic Criteria, Natural History, Techniques, Results, and Indications, Vol.1, Fourth Edition, Elsevier Saunders, 2013, 750.
4. Lawrence H.Cohn, Jon-Cecil M.Walkes,W. Roy Smythe, Michael J. Reardon, Chapter 63 Cardiac Neoplasms, Cardiac surgery in the adult, Third edition, The McGraw-Hill, 2008, 1500-1501.
5. Park DR, Vallieres E, Tumors and cysts of the mediastinum. Chapter 76, Textbook of Respiratory Medicine. 5th eds. Mason RJ, Broaddus VC, Martin TR, King TE, Schraufnagel DE, Murray JF and Nadel JA, Philadelphia, Elsevier Saunders; 2010, 1814-1835.
6. Takenori Mase. Nobuhiko Kawawaki, Chihiro Narumiya, Takahiko Aoyama, Shinji Kato, Yoshihisa Nagata, Primary liposarcoma of the mediastinum, The Japanese Journal of Thoracic and Cardiovascular Surgery, June 2002, Volume 50, Issue 6, 252-255.
7. Nikolaos Barbetakis, Georgios Samanidis, Elpida Samanidou, Efthimios Kirodimos, Anastasia Kiziridou, Theodoros Bischiniotis, Christodoulos Tsilikas, Primary mediastinal liposarcoma: a case report, Journal of Medical Case Reports 2007, 161.
 This work is licensed under a
This work is licensed under a